Sunday Poster Session
Category: Biliary/Pancreas
P0059 - Comparative Efficacy of Steroid-Sparing Agents in Preventing Relapse in Autoimmune Pancreatitis: A Systematic Review and Meta-Analysis
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall
- EA
Emre Adalier
University of Pavia, Faculty of Medicine
Pavia, Lombardia, Italy
Presenting Author(s)
Emre Adalier, 1, Gautam Maddineni, MD2, Nur Barlas, MD3, Sait Barlas, MD3, Ingridy Sodre, 1, Nicola Khoury, 1, Oğuzhan Şal, MD4, Bhaumik Brahmbhatt, MBBS, MD5
1University of Pavia, Faculty of Medicine, Pavia, Lombardia, Italy; 2MD, Cape Coral, FL; 3Florida State University- Lee Health, Cape Coral, FL; 4İstanbul University İstanbul Faculty of Medicine, Istanbul, Istanbul, Turkey; 5Mayo Clinic, Jacksonville, FL
Introduction: Autoimmune pancreatitis (AIP) is a rare, steroid-responsive form of chronic pancreatitis. While glucocorticoids induce remission effectively, relapse after tapering or withdrawal is common, prompting interest in maintenance strategies that minimize long-term steroid exposure. Steroid-sparing agents (SSAs) such as azathioprine, mycophenolate mofetil, methotrexate, and rituximab are increasingly used in clinical practice, yet their comparative efficacy remains uncertain. We conducted a systematic review and meta-analysis to evaluate whether SSAs reduce relapse risk and improve sustained remission compared to steroid monotherapy or no maintenance therapy in patients with AIP.
Methods: We systematically searched PubMed, Scopus, and the Cochrane Library through April 2025 for studies evaluating SSAs in AIP patients with ≥12 months of follow-up. Eligible studies compared SSAs (azathioprine, methotrexate, mycophenolate mofetil, or rituximab) to steroid monotherapy or withdrawal. The primary outcome was relapse; the secondary outcome was sustained remission. Pooled risk ratios (RRs) and 95% confidence intervals (CIs) were calculated using a random-effects model. Heterogeneity was assessed using the I² statistic. A predefined subgroup analysis compared rituximab to azathioprine or methotrexate.
Results: Three studies (n=298) met inclusion criteria. SSAs did not significantly reduce relapse risk compared to no maintenance therapy (RR 0.89, 95% CI 0.37–2.11, p=0.78; I²=74%), nor did they significantly improve sustained remission overall (RR 1.11, 95% CI 0.78–1.57, p=0.58; I²=71%). However, in subgroup analysis, rituximab was associated with significantly higher sustained remission compared to azathioprine or methotrexate (RR 0.71, 95% CI 0.51–0.98, p=0.04). Heterogeneity was moderate to high, reflecting variability in study design, definitions of relapse, and treatment regimens.
Discussion: While steroid-sparing agents did not demonstrate a statistically significant benefit in preventing relapse or achieving sustained remission overall, rituximab showed potential superiority over conventional immunomodulators. The small number of studies and substantial heterogeneity limit the strength of conclusions. Our findings highlight the need for larger, prospective, head-to-head trials to determine optimal AIP maintenance therapy and better define which patients may benefit most from targeted immunosuppressive approaches.
AI-assisted language editing was used; all content was authored by investigators.
