Sunday Poster Session
Category: Biliary/Pancreas
P0126 - Clinical Judgment Guides Multidisciplinary Care: Rare Invasive IOPN with Concurrent Neuroendocrine Tumor Despite Initial Benign Sampling
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall

Kelly Fan, MD (she/her/hers)
SSM Health Saint Louis University Hospital
St. Louis, MO
Presenting Author(s)
Kelly Fan, MD, Nancy Phillips, MD, Danielle Carpenter, MD, Isra N. Taha, MD, Marina Kim, DO
SSM Health Saint Louis University Hospital, St. Louis, MO
Introduction: Intraductal oncocytic papillary neoplasms (IOPN) are rare pancreatic neoplasms that have recently been recognized as a separate entity from other intraductal papillary mucinous neoplasms (IPMNs). This is the case of a patient who presented with a large, symptomatic pancreatic head mass who was found to have an intraductal papillary neoplasm, likely IOPN, and concomitant pancreatic neuroendocrine tumor (NET).
Case Description/
Methods: A 76-year-old woman with gastroesophageal reflux disease and obesity presented to the hospital with nausea, vomiting, reflux, weight loss, and dyspnea for several months.
On admission, labs showed hemoglobin 5.2 g/dL and elevation of alkaline phosphatase, AST ALT and total bilirubin. Computed tomography (CT) revealed a 5.7 x 4.8 cm mass in the pancreatic head and uncinate process. Magnetic resonance imaging (MRI) with magnetic resonance cholangiopancreatography (MRCP) showed the mass obstructing the pancreatic duct and common bile duct (CBD) with CBD dilation.
Endoscopic ultrasound (EUS) revealed a 55mm x 52mm actively bleeding pancreatic head mass abutting the portal vein and infiltrating the duodenum (Fig. A). Fine needle biopsy (FNB) revealed superficial fragments of papillary neoplasm without signs of invasive malignancy. CA 19-9 and CEA were elevated at 262.4 U/mL and 98.2 ng/mL, respectively. Endoscopic retrograde cholangiopancreatography (ERCP) was unsuccessful due to inability to identify the major papilla within the duodenal extension of the mass. Thus, a percutaneous drain was placed to relieve the biliary obstruction. Repeat EUS with biopsy showed superficial fragments of low-grade papillary neoplasm without evidence of invasive malignancy, suggesting either IAPN or IPMN (Fig. B). Following multidisciplinary discussions, the decision to undergo pancreaticoduodenectomy was made due to large tumor size, abuttal of the superior mesenteric vein (SMV), and concern for invasive malignancy not captured with FNB. Pathology from pancreatoduodenectomy revealed intraductal papillary neoplasm (5.1 cm) with associated invasive carcinoma with histologic features most compatible with IOPN, with a very small incidental well differentiated pancreatic NET (0.5 cm).
Discussion: It is rare for intraductal papillary neoplasms to invade the duodenum. Further, there are few reports of concomitant IPMNs and NETs; even less is reported on concomitant IOPNs and NETs. This case exemplifies the importance of multidisciplinary efforts in management of pancreatic tumors.
