Sunday Poster Session
Category: Biliary/Pancreas
P0137 - Acute Cholecystitis and Cholecystocolonic Fistula: Dual Rare Complications of Metal Stenting for Malignant Biliary Obstruction
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall

Raul A. Rios-De Choudens, MD
VA Caribbean Healthcare System, Puerto Rico
Presenting Author(s)
Stephanie Colon-Marrero, MD, Raul A. Rios-De Choudens, MD, Patricia Rivera-Carino, MD, Jose Martin-Ortiz, MD, FACG
VA Caribbean Healthcare System, San Juan, Puerto Rico
Introduction: Endoscopic retrograde cholangiopancreatography (ERCP) with biliary stenting is a cornerstone in the management of malignant biliary obstruction. While post-ERCP pancreatitis is the most common complication, acute cholecystitis and cholecystocolonic fistula (CCF) are rare but serious adverse effects. We present a case of both complications following metal stent placement for malignant pancreaticobiliary stricture.
Case Description/
Methods: A 65-year-old man with history of smoking presented with three months of postprandial epigastric pain and unintentional weight loss. CT imaging scan showed a 2.7 x 3 cm pancreatic head mass with ductal dilation and innumerable hepatic hypodensities concerning for metastases. Laboratories showed direct hyperbilirubinemia and cholestatic liver injury. Liver biopsy confirmed microsatellite-stable pancreatic adenocarcinoma. ERCP with sphincterotomy and placement of a fully covered self-expanding metal stent (SEMS) in the common bile duct, resulting in marked improvement of cholestasis (Figure 1). Three weeks later, the patient returned with fever, chills and poor oral intake. Despite normal bilirubin, laboratories were remarkable for neutrophilic leukocytosis. Imaging showed gallbladder distention, wall thickening, pericholecystic fluid. These findings were consistent with acute cholecystitis due to cystic duct obstruction by the SEMS for which percutaneous cholecystostomy (PCT) was placed. While initially improving, he subsequently developed diffuse abdominal pain and decreased PCT output. Follow-up imaging revealed a complex collection with fluid and gas which communicates with the hepatic flexure and extends to the anterior liver capsule, concerning for a CCF (Figure 2,3). Patient faced progressive clinical decline and was transitioned to hospice care.
Discussion: Acute cholecystitis occurs in 3.5-15% of patients after SEMS placement and is primarily due to cystic duct occlusion. Covered stents are particularly implicated given their expansile nature and risk of obstructing biliary side branches. CCF, on the other hand, is exceedingly rare and typically arise from chronic inflammation, necrosis or perforation the setting of obstruction or infection. Timely recognition of acute cholecystitis and prompt intervention with PCT can be lifesaving, but clinicians must also be alert to the possibility of evolving fistulous complications as these carry a grave prognosis.
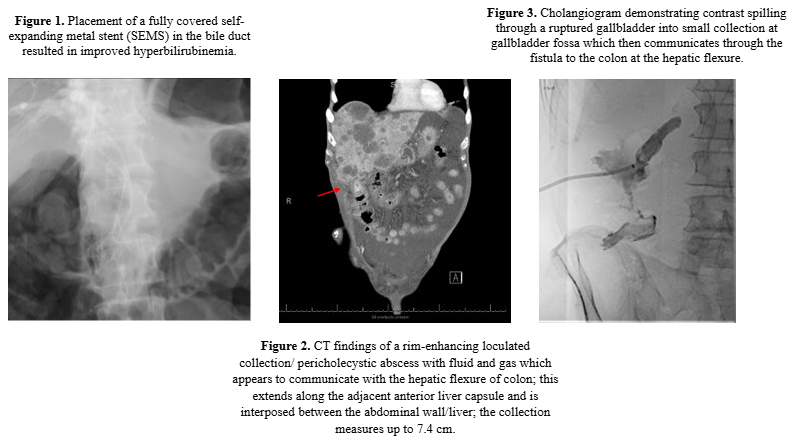
Figure: Acute Cholecystitis and Cholecystocolonic Fistula: Dual Rare Complications of Metal Stenting for Malignant Biliary Obstruction
Disclosures:
Stephanie Colon-Marrero indicated no relevant financial relationships.
Raul A. Rios-De Choudens indicated no relevant financial relationships.
Patricia Rivera-Carino indicated no relevant financial relationships.
Jose Martin-Ortiz indicated no relevant financial relationships.