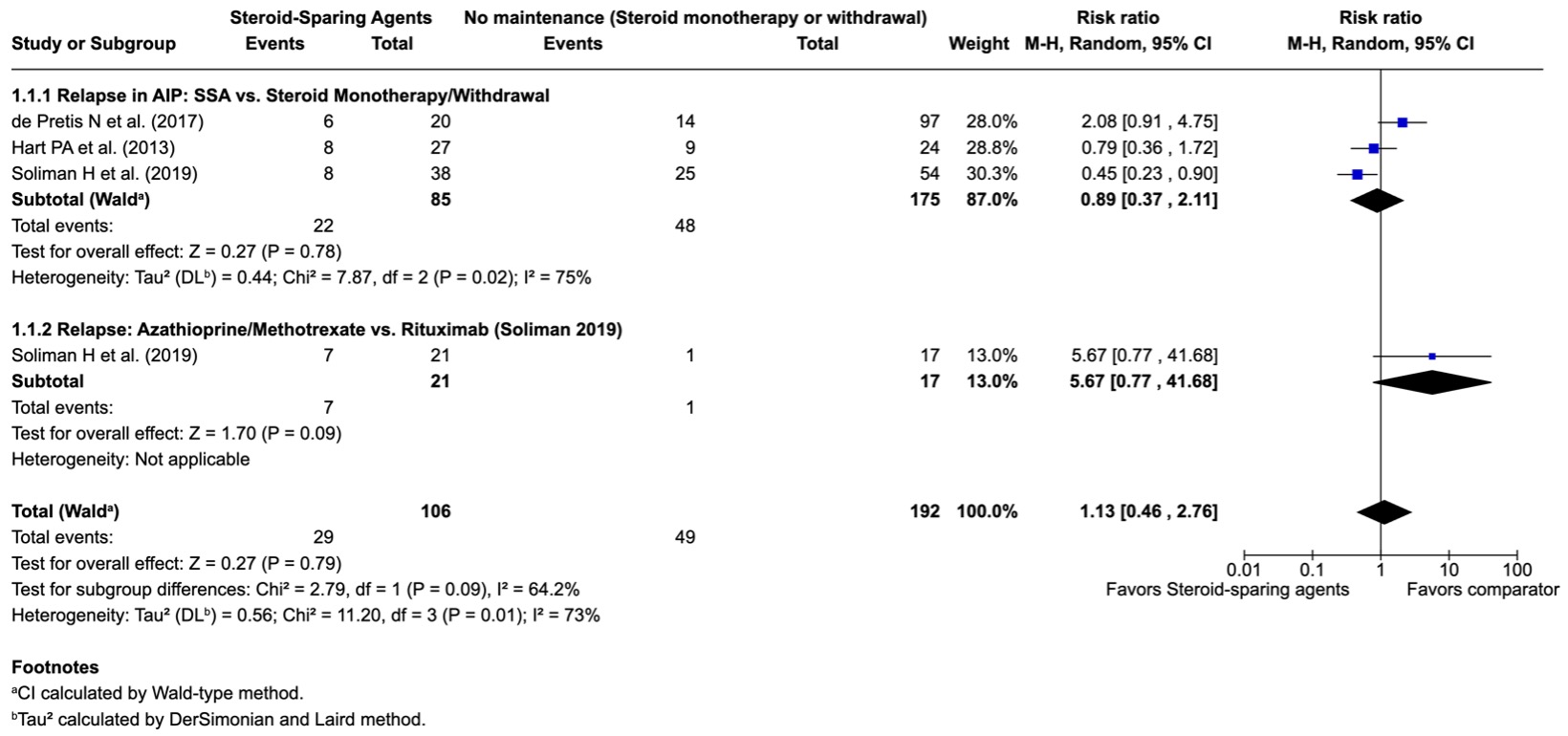
Figure: Forest plot comparing relapse rates in autoimmune pancreatitis patients receiving steroid-sparing agents (azathioprine, mycophenolate mofetil, rituximab) versus steroid monotherapy or no maintenance.
