Sunday Poster Session
Category: Colon
P0280 - Amyloidosis of the Gastrointestinal Tract: Subtypes, Clinical Manifestations, and Organ System Involvement - Systematic Review
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall

Bipneet Singh, MD
Henry Ford Jackson Hospital
Lexington, KY
Presenting Author(s)
Bipneet Singh, MD1, Palak Grover, MD1, Gurleen Kaur, MBBS2, Jahnavi Ethakota, MD1, Sakshi Bai, MD1, Rahul Jain, MBBS3, Merritt Bern, MD1
1Henry Ford Jackson Hospital, Jackson, MI; 2Government Medical College and Hospital, Khanna, Punjab, India; 3Sri Manakula Vinayagar Medical College, Pondicherry, Puducherry, India
Introduction: Gastrointestinal (GI) involvement in amyloidosis is a recognized but relatively uncommon manifestation that presents variably across different amyloid types. This review synthesizes data from multiple studies to delineate amyloid subtypes affecting the GI tract, associated clinical symptoms, diagnostic findings, and systemic involvement.
Methods: We analyzed seven studies conducted between 1993 and 2021 involving biopsy-proven GI amyloidosis. Studies included both localized and systemic cases with gastrointestinal (GI)- dominant features. Data were extracted on the distribution of amyloid types, clinical manifestations, histological sites of deposition, systemic involvement, and survival outcomes.
Results: AL (light chain) amyloidosis was the predominant subtype involved in gastrointestinal (GI) amyloidosis, comprising 55–83% of cases. ATTR amyloidosis accounted for 4–11% of cases, while AA amyloidosis ranged from 6–13%. Clinical symptoms were variable but included diarrhea (32–46%), weight loss (29–45%), GI bleeding (27–36%), early satiety and anorexia (26–37.5%), and nausea/vomiting (29.2%). Diarrhea was notably common in AL and intractable in 32.2% of AA cases. Pseudo-obstruction was rare but present in AA and AL. Histopathologically, the stomach was involved in 55% of AL cases and 42% overall, followed by the colon (45% AL, 24% overall), rectum (35% AL, 5% overall), and small bowel (5% AL, 26% overall).
Discussion: Patients had predominantly the AL type of amyloidosis associated with gastrointestinal involvement. Diarrhea was the most predominant symptom. Histology was variable, ranging from polypoid to erosive lesions. GI amyloidosis is a rare manifestation, often overlooked due to paucity of specific. Diagnosis requires vigilance by the physician, endoscopic study, and biopsy prompted by a pre-existing systemic diagnosis.
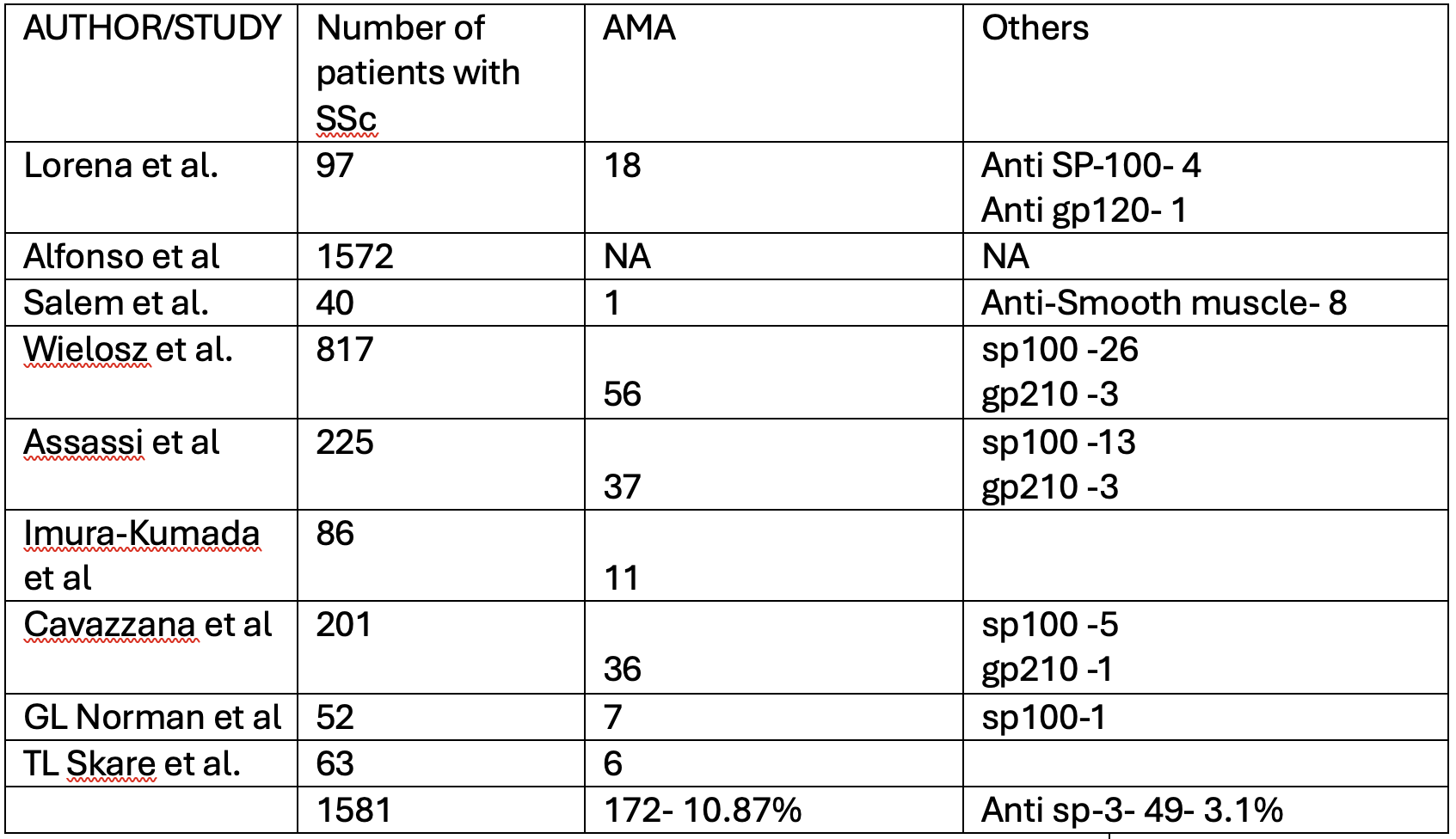
Figure: Table- Subtypes, symptoms and site prevalence in GI Amyloidosis
Disclosures:
Bipneet Singh indicated no relevant financial relationships.
