Sunday Poster Session
Category: Biliary/Pancreas
P0213 - Left Bilothorax of Unknown Origin
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall

Darya Herscovici, MD
University of Massachusetts Chan Medical School
Worcester, MA
Presenting Author(s)
Darya Herscovici, MD, Aravindh Ajithkumar, MD, Mina Zhang, MD, Patrick Bagley, DO
University of Massachusetts Chan Medical School, Worcester, MA
Introduction: Bilothorax is a rare clinical phenomenon defined as the presence of bile within the pleural space. It most commonly presents as a right-sided exudative pleural effusion due to pleurobiliary fistula formation, typically following biliary tract injury. Diagnosis is confirmed by a pleural fluid-to-serum bilirubin ratio of greater than one. Although uncommon, prompt recognition and management are critical to prevent severe complications such as empyema and fibrothorax. Here, we present a unique case of left-sided bilothorax in a patient with complicated biliary history and anatomy.
Case Description/
Methods: A 54-year-old male presented with confusion and cough after a recent discharge for cholangitis with a new chronic percutaneous biliary drain. His medical history included primary sclerosing cholangitis (PSC) necessitating liver transplant, complicated by recurrent autoimmune hepatitis requiring a second liver transplant with Roux-en-Y hepaticojejunostomy. Following his second transplant, he developed papillary thyroid carcinoma for which he underwent left neck dissection and left video-assisted thoracic surgery (VATS).
Workup revealed serum bilirubin of 5.8 mg/dL and alkaline phosphatase of 315 U/L. Chest radiograph showed a large left-sided pleural effusion. Thoracentesis yielded fluid that resembled output from his biliary drain. Pleural fluid bilirubin was 5.5 mg/dL, with a fluid-to-serum ratio of 0.95. A cholangiogram showed no evidence of biliary leak. He was managed with antibiotics and supportive care and discharged with outpatient follow-up for endoscopic ultrasound-directed transgastric ERCP (EDGE) to further evaluate and manage PSC.
Discussion: Left-sided bilothorax is rare, with this being only the third such case in the literature. Its occurrence often requires injury to the biliary tract, causing a pleurobiliary fistula. However, the way in which our patient developed this bilothorax is unclear, given no definitive leak identified on cholangiogram. Nonetheless, he had multiple risk factors for formation, including prior biliary stricture, percutaneous stents, and inflammation surrounding biliary drains that may have caused erosion. His prior left-sided VATS may also have predisposed him to developing a left, rather than right, bilothorax due to manipulation of pleura. This case underscores the need for vigilance and consideration of bilothorax in patients with complex biliary histories, even in the absence of classic findings.