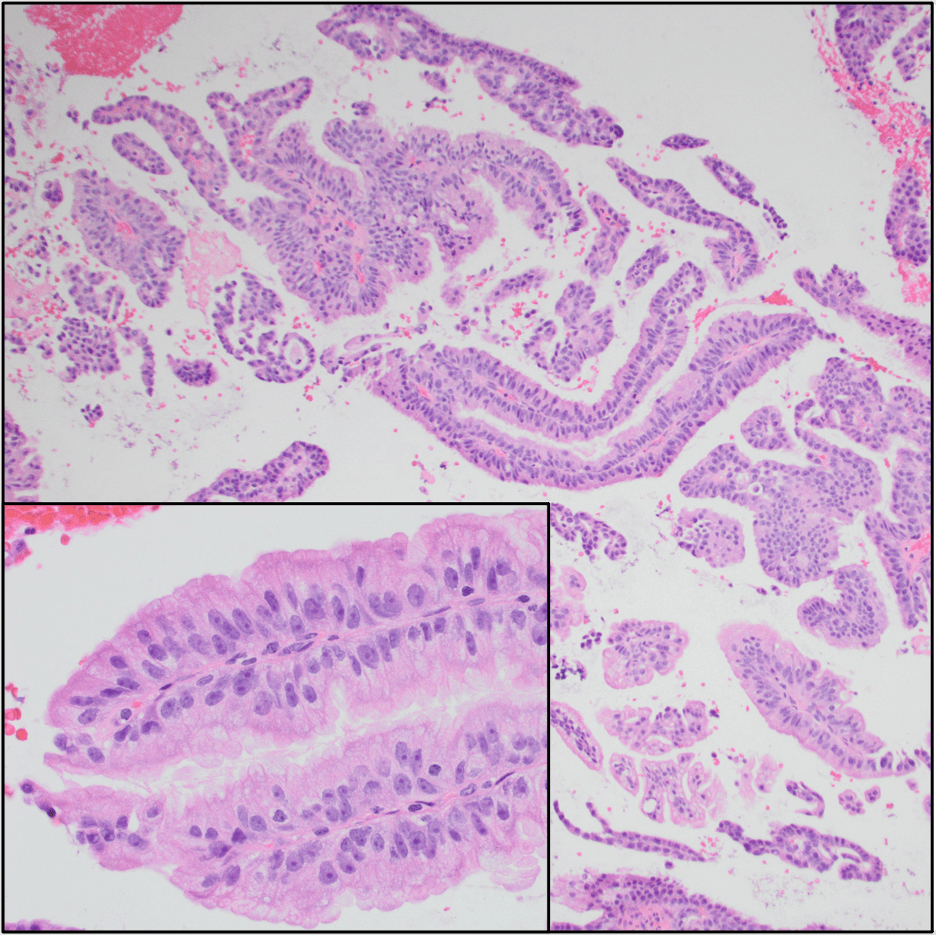
Figure: Figure A. Upper endoscopy revealing a large, infiltrating, actively oozing mass in the area of the major papilla.
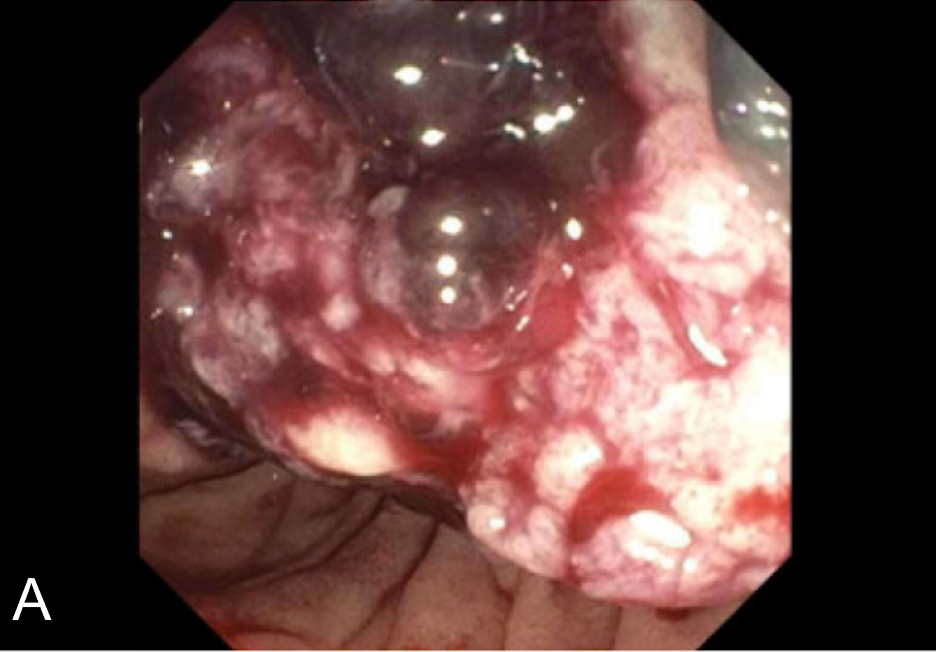
Figure: Figure B. Numerous fragments of tissue with a low power finger-like appearance. The fragments have a fibrovascular core characteristic of papillary growth, and bland epithelium, consistent with low grade papillary neoplasm (inset).
Disclosures:
Kelly Fan indicated no relevant financial relationships.
Nancy Phillips indicated no relevant financial relationships.
Danielle Carpenter indicated no relevant financial relationships.
Isra Taha indicated no relevant financial relationships.
Marina Kim indicated no relevant financial relationships.