Palak Grover indicated no relevant financial relationships.
Gurleen Kaur indicated no relevant financial relationships.
Jahnavi Ethakota indicated no relevant financial relationships.
Sakshi Bai indicated no relevant financial relationships.
Rahul Jain indicated no relevant financial relationships.
Merritt Bern indicated no relevant financial relationships.
Bipneet Singh, MD1, Palak Grover, MD1, Gurleen Kaur, MBBS2, Jahnavi Ethakota, MD1, Sakshi Bai, MD1, Rahul Jain, MBBS3, Merritt Bern, MD1. P0280 - Amyloidosis of the Gastrointestinal Tract: Subtypes, Clinical Manifestations, and Organ System Involvement - Systematic Review, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Henry Ford Jackson Hospital, Jackson, MI; 2Government Medical College and Hospital, Khanna, Punjab, India; 3Sri Manakula Vinayagar Medical College, Pondicherry, Puducherry, India
Introduction: Gastrointestinal (GI) involvement in amyloidosis is a recognized but relatively uncommon manifestation that presents variably across different amyloid types. This review synthesizes data from multiple studies to delineate amyloid subtypes affecting the GI tract, associated clinical symptoms, diagnostic findings, and systemic involvement.
Methods: We analyzed seven studies conducted between 1993 and 2021 involving biopsy-proven GI amyloidosis. Studies included both localized and systemic cases with gastrointestinal (GI)- dominant features. Data were extracted on the distribution of amyloid types, clinical manifestations, histological sites of deposition, systemic involvement, and survival outcomes.
Results: AL (light chain) amyloidosis was the predominant subtype involved in gastrointestinal (GI) amyloidosis, comprising 55–83% of cases. ATTR amyloidosis accounted for 4–11% of cases, while AA amyloidosis ranged from 6–13%. Clinical symptoms were variable but included diarrhea (32–46%), weight loss (29–45%), GI bleeding (27–36%), early satiety and anorexia (26–37.5%), and nausea/vomiting (29.2%). Diarrhea was notably common in AL and intractable in 32.2% of AA cases. Pseudo-obstruction was rare but present in AA and AL. Histopathologically, the stomach was involved in 55% of AL cases and 42% overall, followed by the colon (45% AL, 24% overall), rectum (35% AL, 5% overall), and small bowel (5% AL, 26% overall).
Discussion: Patients had predominantly the AL type of amyloidosis associated with gastrointestinal involvement. Diarrhea was the most predominant symptom. Histology was variable, ranging from polypoid to erosive lesions. GI amyloidosis is a rare manifestation, often overlooked due to paucity of specific. Diagnosis requires vigilance by the physician, endoscopic study, and biopsy prompted by a pre-existing systemic diagnosis.