Figure: Figure 1: Left-sided bilothorax on chest radiography
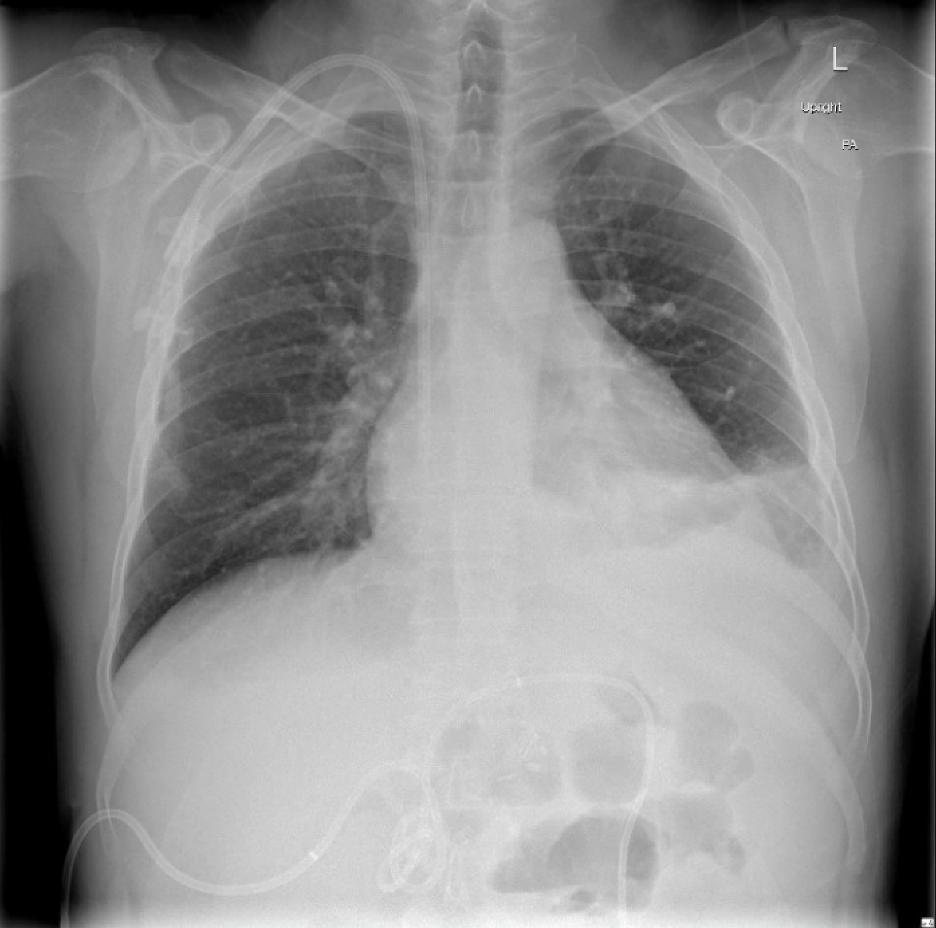
Figure: Figure 2: Visual similarity between biliary drain output (left) and thoracentesis fluid (right)
Disclosures:
Darya Herscovici indicated no relevant financial relationships.
Aravindh Ajithkumar indicated no relevant financial relationships.
Mina Zhang indicated no relevant financial relationships.
Patrick Bagley indicated no relevant financial relationships.
Darya Herscovici, MD, Aravindh Ajithkumar, MD, Mina Zhang, MD, Patrick Bagley, DO. P0213 - Left Bilothorax of Unknown Origin, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
University of Massachusetts Chan Medical School, Worcester, MA
Introduction: Bilothorax is a rare clinical phenomenon defined as the presence of bile within the pleural space. It most commonly presents as a right-sided exudative pleural effusion due to pleurobiliary fistula formation, typically following biliary tract injury. Diagnosis is confirmed by a pleural fluid-to-serum bilirubin ratio of greater than one. Although uncommon, prompt recognition and management are critical to prevent severe complications such as empyema and fibrothorax. Here, we present a unique case of left-sided bilothorax in a patient with complicated biliary history and anatomy.
Case Description/
Methods: A 54-year-old male presented with confusion and cough after a recent discharge for cholangitis with a new chronic percutaneous biliary drain. His medical history included primary sclerosing cholangitis (PSC) necessitating liver transplant, complicated by recurrent autoimmune hepatitis requiring a second liver transplant with Roux-en-Y hepaticojejunostomy. Following his second transplant, he developed papillary thyroid carcinoma for which he underwent left neck dissection and left video-assisted thoracic surgery (VATS).
Workup revealed serum bilirubin of 5.8 mg/dL and alkaline phosphatase of 315 U/L. Chest radiograph showed a large left-sided pleural effusion. Thoracentesis yielded fluid that resembled output from his biliary drain. Pleural fluid bilirubin was 5.5 mg/dL, with a fluid-to-serum ratio of 0.95. A cholangiogram showed no evidence of biliary leak. He was managed with antibiotics and supportive care and discharged with outpatient follow-up for endoscopic ultrasound-directed transgastric ERCP (EDGE) to further evaluate and manage PSC.
