Sunday Poster Session
Category: Colorectal Cancer Prevention
P0536 - Primary Anorectal Melanoma, an Unusual Presentation With Unfavorable Prognosis: Case Report
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall

Natalia Rodriguez-Martino, MD (she/her/hers)
University of Puerto Rico, Medical Sciences Campus
San Juan, PR
Presenting Author(s)
Natalia Rodriguez-Martino, MD1, Jorge Cruz-Cruz, MD1, Jose Rodríguez-León, MD2
1University of Puerto Rico, Medical Sciences Campus, San Juan, Puerto Rico; 2HRP Labs, San Juan, Puerto Rico
Introduction: Melanomas can originate from cutaneous or mucosal tissues, both types arising from melanocytes. In the rectum, melanocytes are primarily located in the anal transition zone and squamous zone. Anorectal malignant melanoma is a rare cancer with poorly defined presentation that tends to follow an aggressive course. It typically occurs in the fifth-sixth decade of life, with female predominance. Common symptoms are nonspecific and include rectal bleeding, which is frequently mistaken for hemorrhoids. Due to submucosal drainage spread of the tumor, more than 50% of patients are found to have distant metastases at time of diagnosis.
Case Description/
Methods: We report a case of an 86 y/o female patient with a medical history of hypertension who presented with a one-month history of constipation and diffuse abdominal pain, with worsening symptoms and the development of rectal bleeding in the past 1-week. Denied weight loss, anal pruritus, rectal mass, rectal pain, nor family history of colon cancer. Laboratory findings were consistent with normocytic normochromic anemia. Abdominopelvic CT scan performed with findings of an intraluminal mass in the rectum with suspected liver metastases. Endoscopic examination revealed an ulcerating, black-colored polypoid lesion primarily located at the anorectal junction, with 2cm proximal extension. A second similar lesion was identified approximately 6cm from anal verge. Biopsy specimens revealed pleomorphic lesions displaying high mitotic rate, prominent nucleoli and positive immunohistochemical staining with markers HMB45, SOX100 and melA.
