Sunday Poster Session
Category: Colon
P0292 - Outcomes in Patients With Malignancies Prior to Diagnosis of Colorectal Cancer: A Propensity Score-Matched Analysis

Imran Qureshi, MD (he/him/his)
Rutgers New Jersey Medical School
Newark, NJ
Presenting Author(s)
1Rutgers New Jersey Medical School, Newark, NJ; 2NYU Grossman School of Medicine, Division of Gastroenterology and Hepatology, New York, NY
Introduction:
Colorectal cancer(CRC) is the third most common cancer and has a rising incidence globally. CRC shares many risk factors with other malignancies and can be a part of hereditary cancer syndromes. Herein, we evaluate outcomes in patients with CRC and a history of prior malignancies.
Methods:
We queried the National Cancer Database from 2004 to 2022 for patients with CRC. We excluded patients with an unknown number of malignancies. Then we divided our sample into two cohorts: patients diagnosed with only CRC or CRC as the first of multiple malignancies, and patients with CRC with at least one malignancy before diagnosis of CRC. We then performed 1:1 propensity score matching(PSM) for sex, race, ethnicity, insurance, setting, comorbidities, literacy, and income. We then conducted a logistic regression to get the odds ratio(OR), 95% confidence interval(CI), and p-values for early onset CRC(Age < 45 at presentation), late stage(stage 3/4) at presentation, delayed treatment( >6 weeks after diagnosis), and 30-day readmission after surgery. Subsequently, we used Kaplan-Meier methods and fit a Cox proportional hazards model for each stage to assess the impact of having prior malignancies on mortality and reported hazard ratios(HR) along with 95% CI and p-values.
Results:
We had 305,290 patients in each cohort after PSM. Compared to patients with CRC was as their first or only malignancy, patients who developed CRC after a previous cancer had lower odds of having early-onset CRC(OR=0.60, 95% CI:0.58–0.61, p< 0.01) and late stage presentaion(OR=0.78, 95% CI:0.77–0.79, p< 0.01), but were more likely to have treatment delay(OR=1.21, 95% CI:1.20–1.23, p< 0.01) and 30 day readmissions (OR=1.17, 95% CI:1.14–1.20, p< 0.01) (Figure 1). These patients also experienced higher mortality for stage 1(HR=1.55, 95% CI:1.52–1.57, p< 0.01), stage 2(HR=1.44, 95% CI: 1.42-1.47, p< 0.01), and stage 3 CRC(HR=1.29, 95% CI:1.27–1.31, p< 0.01), but no difference in stage 4 mortality(HR=1.00, 95% CI: 0.98-1.01, p=0.66) (Figure 2).
Discussion:
Our analysis shows that patients with a prior history of malignancies were less likely to present with late-stage disease, but still encountered treatment delays, higher readmission rates, and increased mortality. This may be explained by aggressive tumor biology, genetic disorders predisposing patients to multiple tumors, or poor response to treatment in these patients. However, further studies are needed to understand the cause of these and improve outcomes in these patients.
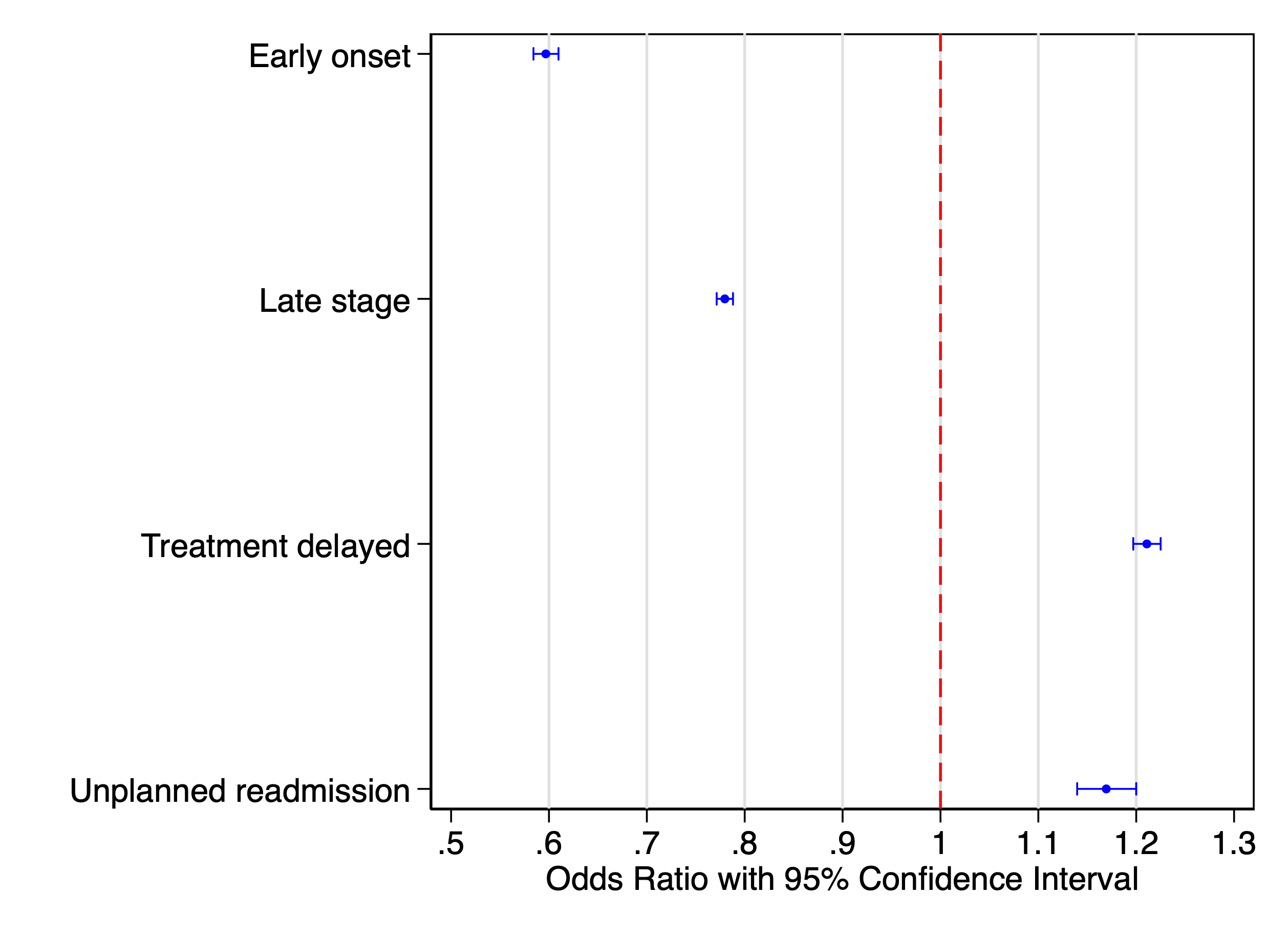
Figure: Figure 1: Forest plot of odds ratio with 95% confidence interval of patients with a history of previous malignancies

Figure: Figure 2: Kaplan-Meier survival curves comparing mortality of patients with and without previous malignancies for stage 1 (A), stage 2 (B), stage 3 (C), and stage 4 (D) colorectal cancer
Disclosures:
Imran Qureshi indicated no relevant financial relationships.
Aasma Shaukat: Freenome inc – Consultant.
Imran Qureshi, MD1, Aasma Shaukat, MD, MPH, FACG2. P0292 - Outcomes in Patients With Malignancies Prior to Diagnosis of Colorectal Cancer: A Propensity Score-Matched Analysis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