Discussion: Left-sided bilothorax is rare, with this being only the third such case in the literature. Its occurrence often requires injury to the biliary tract, causing a pleurobiliary fistula. However, the way in which our patient developed this bilothorax is unclear, given no definitive leak identified on cholangiogram. Nonetheless, he had multiple risk factors for formation, including prior biliary stricture, percutaneous stents, and inflammation surrounding biliary drains that may have caused erosion. His prior left-sided VATS may also have predisposed him to developing a left, rather than right, bilothorax due to manipulation of pleura. This case underscores the need for vigilance and consideration of bilothorax in patients with complex biliary histories, even in the absence of classic findings.

Figure: Figure 1: Left-sided bilothorax on chest radiography
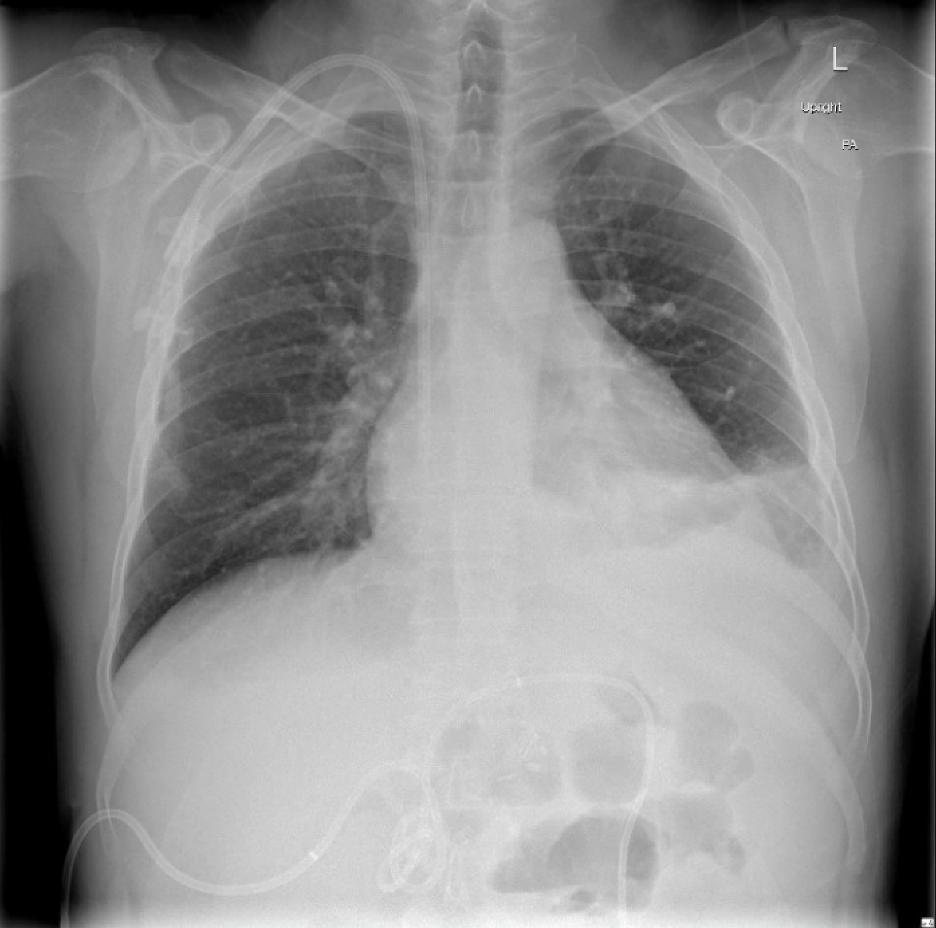
Figure: Figure 2: Visual similarity between biliary drain output (left) and thoracentesis fluid (right)
Disclosures:
Darya Herscovici indicated no relevant financial relationships.
Aravindh Ajithkumar indicated no relevant financial relationships.
Mina Zhang indicated no relevant financial relationships.
Patrick Bagley indicated no relevant financial relationships.
Darya Herscovici, MD, Aravindh Ajithkumar, MD, Mina Zhang, MD, Patrick Bagley, DO. P0213 - Left Bilothorax of Unknown Origin, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