Discussion: To our knowledge, this case adds to the few reported instances of synchronous anorectal mucosal melanomas. It’s rarity, non-specific symptoms and increase in incidence underscores the need for heightened clinical awareness. Limited understanding of its causes and late presentation in older patients pose diagnostic and treatment challenges. Increasing awareness in the gastroenterology community is essential for early detection, better outcomes, and avoiding misdiagnosis of this aggressive malignancy.
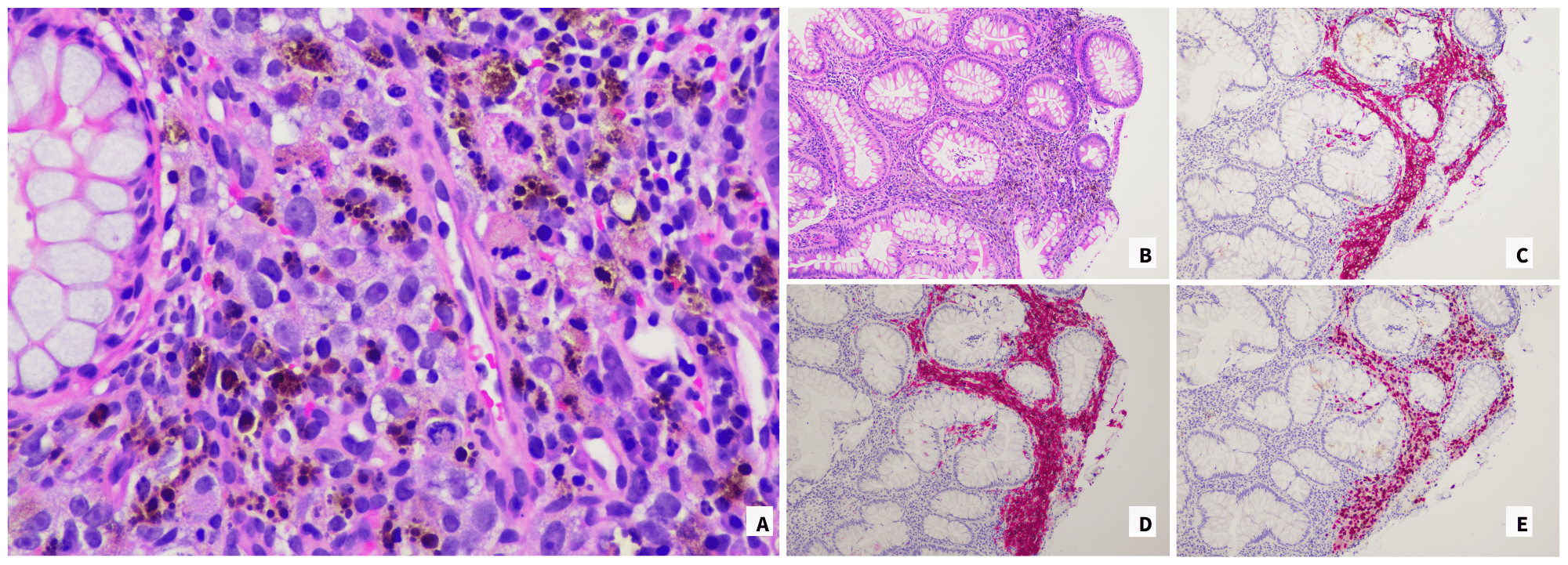
Figure: A. Sheets and nests of malignant-appearing epithelioid cells with prominent nucleoli, atypical mitoses, and conspicuous brown pigment infiltrating the rectal mucosa (H&E, original magnification 400x); B. Malignant-appearing epithelioid cells with abundant brown pigment expanding the lamina propria of the rectal mucosa (H&E, original magnification 100x); C. Malignant cells demonstrating HMB45 positivity (original magnification 100x);
D. Malignant cells demonstrating nuclear positivity for SOX10 (original magnification 100x); E. Malignant cells demonstrating MelA positivity (original magnification 100x).
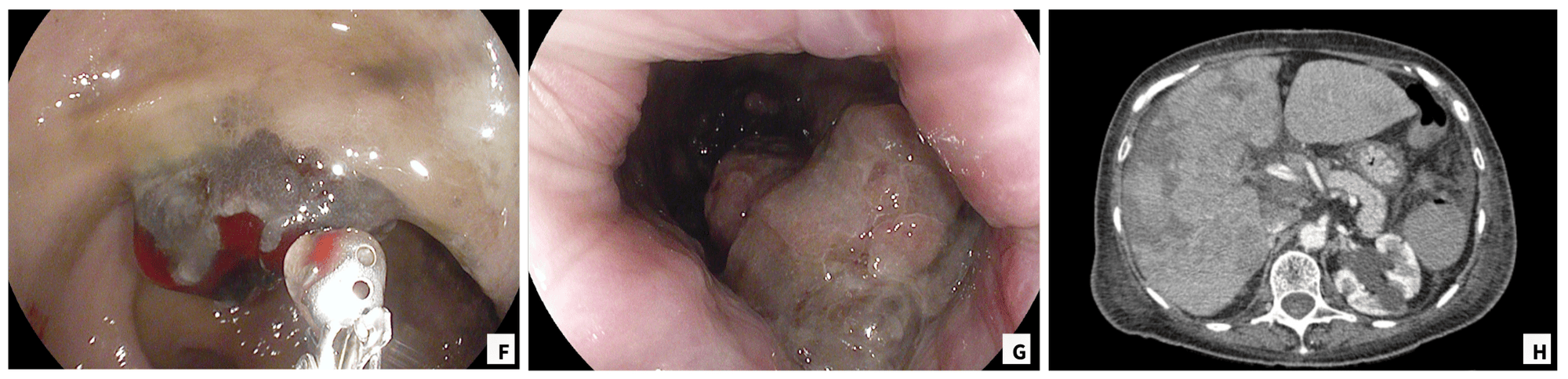
Figure: F. Black-colored polypoid lesion located 6cm from anal verge; G. Ulcerating, black-colored polypoid lesion located at the anorectal junction; H. Abdominal CT-scan with evidence of liver metastases.
Disclosures:
Natalia Rodriguez-Martino indicated no relevant financial relationships.
Jorge Cruz-Cruz indicated no relevant financial relationships.
Jose Rodríguez-León indicated no relevant financial relationships.
