Sunday Poster Session
Category: Biliary/Pancreas
P0056 - The Hidden Gap: Pancreatitis Outcomes in Native Americans in Northern Arizona
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall

Jin Yun, DO (she/her/hers)
Providence Portland Medical Center
Portland, OR
Presenting Author(s)
Afsheen Moshtaghi, DO1, Jin Yun, DO2, Hamza Khan, MD1, Hady Shahbaz, BS3, Lauritta Fowler, BS1, Neychelle Rocca, MD1
1Northern Arizona Health, Cottonwood, AZ; 2Providence Portland Medical Center, Portland, OR; 3Midwestern University, Glendale, AZ
Introduction: While prior studies have investigated racial and ethnic disparities in pancreatitis, data remains sparse for Native American populations, who may be uniquely affected by socioeconomic and geographic factors. This study aims to evaluate the disproportionate outcomes of acute pancreatitis in Native Americans compared to the general population in the same region.
Methods: We conducted a retrospective cohort study of hospitalized patients diagnosed with acute pancreatitis at two community hospitals in Northern Arizona. A total of 1,113 patients hospitalized between 1/2023 and 8/2024 were included, comprising 413 Native American patients and 700 patients of other racial backgrounds (White, Black, Hispanic, Asian, Multiracial). The cause of pancreatitis was categorized as alcohol-induced, biliary-induced, unspecified, or other (including idiopathic, drug-induced, and cyst-related causes). Outcomes such as hospital length of stay, discharge disposition, and in-hospital mortality were analyzed.
Results: Among 1,113 pancreatitis-related hospitalizations, 37.1% were Native American and 62.9% were of other racial backgrounds. The etiology of pancreatitis significantly differed between Native American and other racial groups (p < 0.001) seen in Figure 1. Native American patients had a markedly higher proportion of alcohol-induced pancreatitis (56.4%) compared to other patients (26.2%). Conversely, biliary-induced pancreatitis was more common in the other group (21.0% vs 5.6%). The proportion of cases attributed to unspecified or other causes did not differ as sharply between groups. Discharge disposition patterns showed that most patients in both groups were discharged home. However, Native American patients had a higher rate of in-hospital mortality (3.9% vs. 2.9%) and fewer hospice discharges (0.5% vs. 2.1%). Additionally, 17 Native American patients (4.1%) and 1 patient in the other group (0.1%) left the hospital against medical advice.
Discussion: Native American patients had a markedly higher proportion of alcohol-induced pancreatitis compared to other racial groups. Trends showed Native American patients experienced higher inpatient mortality rates, increased instances of elopement, and fewer hospice referrals. These findings suggest a disproportionate burden of alcohol-related pancreatitis among Native American patients and highlight the need for targeted public health interventions and culturally sensitive preventive strategies.
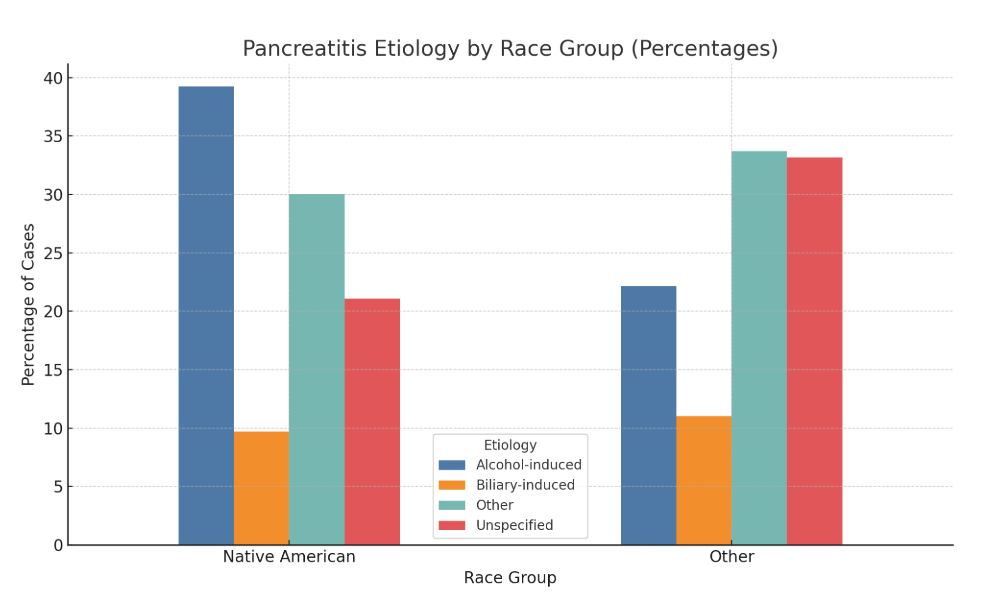
Figure: Figure 1: The etiology of acute pancreatitis found in Native American individuals compared to other racial groups.
Disclosures:
Afsheen Moshtaghi indicated no relevant financial relationships.
Jin Yun indicated no relevant financial relationships.
Hamza Khan indicated no relevant financial relationships.
Hady Shahbaz indicated no relevant financial relationships.
Lauritta Fowler indicated no relevant financial relationships.
Neychelle Rocca indicated no relevant financial relationships.
