Sunday Poster Session
Category: IBD
P1248 - Plot Twist: Neuroendocrine Tumor in a Patient With Ileal Pouch-Anal Anastomosis
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall
- PR
Prajith Raj Ramesh, MBBS
University of South Dakota
Sioux Falls, SD
Presenting Author(s)
Prajith Raj Ramesh, MBBS1, Victor Chedid, MD, MSc2, Siri A. Urquhart, MD2
1University of South Dakota, Sioux Falls, SD; 2Mayo Clinic, Rochester, MN
Introduction: Neoplasia of the ileoanal pouch is uncommon, reported to occur in fewer than 1% of patients. Neuroendocrine tumors (NET) are rare neoplastic complications of the pouch and can present diagnostic challenges given the presence of overlapping symptoms with pouchitis or pouch disorders. We present a case of mixed poorly differentiated adenocarcinoma and NET arising in the ileoanal pouch of a patient with a history of ileal pouch-anal anastomosis (IPAA).
Case Description/
Methods: A 36-year-old male with a history of 2-stage IPAA for medically refractory ulcerative colitis complicated by Crohn’s-like disease of the pouch (on ustekinumab 90 mg SQ every 4 weeks) presented with abdominal pain. Imaging and pouchoscopy showed pre-pouch ileum inflammation with associated stricturing disease at the prior enteroenterostomy site and pouch inlet as well as fistulizing disease from the pre-pouch ileum and posterior pouch to the presacral space with abscess formation. He transitioned to combination therapy with infliximab and azathioprine.
Due to refractory disease and pouch dysfunction, he underwent pouch excision with end ileostomy. Pathology revealed a 1.8 cm mass consistent with mixed poorly differentiated adenocarcinoma and neuroendocrine carcinoma with positive immunostains for synaptophysin, chromogranin, and mucicarmine (Figure 1). Lymph nodes were negative, but surgical margin was involved by tumor. Postoperative complications included bowel obstruction requiring stricturoplasty and revision of ileostomy, wound dehiscence, and C. difficile infection.
PET-CT scan showed small FDG-avid mesenteric nodes and peritoneal nodules suspicious for metastases (Figure 2). Exploratory laparotomy with biopsy of peritoneum, omentum, and mesenteric nodules revealed fibroadipose tissue with fat necrosis and organizing abscess, but no malignancy. He remains under imaging surveillance per oncology.
Discussion: NETs of the ileoanal pouch are rare, but histologically similar to other gastrointestinal NETs, staining positive for chromogranin and synaptophysin. Most are nonfunctional, but may present with symptoms of obstruction, bleeding, or hormonal secretion. Diagnosis is made histologically, often during surveillance pouchoscopy or investigation of refractory symptoms. Management includes surgical resection for localized disease and systemic therapy for advanced cases. This case underscores the importance of considering neoplastic processes, including NETs, in patients with persistent or atypical pouch symptoms.
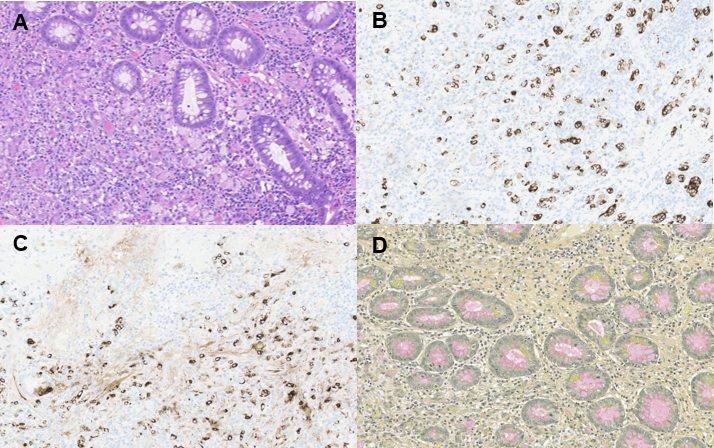
Figure: Figure 1. Representative hematoxyclin and eosin (A) histology image (10X) demonstrating mixed poorly differentiated adenocarcinoma and neuroendocrine carcinoma with positive immunostains for synaptophysin (B) and chromogranin (C). Mucicarmine stain (D) demonstrating presence of signet ring cells. Pathologic stage I (pT1, pN0, cM0), histologic grade 3, and residual tumor (R) R1 (microscopic).
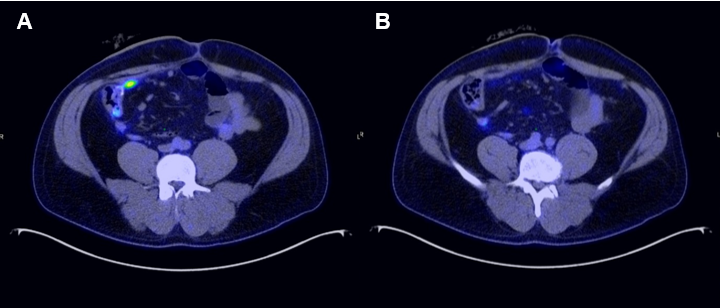
Figure: Figure 2. PET-CT with a small FDG-avid abdominal soft tissue nodule subjacent to the right anterior abdominal wall (A) and prominent node in central mesentery (B) suspicious for metastasis.
Disclosures:
Prajith Raj Ramesh indicated no relevant financial relationships.
Victor Chedid: Pfizer – Grant/Research Support. Takeda – Consultant.
Siri Urquhart indicated no relevant financial relationships.