Natalia Rodriguez-Martino, MD1, Jorge Cruz-Cruz, MD1, Jose Rodríguez-León, MD2. P0536 - Primary Anorectal Melanoma, an Unusual Presentation With Unfavorable Prognosis: Case Report, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1University of Puerto Rico, Medical Sciences Campus, San Juan, Puerto Rico; 2HRP Labs, San Juan, Puerto Rico
Introduction: Melanomas can originate from cutaneous or mucosal tissues, both types arising from melanocytes. In the rectum, melanocytes are primarily located in the anal transition zone and squamous zone. Anorectal malignant melanoma is a rare cancer with poorly defined presentation that tends to follow an aggressive course. It typically occurs in the fifth-sixth decade of life, with female predominance. Common symptoms are nonspecific and include rectal bleeding, which is frequently mistaken for hemorrhoids. Due to submucosal drainage spread of the tumor, more than 50% of patients are found to have distant metastases at time of diagnosis.
Case Description/
Methods: We report a case of an 86 y/o female patient with a medical history of hypertension who presented with a one-month history of constipation and diffuse abdominal pain, with worsening symptoms and the development of rectal bleeding in the past 1-week. Denied weight loss, anal pruritus, rectal mass, rectal pain, nor family history of colon cancer. Laboratory findings were consistent with normocytic normochromic anemia. Abdominopelvic CT scan performed with findings of an intraluminal mass in the rectum with suspected liver metastases. Endoscopic examination revealed an ulcerating, black-colored polypoid lesion primarily located at the anorectal junction, with 2cm proximal extension. A second similar lesion was identified approximately 6cm from anal verge. Biopsy specimens revealed pleomorphic lesions displaying high mitotic rate, prominent nucleoli and positive immunohistochemical staining with markers HMB45, SOX100 and melA.
