Sunday Poster Session
Category: Liver
P1773 - Abdominal Abscess Post-Splenic Embolization in a Patient With Decompensated Cirrhosis
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall

Christopher E. Potts, BS
Marshall University Joan C. Edwards School of Medicine
Huntington, WV
Presenting Author(s)
Christopher E. Potts, BS, Alexander G. Burbelo, BS, Mohamed L. Hammad, MD, Ahmed M. Sherif, MD, Wesam Frandah, MD, Mujtaba Mohamed, MD
Marshall University Joan C. Edwards School of Medicine, Huntington, WV
Introduction: Partial splenic embolization (PSE) is a minimally invasive treatment option for patients with cirrhosis-related thrombocytopenia where splenectomy carries significant risks. PSE is known to be associated with complications such as infarction, abscess formation, and portal vein thrombosis. We present a case of intra-abdominal abscess formation following PSC in a patient with advanced liver disease.
Case Description/
Methods: A 44-year-old male with decompensated cirrhosis secondary to Hepatitis C and IV drug use, complicated by esophageal varices, underwent elective PSE in January and February 2025 to address hypersplenism-related pancytopenia. The patient initially tolerated treatment well, but returned weeks later with worsening abdominal pain, distension, and dyspnea. Despite intervention with broad-spectrum antibiotics and multiple paracenteses, neutrophilia and symptoms of spontaneous bacterial peritonitis (SBP) persisted while ascitic fluid remained culture negative.
One month later, the patient presented again with similar symptoms of increased severity and signs of systemic inflammation. Computed Tomography imaging revealed a sizable intra-abdominal fluid collection containing gas inclusions, consistent with abscess formation. Treatment was initiated with empirical IV antibiotics and interventional radiology (IR) was consulted to perform percutaneous drainage. Although the patient remained culture-negative, 16S rRNA PCR testing identified Robinsonella peoriensis, a rare bacterium found in humans. The patient progressed well with treatment, was discharged with a drain in place, and advised to follow up with IR and infectious disease.
Discussion: Intra-abdominal abscess formation following PSE is a rare but serious complication in immunocompromised patients with advanced liver disease. In our experience, differentiating SBP and abscess formation can be quite challenging, especially when culture-negative ascitic fluid neutrophilia persists. Importantly, culture-negative results and suspected treatment-resistant SBP do not rule out infection. Molecular analysis using 16S rRNA sequencing is of invaluable diagnostic importance, and timely IR-guided drainage and pharmacologic therapy was crucial for the recovery of this patient.
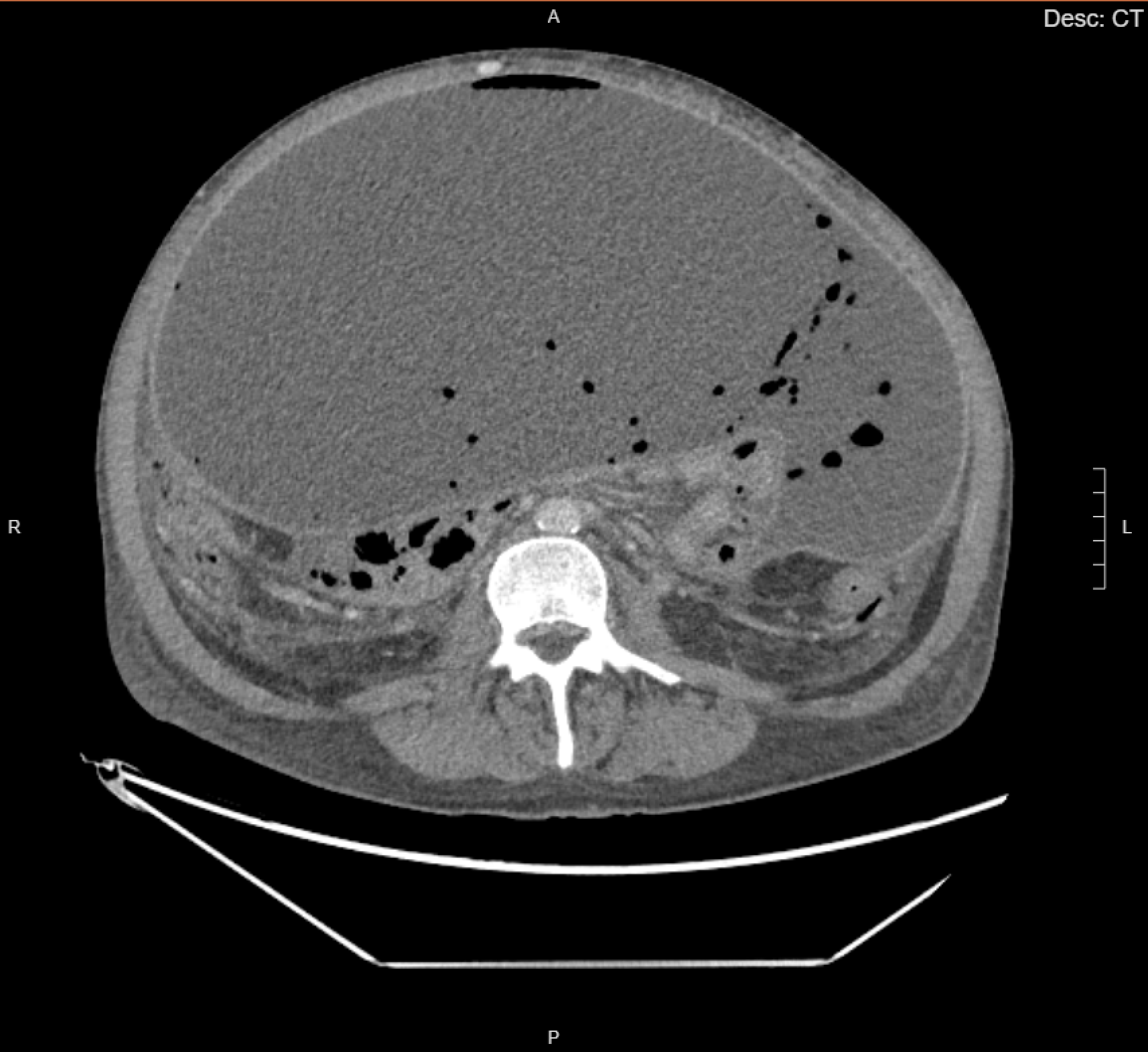
Figure: Transverse section of a contrast-enhanced CT of the abdomen demonstrating a large intra-abdominal fluid collection with gaseous inclusions, consistent with abscess formation.

Figure: X-ray Angiography during the first partial splenic embolization procedure shows catheter placement within the splenic artery and embolization of distal arterial branches.