Prajith Raj Ramesh, MBBS1, Victor Chedid, MD, MSc2, Siri A. Urquhart, MD2. P1248 - Plot Twist: Neuroendocrine Tumor in a Patient With Ileal Pouch-Anal Anastomosis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1University of South Dakota, Sioux Falls, SD; 2Mayo Clinic, Rochester, MN
Introduction: Neoplasia of the ileoanal pouch is uncommon, reported to occur in fewer than 1% of patients. Neuroendocrine tumors (NET) are rare neoplastic complications of the pouch and can present diagnostic challenges given the presence of overlapping symptoms with pouchitis or pouch disorders. We present a case of mixed poorly differentiated adenocarcinoma and NET arising in the ileoanal pouch of a patient with a history of ileal pouch-anal anastomosis (IPAA).
Case Description/
Methods: A 36-year-old male with a history of 2-stage IPAA for medically refractory ulcerative colitis complicated by Crohn’s-like disease of the pouch (on ustekinumab 90 mg SQ every 4 weeks) presented with abdominal pain. Imaging and pouchoscopy showed pre-pouch ileum inflammation with associated stricturing disease at the prior enteroenterostomy site and pouch inlet as well as fistulizing disease from the pre-pouch ileum and posterior pouch to the presacral space with abscess formation. He transitioned to combination therapy with infliximab and azathioprine.
Due to refractory disease and pouch dysfunction, he underwent pouch excision with end ileostomy. Pathology revealed a 1.8 cm mass consistent with mixed poorly differentiated adenocarcinoma and neuroendocrine carcinoma with positive immunostains for synaptophysin, chromogranin, and mucicarmine (Figure 1). Lymph nodes were negative, but surgical margin was involved by tumor. Postoperative complications included bowel obstruction requiring stricturoplasty and revision of ileostomy, wound dehiscence, and C. difficile infection.
PET-CT scan showed small FDG-avid mesenteric nodes and peritoneal nodules suspicious for metastases (Figure 2). Exploratory laparotomy with biopsy of peritoneum, omentum, and mesenteric nodules revealed fibroadipose tissue with fat necrosis and organizing abscess, but no malignancy. He remains under imaging surveillance per oncology.
Discussion: NETs of the ileoanal pouch are rare, but histologically similar to other gastrointestinal NETs, staining positive for chromogranin and synaptophysin. Most are nonfunctional, but may present with symptoms of obstruction, bleeding, or hormonal secretion. Diagnosis is made histologically, often during surveillance pouchoscopy or investigation of refractory symptoms. Management includes surgical resection for localized disease and systemic therapy for advanced cases. This case underscores the importance of considering neoplastic processes, including NETs, in patients with persistent or atypical pouch symptoms.
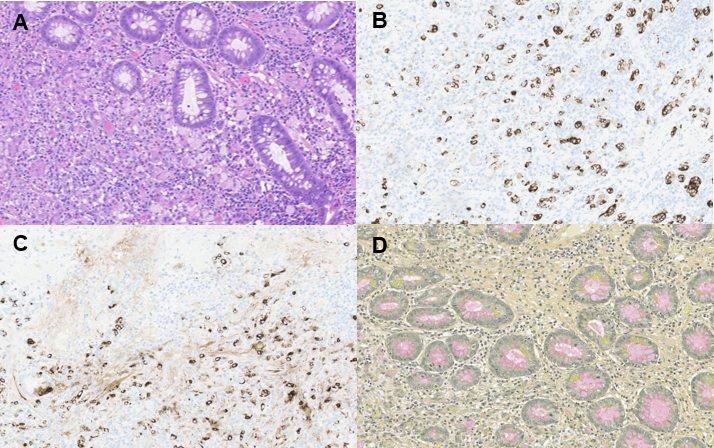
Figure: Figure 1. Representative hematoxyclin and eosin (A) histology image (10X) demonstrating mixed poorly differentiated adenocarcinoma and neuroendocrine carcinoma with positive immunostains for synaptophysin (B) and chromogranin (C). Mucicarmine stain (D) demonstrating presence of signet ring cells. Pathologic stage I (pT1, pN0, cM0), histologic grade 3, and residual tumor (R) R1 (microscopic).
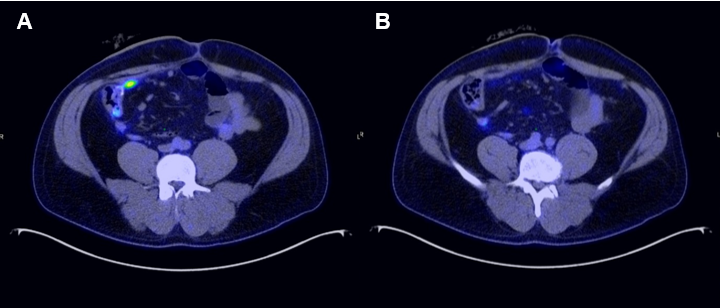
Figure: Figure 2. PET-CT with a small FDG-avid abdominal soft tissue nodule subjacent to the right anterior abdominal wall (A) and prominent node in central mesentery (B) suspicious for metastasis.
Disclosures:
Prajith Raj Ramesh indicated no relevant financial relationships.
Victor Chedid: Pfizer – Grant/Research Support. Takeda – Consultant.
Siri Urquhart indicated no relevant financial relationships.
Prajith Raj Ramesh, MBBS1, Victor Chedid, MD, MSc2, Siri A. Urquhart, MD2. P1248 - Plot Twist: Neuroendocrine Tumor in a Patient With Ileal Pouch-Anal Anastomosis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