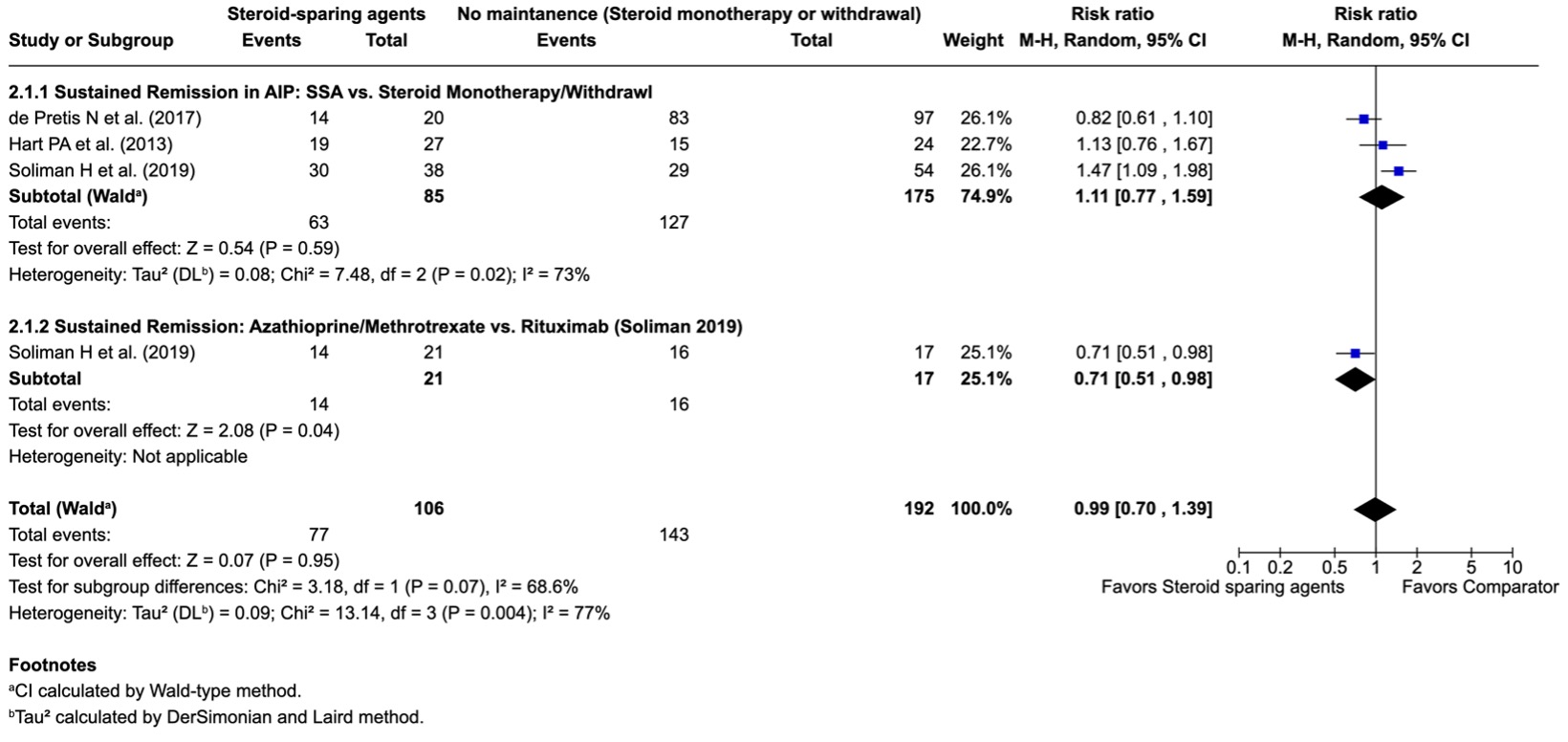
Figure: Forest plot comparing sustained remission in autoimmune pancreatitis patients.
Disclosures:
Emre Adalier indicated no relevant financial relationships.
Gautam Maddineni indicated no relevant financial relationships.
Nur Barlas indicated no relevant financial relationships.
Sait Barlas indicated no relevant financial relationships.
Ingridy Sodre indicated no relevant financial relationships.
Nicola Khoury indicated no relevant financial relationships.
Oğuzhan Şal indicated no relevant financial relationships.
Bhaumik Brahmbhatt indicated no relevant financial relationships.