Disclosures:
Christopher Potts indicated no relevant financial relationships.
Alexander Burbelo indicated no relevant financial relationships.
Mohamed Hammad indicated no relevant financial relationships.
Ahmed Sherif indicated no relevant financial relationships.
Wesam Frandah: Boston Scientific – Advisor or Review Panel Member, Consultant. Merritt – Consultant. Olympus corporation of America – Consultant.
Mujtaba Mohamed indicated no relevant financial relationships.
Christopher E. Potts, BS, Alexander G. Burbelo, BS, Mohamed L. Hammad, MD, Ahmed M. Sherif, MD, Wesam Frandah, MD, Mujtaba Mohamed, MD. P1773 - Abdominal Abscess Post-Splenic Embolization in a Patient With Decompensated Cirrhosis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
Marshall University Joan C. Edwards School of Medicine, Huntington, WV
Introduction: Partial splenic embolization (PSE) is a minimally invasive treatment option for patients with cirrhosis-related thrombocytopenia where splenectomy carries significant risks. PSE is known to be associated with complications such as infarction, abscess formation, and portal vein thrombosis. We present a case of intra-abdominal abscess formation following PSC in a patient with advanced liver disease.
Case Description/
Methods: A 44-year-old male with decompensated cirrhosis secondary to Hepatitis C and IV drug use, complicated by esophageal varices, underwent elective PSE in January and February 2025 to address hypersplenism-related pancytopenia. The patient initially tolerated treatment well, but returned weeks later with worsening abdominal pain, distension, and dyspnea. Despite intervention with broad-spectrum antibiotics and multiple paracenteses, neutrophilia and symptoms of spontaneous bacterial peritonitis (SBP) persisted while ascitic fluid remained culture negative.
One month later, the patient presented again with similar symptoms of increased severity and signs of systemic inflammation. Computed Tomography imaging revealed a sizable intra-abdominal fluid collection containing gas inclusions, consistent with abscess formation. Treatment was initiated with empirical IV antibiotics and interventional radiology (IR) was consulted to perform percutaneous drainage. Although the patient remained culture-negative, 16S rRNA PCR testing identified Robinsonella peoriensis, a rare bacterium found in humans. The patient progressed well with treatment, was discharged with a drain in place, and advised to follow up with IR and infectious disease.
Discussion: Intra-abdominal abscess formation following PSE is a rare but serious complication in immunocompromised patients with advanced liver disease. In our experience, differentiating SBP and abscess formation can be quite challenging, especially when culture-negative ascitic fluid neutrophilia persists. Importantly, culture-negative results and suspected treatment-resistant SBP do not rule out infection. Molecular analysis using 16S rRNA sequencing is of invaluable diagnostic importance, and timely IR-guided drainage and pharmacologic therapy was crucial for the recovery of this patient.
