Sunday Poster Session
Category: Colon
P0377 - Steroid-Induced Transverse Colon Perforation in Systemic Lupus Erythematosus: A Diagnostic Challenge
.jpg)
Ridwan A. Lawal, MBBS (he/him/his)
University of Texas Rio Grande Valley - Knapp Medical Center
Weslaco, TX
Presenting Author(s)
1University of Texas Rio Grande Valley - Knapp Medical Center, Weslaco, TX; 2University of texas (knapp) rgv, Weslaco, TX
Introduction:
Gastrointestinal symptoms in systemic lupus erythematosus (SLE) vary widely, from mild cases to potentially life-threatening conditions. Gastrointestinal injury induced by corticosteroids and Lupus enteritis, a rare complication of vasculitis, are both recognized causes of bowel perforation. However, distinguishing between these two conditions can be clinically challenging. We present a case of spontaneous transverse colon perforation in a patient with systemic lupus erythematosus, highlighting a critical diagnostic and management dilemma.
Case Description/
Methods:
A 62-year-old female with systemic lupus erythematosus presented with sudden abdominal pain in both the right upper and lower quadrants, accompanied by nausea and vomiting. She had been on a high-dose prednisone regimen, tapered from 60 mg to 10 mg over three months before her presentation.
Upon examination, she was afebrile but showed significant abdominal tenderness. Laboratory tests revealed leukocytosis, elevated lactic acid levels, and a hemoglobin level of 10.3 g/dL. A chest radiograph showed free air under the right hemidiaphragm. A subsequent CT scan confirmed the presence of intraperitoneal free air anterior to the liver and spleen, but no clear source of perforation could be identified.