Afsheen Moshtaghi, DO1, Jin Yun, DO2, Hamza Khan, MD1, Hady Shahbaz, BS3, Lauritta Fowler, BS1, Neychelle Rocca, MD1. P0056 - The Hidden Gap: Pancreatitis Outcomes in Native Americans in Northern Arizona, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Northern Arizona Health, Cottonwood, AZ; 2Providence Portland Medical Center, Portland, OR; 3Midwestern University, Glendale, AZ
Introduction: While prior studies have investigated racial and ethnic disparities in pancreatitis, data remains sparse for Native American populations, who may be uniquely affected by socioeconomic and geographic factors. This study aims to evaluate the disproportionate outcomes of acute pancreatitis in Native Americans compared to the general population in the same region.
Methods: We conducted a retrospective cohort study of hospitalized patients diagnosed with acute pancreatitis at two community hospitals in Northern Arizona. A total of 1,113 patients hospitalized between 1/2023 and 8/2024 were included, comprising 413 Native American patients and 700 patients of other racial backgrounds (White, Black, Hispanic, Asian, Multiracial). The cause of pancreatitis was categorized as alcohol-induced, biliary-induced, unspecified, or other (including idiopathic, drug-induced, and cyst-related causes). Outcomes such as hospital length of stay, discharge disposition, and in-hospital mortality were analyzed.
Results: Among 1,113 pancreatitis-related hospitalizations, 37.1% were Native American and 62.9% were of other racial backgrounds. The etiology of pancreatitis significantly differed between Native American and other racial groups (p < 0.001) seen in Figure 1. Native American patients had a markedly higher proportion of alcohol-induced pancreatitis (56.4%) compared to other patients (26.2%). Conversely, biliary-induced pancreatitis was more common in the other group (21.0% vs 5.6%). The proportion of cases attributed to unspecified or other causes did not differ as sharply between groups. Discharge disposition patterns showed that most patients in both groups were discharged home. However, Native American patients had a higher rate of in-hospital mortality (3.9% vs. 2.9%) and fewer hospice discharges (0.5% vs. 2.1%). Additionally, 17 Native American patients (4.1%) and 1 patient in the other group (0.1%) left the hospital against medical advice.
Discussion: Native American patients had a markedly higher proportion of alcohol-induced pancreatitis compared to other racial groups. Trends showed Native American patients experienced higher inpatient mortality rates, increased instances of elopement, and fewer hospice referrals. These findings suggest a disproportionate burden of alcohol-related pancreatitis among Native American patients and highlight the need for targeted public health interventions and culturally sensitive preventive strategies.
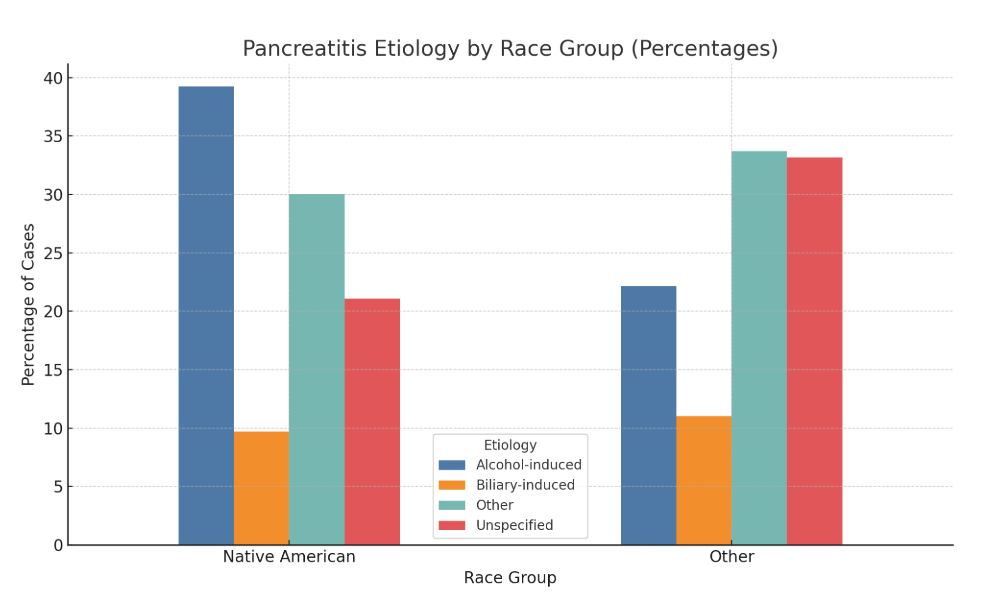
Figure: Figure 1: The etiology of acute pancreatitis found in Native American individuals compared to other racial groups.
Disclosures:
Afsheen Moshtaghi indicated no relevant financial relationships.
Jin Yun indicated no relevant financial relationships.
Hamza Khan indicated no relevant financial relationships.
Hady Shahbaz indicated no relevant financial relationships.
Lauritta Fowler indicated no relevant financial relationships.
Neychelle Rocca indicated no relevant financial relationships.
Afsheen Moshtaghi, DO1, Jin Yun, DO2, Hamza Khan, MD1, Hady Shahbaz, BS3, Lauritta Fowler, BS1, Neychelle Rocca, MD1. P0056 - The Hidden Gap: Pancreatitis Outcomes in Native Americans in Northern Arizona, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.