Emre Adalier, 1, Gautam Maddineni, MD2, Nur Barlas, MD3, Sait Barlas, MD3, Ingridy Sodre, 1, Nicola Khoury, 1, Oğuzhan Şal, MD4, Bhaumik Brahmbhatt, MBBS, MD5. P0059 - Comparative Efficacy of Steroid-Sparing Agents in Preventing Relapse in Autoimmune Pancreatitis: A Systematic Review and Meta-Analysis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1University of Pavia, Faculty of Medicine, Pavia, Lombardia, Italy; 2MD, Cape Coral, FL; 3Florida State University- Lee Health, Cape Coral, FL; 4İstanbul University İstanbul Faculty of Medicine, Istanbul, Istanbul, Turkey; 5Mayo Clinic, Jacksonville, FL
Introduction: Autoimmune pancreatitis (AIP) is a rare, steroid-responsive form of chronic pancreatitis. While glucocorticoids induce remission effectively, relapse after tapering or withdrawal is common, prompting interest in maintenance strategies that minimize long-term steroid exposure. Steroid-sparing agents (SSAs) such as azathioprine, mycophenolate mofetil, methotrexate, and rituximab are increasingly used in clinical practice, yet their comparative efficacy remains uncertain. We conducted a systematic review and meta-analysis to evaluate whether SSAs reduce relapse risk and improve sustained remission compared to steroid monotherapy or no maintenance therapy in patients with AIP.
Methods: We systematically searched PubMed, Scopus, and the Cochrane Library through April 2025 for studies evaluating SSAs in AIP patients with ≥12 months of follow-up. Eligible studies compared SSAs (azathioprine, methotrexate, mycophenolate mofetil, or rituximab) to steroid monotherapy or withdrawal. The primary outcome was relapse; the secondary outcome was sustained remission. Pooled risk ratios (RRs) and 95% confidence intervals (CIs) were calculated using a random-effects model. Heterogeneity was assessed using the I² statistic. A predefined subgroup analysis compared rituximab to azathioprine or methotrexate.
Results: Three studies (n=298) met inclusion criteria. SSAs did not significantly reduce relapse risk compared to no maintenance therapy (RR 0.89, 95% CI 0.37–2.11, p=0.78; I²=74%), nor did they significantly improve sustained remission overall (RR 1.11, 95% CI 0.78–1.57, p=0.58; I²=71%). However, in subgroup analysis, rituximab was associated with significantly higher sustained remission compared to azathioprine or methotrexate (RR 0.71, 95% CI 0.51–0.98, p=0.04). Heterogeneity was moderate to high, reflecting variability in study design, definitions of relapse, and treatment regimens.
Discussion: While steroid-sparing agents did not demonstrate a statistically significant benefit in preventing relapse or achieving sustained remission overall, rituximab showed potential superiority over conventional immunomodulators. The small number of studies and substantial heterogeneity limit the strength of conclusions. Our findings highlight the need for larger, prospective, head-to-head trials to determine optimal AIP maintenance therapy and better define which patients may benefit most from targeted immunosuppressive approaches.
AI-assisted language editing was used; all content was authored by investigators.
