Sunday Poster Session
Category: Colon
P0447 - Now You See Me, Now You Don't: An Inflamed Diverticulum With an Obstructing Fecalith Mimicking Cecal Malignancy

Anna Archbold, MD
University of Texas Medical Branch
Texas City, TX
Presenting Author(s)
1University of Texas Medical Branch, Texas City, TX; 2University of Texas Medical Branch, Department of Gastroenterology and Hepatology, Galveston, TX; 3University of Texas Medical Branch, Galveston, TX
Introduction:
Colorectal cancer (CRC) remains a leading cause of cancer-related morbidity and mortality. While colonoscopy is essential for detecting colon cancer, certain conditions can closely mimic malignancy and pose a diagnostic challenge.
We present a case of a presumed malignancy that was later determined to be an inflammatory mass arising from an impacted diverticulum.
Case Description/
Methods:
A 67-year-old male presented for surveillance of colon polyps. He had a self-reported history of prior colon polyps of uncertain histology. He was uncertain if he had any family history of CRC.
Colonoscopy revealed a medium-sized fungating, non-obstructing mass in the cecum (Figure 1). Biopsies revealed colonic mucosa with ulceration and granulation tissue and was not diagnostic for malignancy. Four additional small tubular adenomas were resected during the procedure.
Given the appearance of the cecal mass, there was still suspicion for malignancy and the patient was brought back for another colonoscopy for repeat sampling. CEA level was within normal limits. CT chest, abdomen and pelvis were also obtained and showed no evidence of intrathoracic or abdominopelvic metastases.
During repeat colonoscopy a month after the original procedure, the cecal mass was no longer visualized. There was a localized area of mildly erythematous mucosa at the site of the prior lesion (Figure 2) and this was close to a cecal diverticulum. Biopsies revealed no ulceration, dysplasia, inflammation, or malignancy. The initial mass was then most likely an impacted fecalith within a cecal diverticulum leading to surrounding inflammatory changes and a pseudotumor-like appearance.
Discussion:
CRC remains the third most common type of cancer worldwide and a leading cause of cancer-related deaths in the USA. Colon cancer screening via colonoscopy is an effective method for detection of colon cancer and precancerous lesions. However, it is important to be aware of benign conditions that can mimic CRC visually including impacted fecaliths, ischemic colitis, endometriosis, and various infectious etiologies. This case illustrates a diagnostic challenge and highlights the importance of careful interpretation of endoscopic findings in the context of inconclusive histology. This helps in preventing potential misdiagnoses, unwarranted invasive interventions, and unnecessary anxiety for patients.
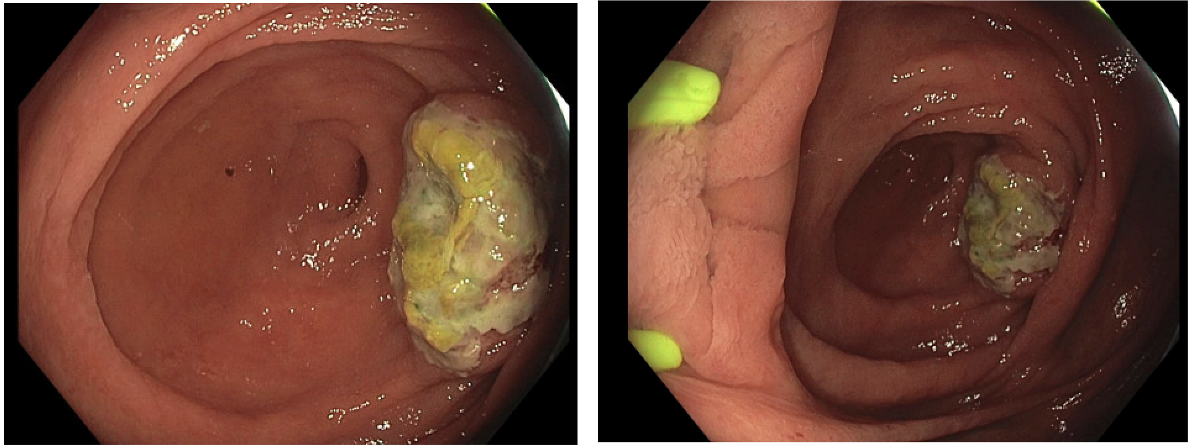
Figure: Figure 1: Endoscopic finding of medium-sized fungating, infiltrative, non-obstructing mass in the cecum.
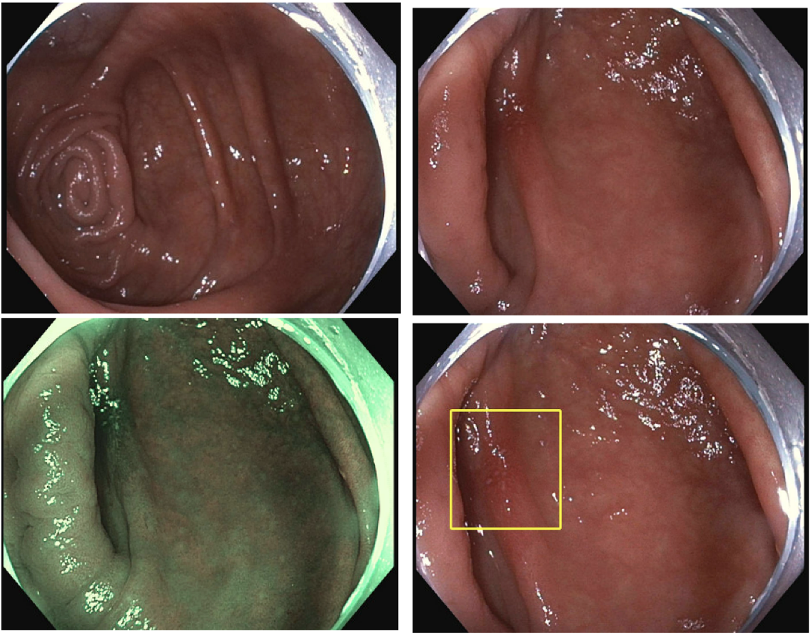
Figure: Figure 2: Endoscopic finding of localized area of mildly erythematous mucosa in the cecum
Disclosures:
Anna Archbold indicated no relevant financial relationships.
Julia Zhang indicated no relevant financial relationships.
Sreeram Parupudi indicated no relevant financial relationships.
Anna Archbold, MD1, Julia Zhang, MD2, Sreeram Parupudi, MD3. P0447 - Now You See Me, Now You Don't: An Inflamed Diverticulum With an Obstructing Fecalith Mimicking Cecal Malignancy, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