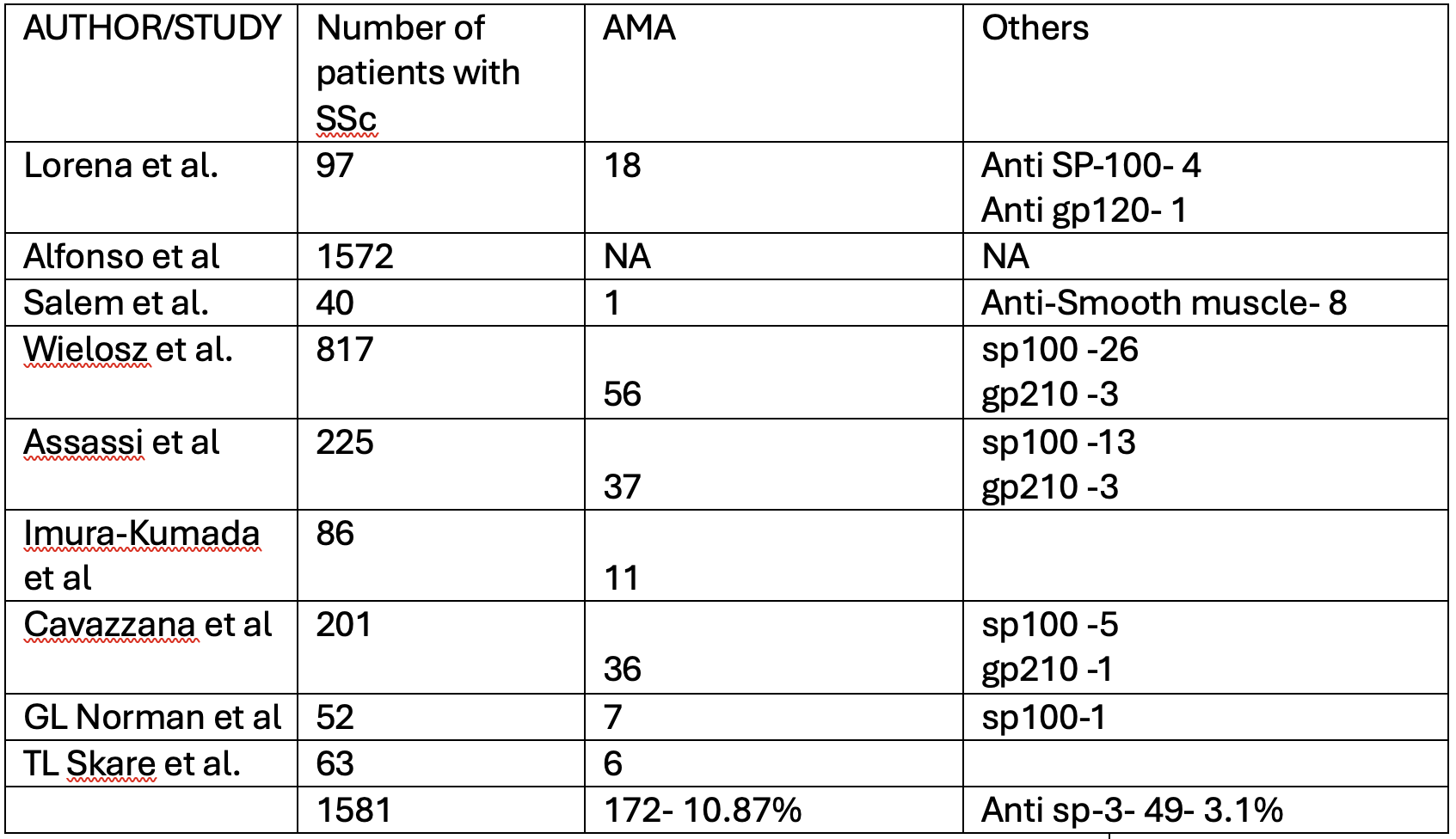
Figure: Table- Subtypes, symptoms and site prevalence in GI Amyloidosis
Disclosures:
Bipneet Singh indicated no relevant financial relationships.
Palak Grover indicated no relevant financial relationships.
Gurleen Kaur indicated no relevant financial relationships.
Jahnavi Ethakota indicated no relevant financial relationships.
Sakshi Bai indicated no relevant financial relationships.
Rahul Jain indicated no relevant financial relationships.
Merritt Bern indicated no relevant financial relationships.
Bipneet Singh, MD1, Palak Grover, MD1, Gurleen Kaur, MBBS2, Jahnavi Ethakota, MD1, Sakshi Bai, MD1, Rahul Jain, MBBS3, Merritt Bern, MD1. P0280 - Amyloidosis of the Gastrointestinal Tract: Subtypes, Clinical Manifestations, and Organ System Involvement - Systematic Review, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