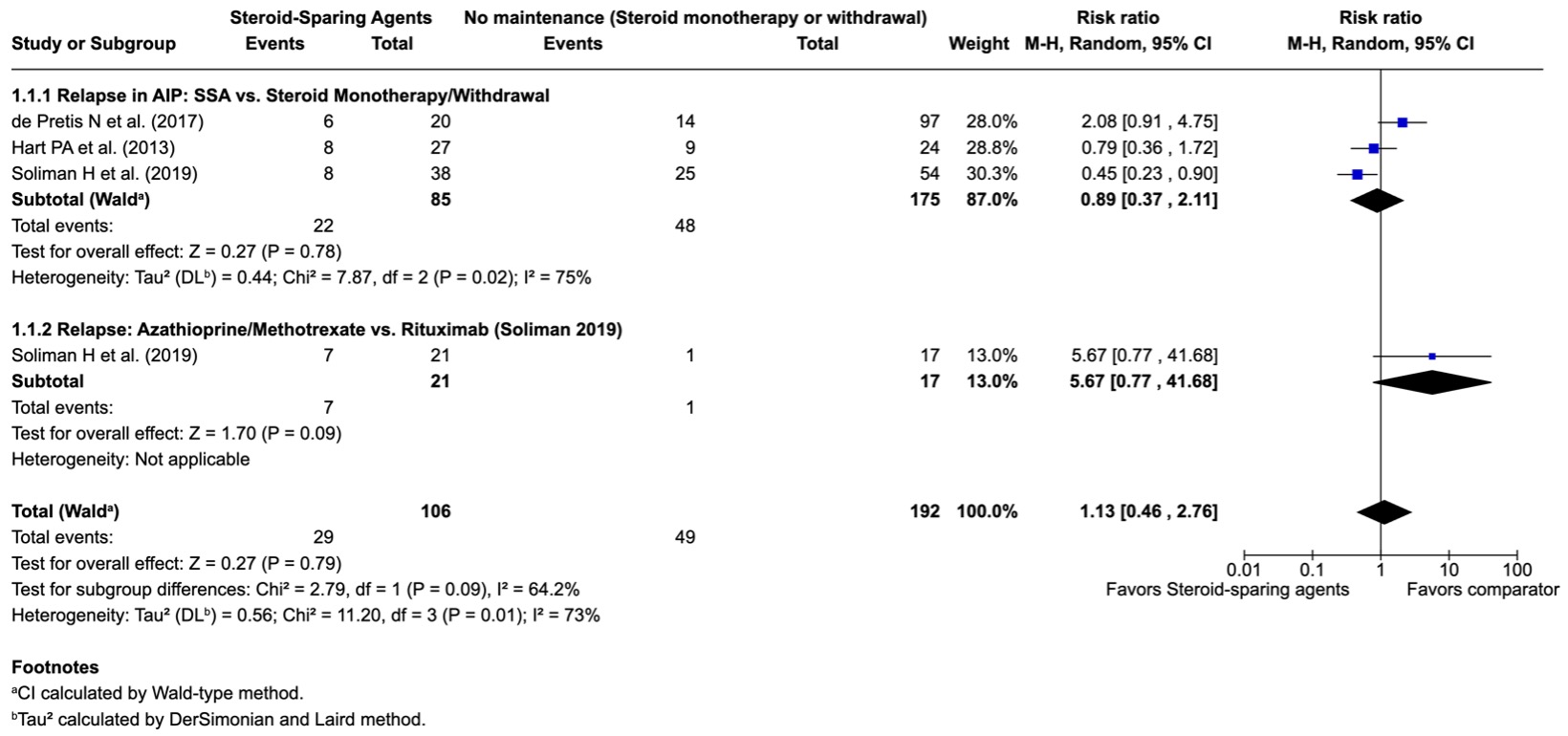
Figure: Forest plot comparing relapse rates in autoimmune pancreatitis patients receiving steroid-sparing agents (azathioprine, mycophenolate mofetil, rituximab) versus steroid monotherapy or no maintenance.