She underwent emergent robotic-assisted diagnostic laparoscopy, which was converted to an exploratory laparotomy with transverse colectomy. During the procedure, purulence was observed in the right upper quadrant, and a single perforation was found in the mid-transverse colon, with no indications of diverticulitis or malignancy. The postoperative course was uneventful.
Histopathologic examination revealed a perforated ulcer surrounded by granulation tissue, acute on chronic inflammation, and serosal adhesions. Notably, there was no evidence of vasculitis, thrombosis, or ischemic necrosis, making lupus enteritis less likely. The findings were most consistent with steroid-induced mucosal injury.
Discussion: This case highlights a significant diagnostic challenge in systemic lupus erythematosus (SLE): distinguishing between complications related to treatment and lupus enteritis. While corticosteroids are vital for managing flare-ups, they can weaken the mucosal lining and mask symptoms, which increases the risk of perforation. It is essential to accurately identify the underlying cause to optimize treatment and prevent future occurrences.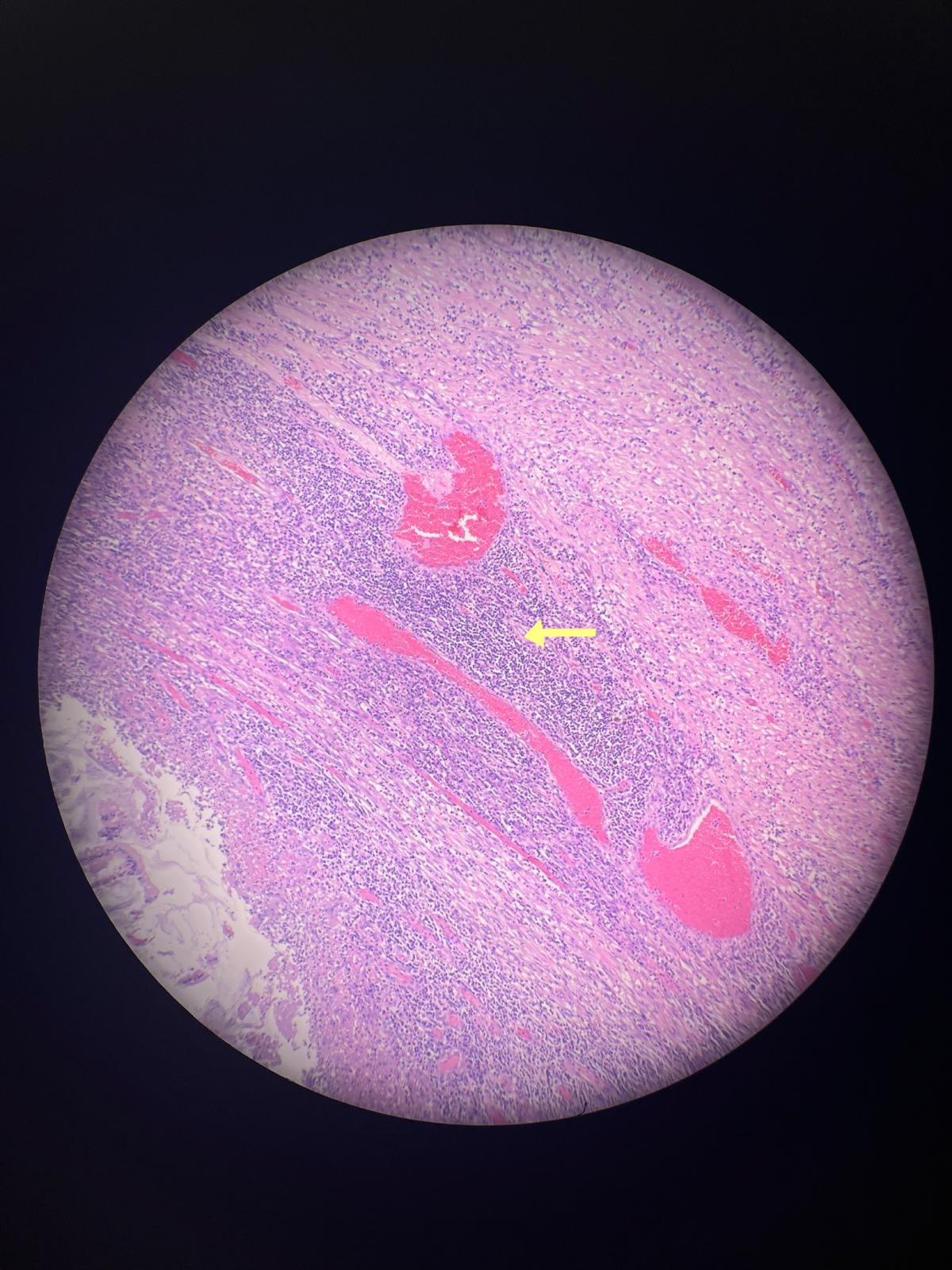
Figure: H&E Image showing transmural acute and chronic inflammation without vascular involvement.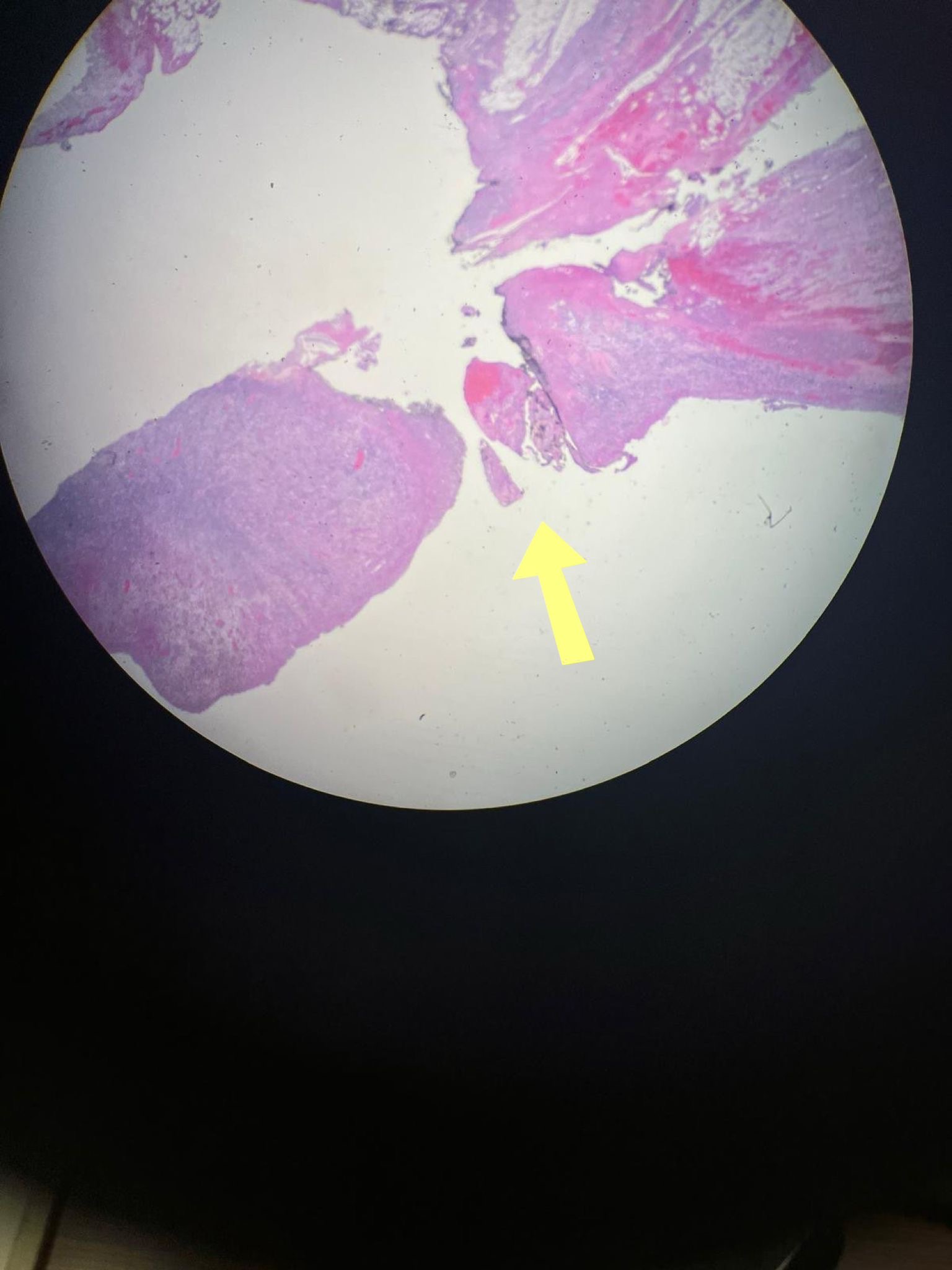
Figure: H&E Image showing full-thickness ulceration and perforation of the colonic wall.
Disclosures:
Ridwan Lawal indicated no relevant financial relationships.
Nestor Malaga indicated no relevant financial relationships.
Nida Asif indicated no relevant financial relationships.
Ridwan A. Lawal, MBBS1, Nestor C. Malaga, MD1, Nida Asif, MD2. P0377 - Steroid-Induced Transverse Colon Perforation in Systemic Lupus Erythematosus: A Diagnostic Challenge, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.