Stephanie Colon-Marrero, MD, Raul A. Rios-De Choudens, MD, Patricia Rivera-Carino, MD, Jose Martin-Ortiz, MD, FACG. P0137 - Acute Cholecystitis and Cholecystocolonic Fistula: Dual Rare Complications of Metal Stenting for Malignant Biliary Obstruction, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
VA Caribbean Healthcare System, San Juan, Puerto Rico
Introduction: Endoscopic retrograde cholangiopancreatography (ERCP) with biliary stenting is a cornerstone in the management of malignant biliary obstruction. While post-ERCP pancreatitis is the most common complication, acute cholecystitis and cholecystocolonic fistula (CCF) are rare but serious adverse effects. We present a case of both complications following metal stent placement for malignant pancreaticobiliary stricture.
Case Description/
Methods: A 65-year-old man with history of smoking presented with three months of postprandial epigastric pain and unintentional weight loss. CT imaging scan showed a 2.7 x 3 cm pancreatic head mass with ductal dilation and innumerable hepatic hypodensities concerning for metastases. Laboratories showed direct hyperbilirubinemia and cholestatic liver injury. Liver biopsy confirmed microsatellite-stable pancreatic adenocarcinoma. ERCP with sphincterotomy and placement of a fully covered self-expanding metal stent (SEMS) in the common bile duct, resulting in marked improvement of cholestasis (Figure 1). Three weeks later, the patient returned with fever, chills and poor oral intake. Despite normal bilirubin, laboratories were remarkable for neutrophilic leukocytosis. Imaging showed gallbladder distention, wall thickening, pericholecystic fluid. These findings were consistent with acute cholecystitis due to cystic duct obstruction by the SEMS for which percutaneous cholecystostomy (PCT) was placed. While initially improving, he subsequently developed diffuse abdominal pain and decreased PCT output. Follow-up imaging revealed a complex collection with fluid and gas which communicates with the hepatic flexure and extends to the anterior liver capsule, concerning for a CCF (Figure 2,3). Patient faced progressive clinical decline and was transitioned to hospice care.
Discussion: Acute cholecystitis occurs in 3.5-15% of patients after SEMS placement and is primarily due to cystic duct occlusion. Covered stents are particularly implicated given their expansile nature and risk of obstructing biliary side branches. CCF, on the other hand, is exceedingly rare and typically arise from chronic inflammation, necrosis or perforation the setting of obstruction or infection. Timely recognition of acute cholecystitis and prompt intervention with PCT can be lifesaving, but clinicians must also be alert to the possibility of evolving fistulous complications as these carry a grave prognosis.
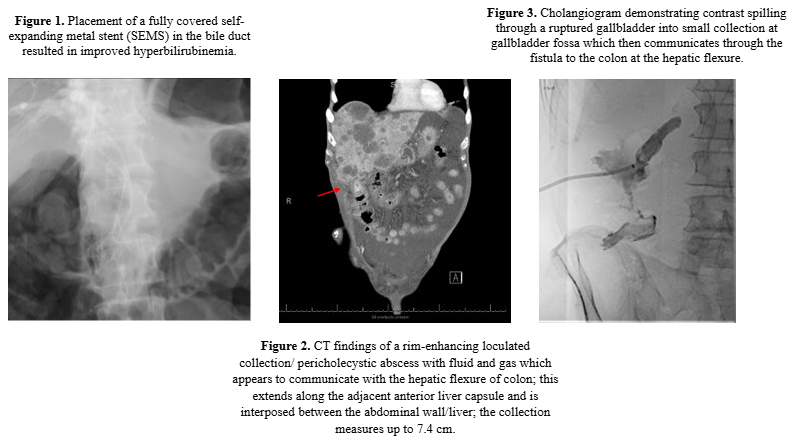
Figure: Acute Cholecystitis and Cholecystocolonic Fistula: Dual Rare Complications of Metal Stenting for Malignant Biliary Obstruction
Disclosures:
Stephanie Colon-Marrero indicated no relevant financial relationships.
Raul A. Rios-De Choudens indicated no relevant financial relationships.
Patricia Rivera-Carino indicated no relevant financial relationships.
Jose Martin-Ortiz indicated no relevant financial relationships.
Stephanie Colon-Marrero, MD, Raul A. Rios-De Choudens, MD, Patricia Rivera-Carino, MD, Jose Martin-Ortiz, MD, FACG. P0137 - Acute Cholecystitis and Cholecystocolonic Fistula: Dual Rare Complications of Metal Stenting for Malignant Biliary Obstruction, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