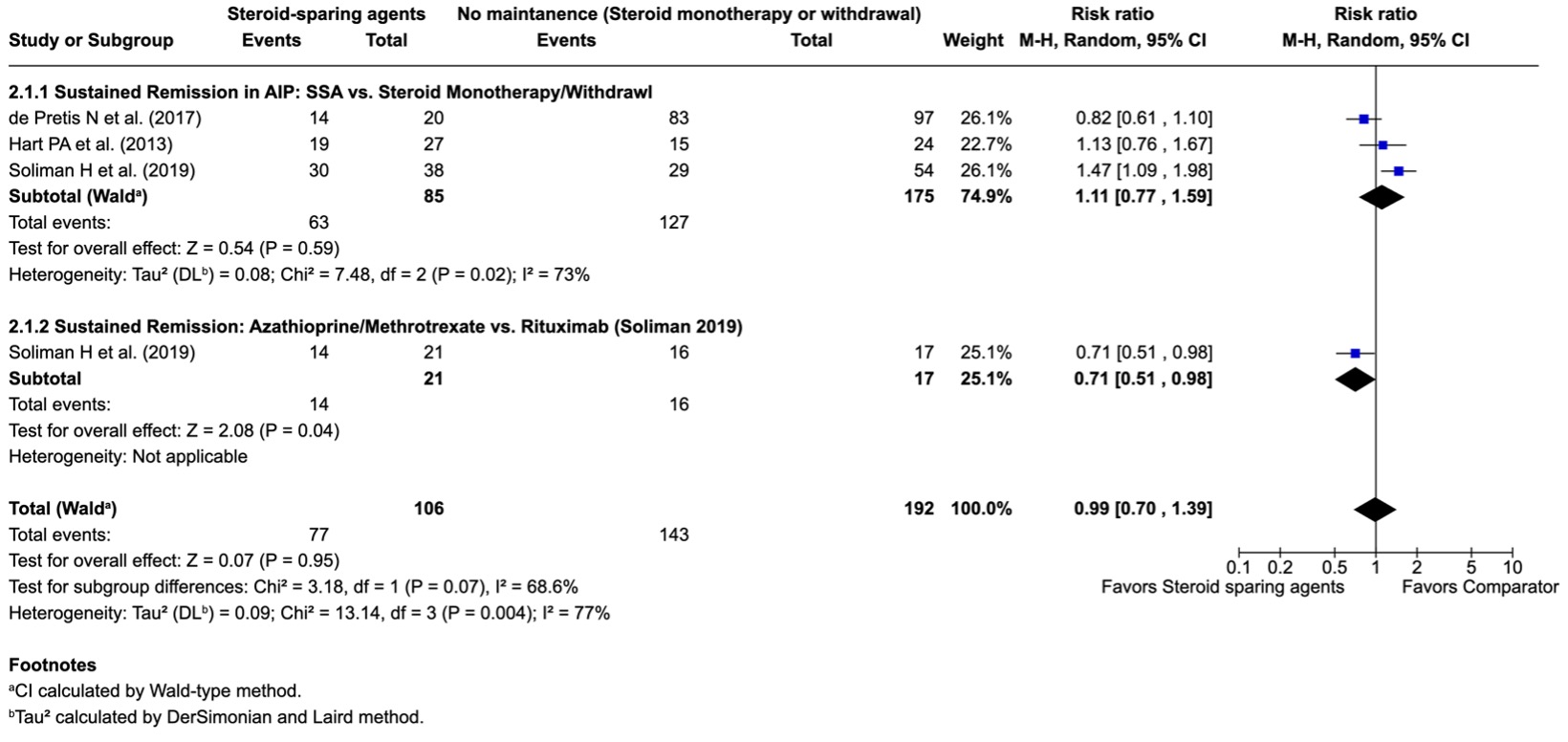
Figure: Forest plot comparing sustained remission in autoimmune pancreatitis patients.
Disclosures:
Emre Adalier indicated no relevant financial relationships.
Gautam Maddineni indicated no relevant financial relationships.
Nur Barlas indicated no relevant financial relationships.
Sait Barlas indicated no relevant financial relationships.
Ingridy Sodre indicated no relevant financial relationships.
Nicola Khoury indicated no relevant financial relationships.
Oğuzhan Şal indicated no relevant financial relationships.
Bhaumik Brahmbhatt indicated no relevant financial relationships.
Emre Adalier, 1, Gautam Maddineni, MD2, Nur Barlas, MD3, Sait Barlas, MD3, Ingridy Sodre, 1, Nicola Khoury, 1, Oğuzhan Şal, MD4, Bhaumik Brahmbhatt, MBBS, MD5. P0059 - Comparative Efficacy of Steroid-Sparing Agents in Preventing Relapse in Autoimmune Pancreatitis: A Systematic Review and Meta-Analysis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