Discussion: To our knowledge, this case adds to the few reported instances of synchronous anorectal mucosal melanomas. It’s rarity, non-specific symptoms and increase in incidence underscores the need for heightened clinical awareness. Limited understanding of its causes and late presentation in older patients pose diagnostic and treatment challenges. Increasing awareness in the gastroenterology community is essential for early detection, better outcomes, and avoiding misdiagnosis of this aggressive malignancy.
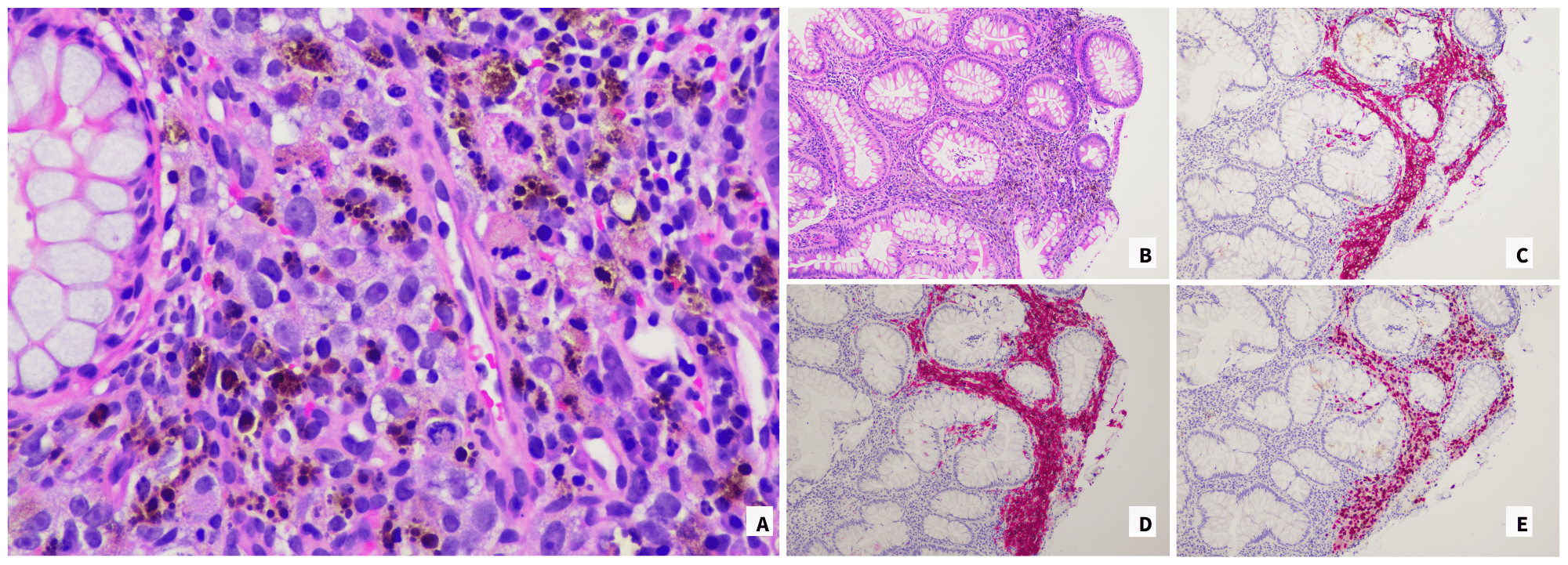
Figure: A. Sheets and nests of malignant-appearing epithelioid cells with prominent nucleoli, atypical mitoses, and conspicuous brown pigment infiltrating the rectal mucosa (H&E, original magnification 400x); B. Malignant-appearing epithelioid cells with abundant brown pigment expanding the lamina propria of the rectal mucosa (H&E, original magnification 100x); C. Malignant cells demonstrating HMB45 positivity (original magnification 100x);
D. Malignant cells demonstrating nuclear positivity for SOX10 (original magnification 100x); E. Malignant cells demonstrating MelA positivity (original magnification 100x).
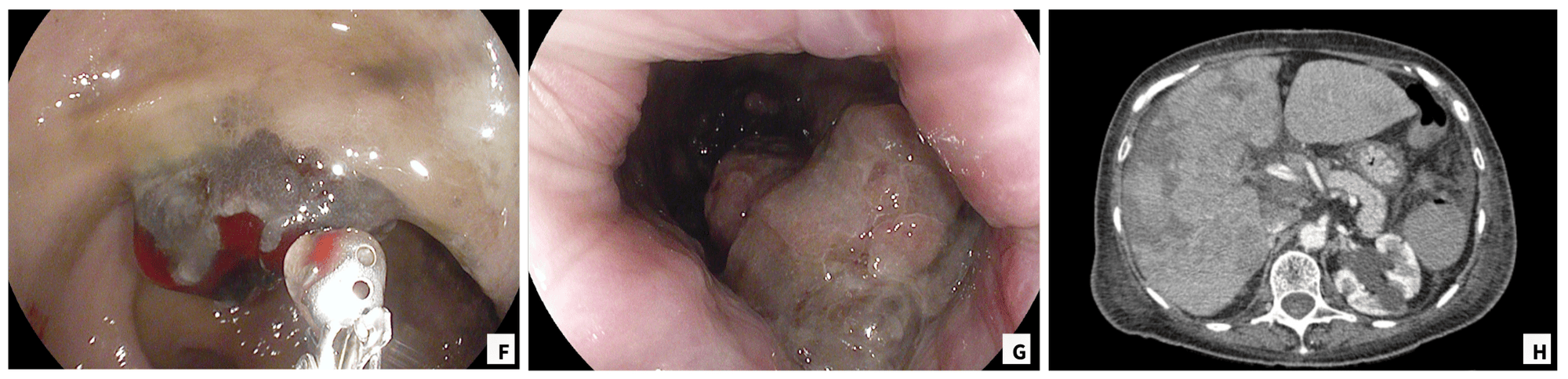
Figure: F. Black-colored polypoid lesion located 6cm from anal verge; G. Ulcerating, black-colored polypoid lesion located at the anorectal junction; H. Abdominal CT-scan with evidence of liver metastases.
Disclosures:
Natalia Rodriguez-Martino indicated no relevant financial relationships.
Jorge Cruz-Cruz indicated no relevant financial relationships.
Jose Rodríguez-León indicated no relevant financial relationships.
Natalia Rodriguez-Martino, MD1, Jorge Cruz-Cruz, MD1, Jose Rodríguez-León, MD2. P0536 - Primary Anorectal Melanoma, an Unusual Presentation With Unfavorable Prognosis: Case Report, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