Kelly Fan, MD, Nancy Phillips, MD, Danielle Carpenter, MD, Isra N. Taha, MD, Marina Kim, DO. P0126 - Clinical Judgment Guides Multidisciplinary Care: Rare Invasive IOPN with Concurrent Neuroendocrine Tumor Despite Initial Benign Sampling, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
SSM Health Saint Louis University Hospital, St. Louis, MO
Introduction: Intraductal oncocytic papillary neoplasms (IOPN) are rare pancreatic neoplasms that have recently been recognized as a separate entity from other intraductal papillary mucinous neoplasms (IPMNs). This is the case of a patient who presented with a large, symptomatic pancreatic head mass who was found to have an intraductal papillary neoplasm, likely IOPN, and concomitant pancreatic neuroendocrine tumor (NET).
Case Description/
Methods: A 76-year-old woman with gastroesophageal reflux disease and obesity presented to the hospital with nausea, vomiting, reflux, weight loss, and dyspnea for several months.
On admission, labs showed hemoglobin 5.2 g/dL and elevation of alkaline phosphatase, AST ALT and total bilirubin. Computed tomography (CT) revealed a 5.7 x 4.8 cm mass in the pancreatic head and uncinate process. Magnetic resonance imaging (MRI) with magnetic resonance cholangiopancreatography (MRCP) showed the mass obstructing the pancreatic duct and common bile duct (CBD) with CBD dilation.
Endoscopic ultrasound (EUS) revealed a 55mm x 52mm actively bleeding pancreatic head mass abutting the portal vein and infiltrating the duodenum (Fig. A). Fine needle biopsy (FNB) revealed superficial fragments of papillary neoplasm without signs of invasive malignancy. CA 19-9 and CEA were elevated at 262.4 U/mL and 98.2 ng/mL, respectively. Endoscopic retrograde cholangiopancreatography (ERCP) was unsuccessful due to inability to identify the major papilla within the duodenal extension of the mass. Thus, a percutaneous drain was placed to relieve the biliary obstruction. Repeat EUS with biopsy