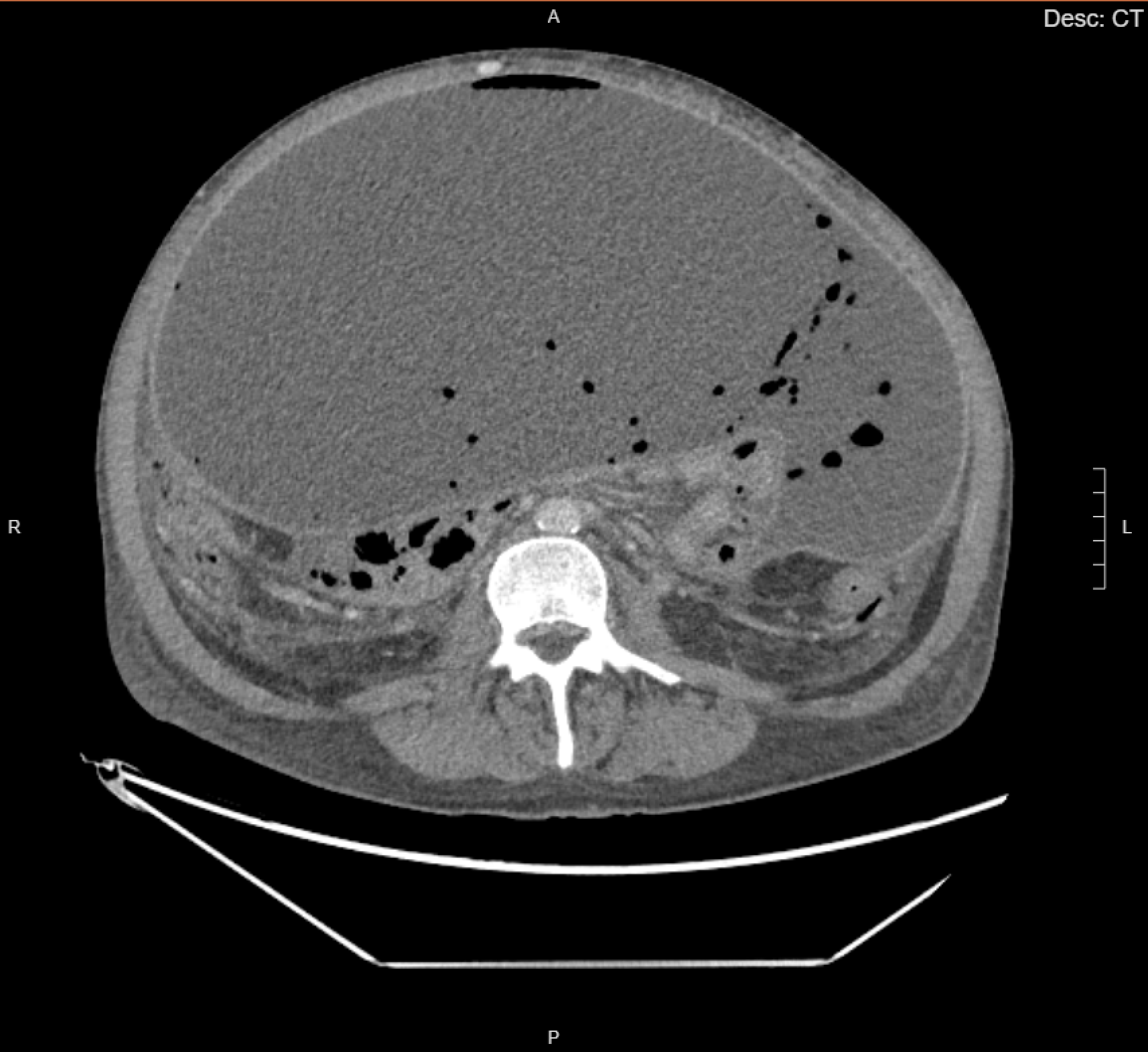
Figure: Transverse section of a contrast-enhanced CT of the abdomen demonstrating a large intra-abdominal fluid collection with gaseous inclusions, consistent with abscess formation.

Figure: X-ray Angiography during the first partial splenic embolization procedure shows catheter placement within the splenic artery and embolization of distal arterial branches.
Disclosures:
Christopher Potts indicated no relevant financial relationships.
Alexander Burbelo indicated no relevant financial relationships.
Mohamed Hammad indicated no relevant financial relationships.
Ahmed Sherif indicated no relevant financial relationships.
Wesam Frandah: Boston Scientific – Advisor or Review Panel Member, Consultant. Merritt – Consultant. Olympus corporation of America – Consultant.
Mujtaba Mohamed indicated no relevant financial relationships.
Christopher E. Potts, BS, Alexander G. Burbelo, BS, Mohamed L. Hammad, MD, Ahmed M. Sherif, MD, Wesam Frandah, MD, Mujtaba Mohamed, MD. P1773 - Abdominal Abscess Post-Splenic Embolization in a Patient With Decompensated Cirrhosis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
