Sunday Poster Session
Category: Diet, Nutrition, and Obesity
P0542 - The Holy Grail Illusion: GLP-1s, Pharmacologic Hope, and Public Health Failure in Obesity Care
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall

Julian Galindo-Ramírez, MD (he/him/his)
University of Texas Rio Grande Valley - HCA
McAllen, Colombia
Presenting Author(s)
Julian Galindo-Ramírez, MD1, Ivan Mogollon, MD2, Calderon Aura, MD3, Daniela Hernandez, MD2
1University of Texas Rio Grande Valley - HCA, McAllen, TX; 2University of Texas Rio Grande Valley, Edinburg, TX; 3University of Texas Rio Grande Valley, McAllen, TX
Introduction: Glucagon-like peptide-1 receptor agonists (GLP-1 RAs), such as semaglutide and tirzepatide, are widely praised for promoting weight loss. However, their rapid adoption risks diverting attention from the deeper structural and socioeconomic drivers of obesity. This study explores the public health implications of GLP-1 RA proliferation in underserved areas, focusing on the Rio Grande Valley (RGV) in South Texas.
Methods: We conducted an evidence-informed policy and public health analysis using epidemiological data, peer-reviewed literature, and policy reports. McAllen, Texas—a city with the highest adult obesity rate and lowest physical activity in the U.S.—served as a case study to illustrate structural barriers to equitable obesity care.
Results: In McAllen, 45% of adults are obese and 31% overweight. The city ranks lowest in physical activity, constrained by limited walkability and park access. Across the RGV, 1 in 4 households experiences food insecurity, over half of neighborhoods are food deserts, and many live in colonias lacking basic infrastructure. Healthcare access is limited—50% of adults in Hidalgo County are uninsured, and Texas has not expanded Medicaid. Chronic conditions like diabetes (affecting nearly 30% of adults) and MASLD are widespread. GLP-1 therapies are unaffordable for most, with monthly out-of-pocket costs over $900–$1,300 and minimal Medicaid coverage. Cross-border acquisition of unregulated GLP-1s in Mexico is common, or obtaining medications from compound pharmacies or wellness business without monitoring, raising safety concerns. Most patients regain weight within two years of stopping treatment, often resuming therapy without clinical oversight.
Discussion: This overreliance on GLP-1 RAs risks medicalizing obesity and ignoring its root causes. In RGV, decades of underinvestment in public health, widespread food insecurity, and limited healthcare access make long-term pharmacologic solutions inadequate. Without broader reforms—such as community-based prevention, better infrastructure, targeted insurance expansion, and regulation—GLP-1s remain a costly, short-term fix. True progress requires aligning pharmacologic advances with social and structural change to avoid reinforcing stigma and deepen health inequities. To ensure these medications contribute meaningfully to health equity, policy reform must accompany pharmacologic innovation. Recommendations, outlined in Table 1, present a more comprehensive and equitable approach.
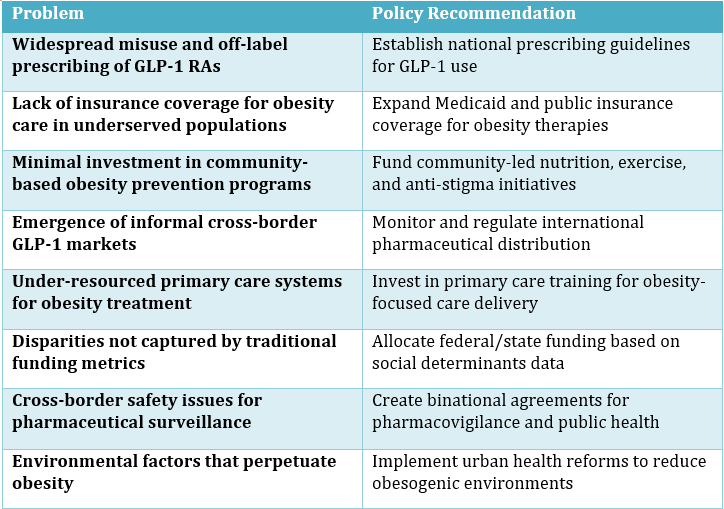
Figure: Table 1. Policy Recommendations for Equitable Integration of GLP-1 Receptor Agonists in Obesity Care.
Disclosures:
Julian Galindo-Ramírez indicated no relevant financial relationships.
Ivan Mogollon indicated no relevant financial relationships.
Calderon Aura indicated no relevant financial relationships.
Daniela Hernandez indicated no relevant financial relationships.