showed superficial fragments of low-grade papillary neoplasm without evidence of invasive malignancy, suggesting either IAPN or IPMN (Fig. B). Following multidisciplinary discussions, the decision to undergo pancreaticoduodenectomy was made due to large tumor size, abuttal of the superior mesenteric vein (SMV), and concern for invasive malignancy not captured with FNB. Pathology from pancreatoduodenectomy revealed intraductal papillary neoplasm (5.1 cm) with associated invasive carcinoma with histologic features most compatible with IOPN, with a very small incidental well differentiated pancreatic NET (0.5 cm).
Discussion: It is rare for intraductal papillary neoplasms to invade the duodenum. Further, there are few reports of concomitant IPMNs and NETs; even less is reported on concomitant IOPNs and NETs. This case exemplifies the importance of multidisciplinary efforts in management of pancreatic tumors.
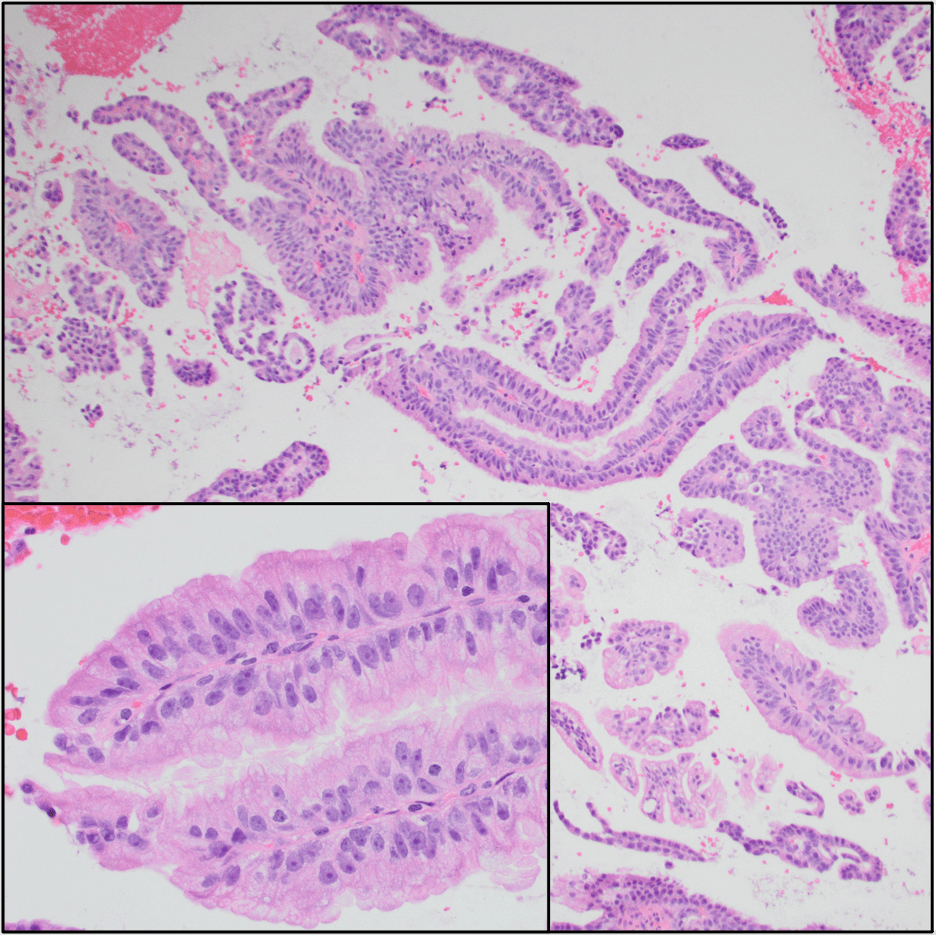
Figure: Figure A. Upper endoscopy revealing a large, infiltrating, actively oozing mass in the area of the major papilla.
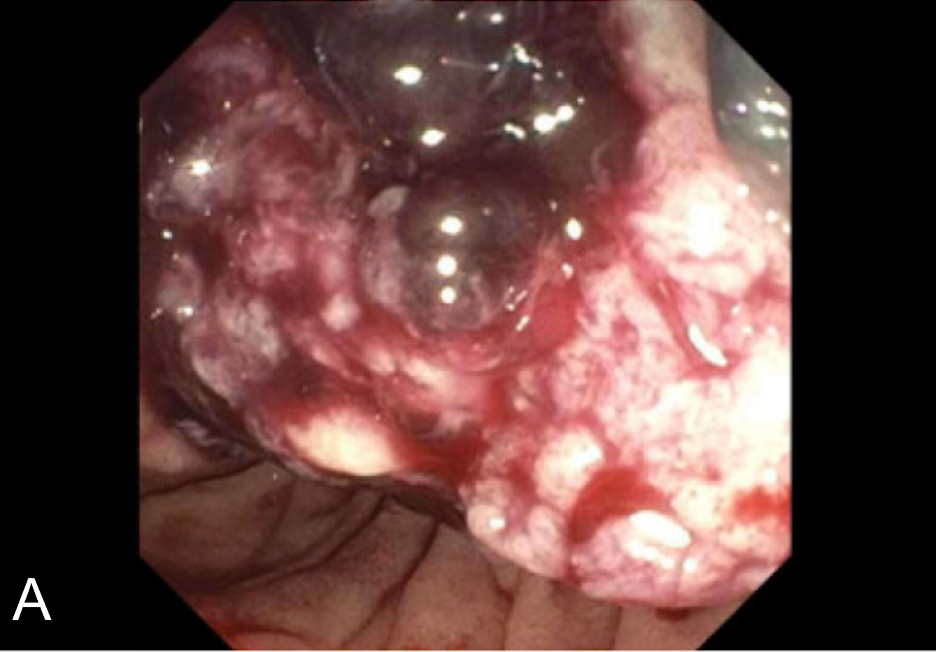
Figure: Figure B. Numerous fragments of tissue with a low power finger-like appearance. The fragments have a fibrovascular core characteristic of papillary growth, and bland epithelium, consistent with low grade papillary neoplasm (inset).
Disclosures:
Kelly Fan indicated no relevant financial relationships.
Nancy Phillips indicated no relevant financial relationships.
Danielle Carpenter indicated no relevant financial relationships.
Isra Taha indicated no relevant financial relationships.
Marina Kim indicated no relevant financial relationships.
Kelly Fan, MD, Nancy Phillips, MD, Danielle Carpenter, MD, Isra N. Taha, MD, Marina Kim, DO. P0126 - Clinical Judgment Guides Multidisciplinary Care: Rare Invasive IOPN with Concurrent Neuroendocrine Tumor Despite Initial Benign Sampling, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