Julian Galindo-Ramírez, MD1, Ivan Mogollon, MD2, Calderon Aura, MD3, Daniela Hernandez, MD2. P0542 - The Holy Grail Illusion: GLP-1s, Pharmacologic Hope, and Public Health Failure in Obesity Care, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1University of Texas Rio Grande Valley - HCA, McAllen, TX; 2University of Texas Rio Grande Valley, Edinburg, TX; 3University of Texas Rio Grande Valley, McAllen, TX
Introduction: Glucagon-like peptide-1 receptor agonists (GLP-1 RAs), such as semaglutide and tirzepatide, are widely praised for promoting weight loss. However, their rapid adoption risks diverting attention from the deeper structural and socioeconomic drivers of obesity. This study explores the public health implications of GLP-1 RA proliferation in underserved areas, focusing on the Rio Grande Valley (RGV) in South Texas.
Methods: We conducted an evidence-informed policy and public health analysis using epidemiological data, peer-reviewed literature, and policy reports. McAllen, Texas—a city with the highest adult obesity rate and lowest physical activity in the U.S.—served as a case study to illustrate structural barriers to equitable obesity care.
Results: In McAllen, 45% of adults are obese and 31% overweight. The city ranks lowest in physical activity, constrained by limited walkability and park access. Across the RGV, 1 in 4 households experiences food insecurity, over half of neighborhoods are food deserts, and many live in colonias lacking basic infrastructure. Healthcare access is limited—50% of adults in Hidalgo County are uninsured, and Texas has not expanded Medicaid. Chronic conditions like diabetes (affecting nearly 30% of adults) and MASLD are widespread. GLP-1 therapies are unaffordable for most, with monthly out-of-pocket costs over $900–$1,300 and minimal Medicaid coverage. Cross-border acquisition of unregulated GLP-1s in Mexico is common, or obtaining medications from compound pharmacies or wellness business without monitoring, raising safety concerns. Most patients regain weight within two years of stopping treatment, often resuming therapy without clinical oversight.
Discussion: This overreliance on GLP-1 RAs risks medicalizing obesity and ignoring its root causes. In RGV, decades of underinvestment in public health, widespread food insecurity, and limited healthcare access make long-term pharmacologic solutions inadequate. Without broader reforms—such as community-based prevention, better infrastructure, targeted insurance expansion, and regulation—GLP-1s remain a costly, short-term fix. True progress requires aligning pharmacologic advances with social and structural change to avoid reinforcing stigma and deepen health inequities. To ensure these medications contribute meaningfully to health equity, policy reform must accompany pharmacologic innovation. Recommendations, outlined in Table 1, present a more comprehensive and equitable approach.
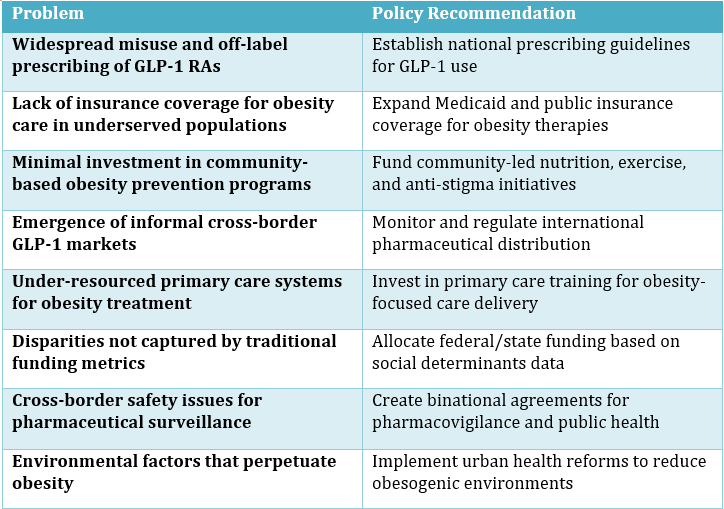
Figure: Table 1. Policy Recommendations for Equitable Integration of GLP-1 Receptor Agonists in Obesity Care.
Disclosures:
Julian Galindo-Ramírez indicated no relevant financial relationships.
Ivan Mogollon indicated no relevant financial relationships.
Calderon Aura indicated no relevant financial relationships.
Daniela Hernandez indicated no relevant financial relationships.
Julian Galindo-Ramírez, MD1, Ivan Mogollon, MD2, Calderon Aura, MD3, Daniela Hernandez, MD2. P0542 - The Holy Grail Illusion: GLP-1s, Pharmacologic Hope, and Public Health Failure in Obesity Care, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
