Sunday Poster Session
Category: Esophagus
P0618 - Does Low Magnesium in Veterans Make Esophageal Muscle Cramp?
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall

Christine Son, MD (she/her/hers)
Loyola University Medical Center
Maywood, IL
Presenting Author(s)
Christine Son, MD1, Promila Banerjee, MD, FACG2, Joshua Kalapala, MD3, Jeff Leya, MD4, Jill Tolentino, CGRN4, Maria Pobleti, RN4, Teri Herzog, CGRN2, Teresa Pope, RN2, Micky Dalia, LPN2, Thomas Schnell, MD2, Stephen Sontag, MD2
1Loyola University Medical Center, Maywood, IL; 2Edward Hines Jr. Veterans Affairs Hospital, Hines, IL; 3Loyola University Chicago Stritch School of Medicine, Maywood, IL; 4Edward Hines Jr. Veterans Affairs Hospital, Maywood, IL
Introduction: Magnesium (Mg) serves an essential role in neuromuscular coordination, allowing for muscle relaxation by removing calcium back into storage. Role of Mg has been well characterized in neurological disorders. Dysphagia is one of the major presenting symptoms of Mg deficiency in addition to muscle cramps and spasms. However, the role of Mg in dysphagia and spastic esophageal disorders, compared to non-spastic or normal esophageal motility, remains unclear. This is the first study to assess whether a low Mg level is associated with spastic esophageal dysmotility, especially in U.S. Veterans who are commonly deficient in Mg.
Methods: Retrospective database study was conducted at Hines VA for all Veterans referred for High-Resolution Manometry (HRM) from 2013-2024 (Medtronic Manoview ESO 3.3 software). Patterns of dysmotility in Veterans with low Mg vs. normal Mg were compared. Chronic Mg deficiency was defined as a serum Mg < 1.7 mg/dL for >1 year duration. Findings were reported as descriptive statistics.
Results: Of 476 total patients, 406 patients were male (85.3%), average age was 62.3 yrs (23 - 100), 323 White (67.9%), 112 Black (23.5%), 32 unknown (6.7%), 6 Native Americans (1.3%), and 3 Asians (0.6%). 67 (0.14%) with incomplete Mg data excluded from analysis. Most common indication for HRM was dysphagia for both low Mg & normal Mg groups (Figure 1). Of remaining 409 patients, 22.7% of patients (93 of 409) had Mg deficiency. Average Mg values were 1.61 (median 1.6, range 1.13-2, SD 0.17) in low Mg vs. 2.12 (median 2.1, range 1.73-3.04, SD 0.16) in normal Mg group. Total number of manometric diagnoses is 110 for the 93 with low Mg and 376 for 316 normal Mg with some patients having overlapping motility diagnoses. Figure 2 shows distribution of dysmotilities among low Mg vs. normal Mg.
Discussion: This study is the first to raise awareness about the role of Mg in esophageal dysmotility, especially in Veterans. 23% of Veterans at our VA presenting for manometry have hypomagnesemia. Normal Mg group was more likely to have normal manometry results. EGJOO was the most common manometric diagnosis irrespective of Mg level. IEM was the second most common diagnosis among both groups. However, among Veterans with IEM in low Mg group, spastic esophageal contractions like hypertensive UES and DES were more prevalent compared to normal Mg group (Hypertensive UES, 31.25% vs. 20%; DES, 6.25% vs. 0%). These novel associations between low Mg and esophageal spastic dysmotility warrant further studies.
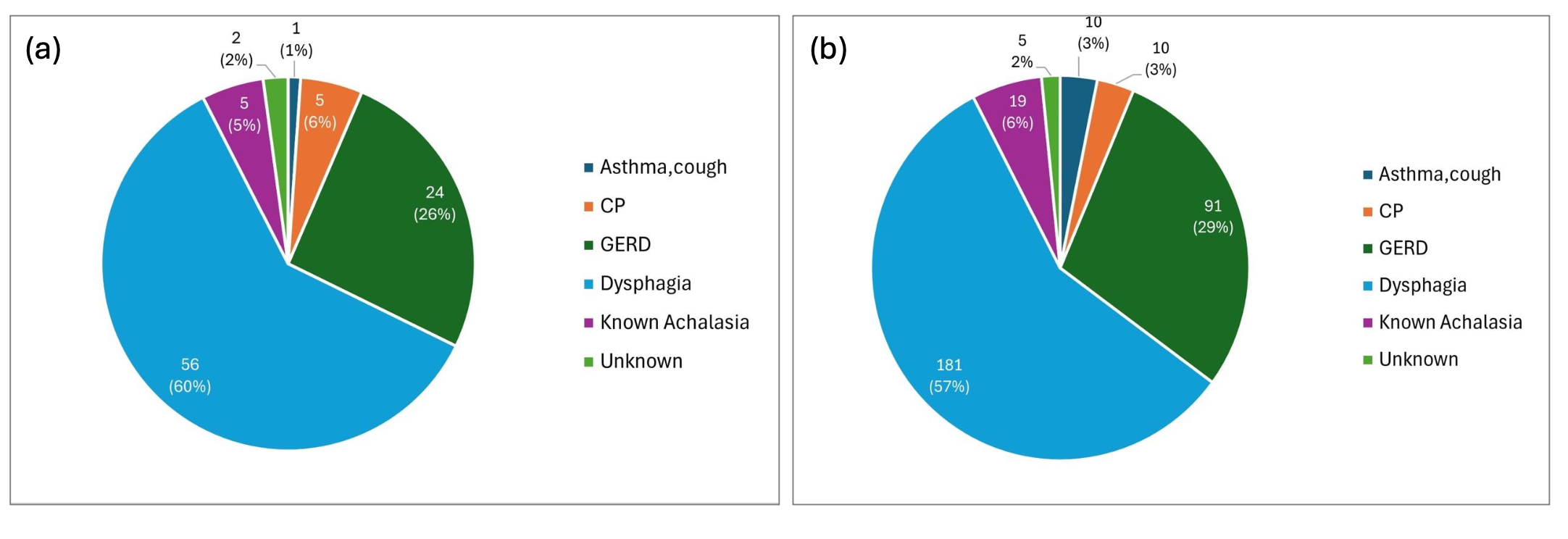
Figure: Figure 1. Distribution of Manometry Indications in Veterans with Low Mg (a) vs. Normal Mg (b).
Dysphagia was the most common indication for manometry for both groups, 60% in low Mg (a) vs. 57% in normal Mg (b).
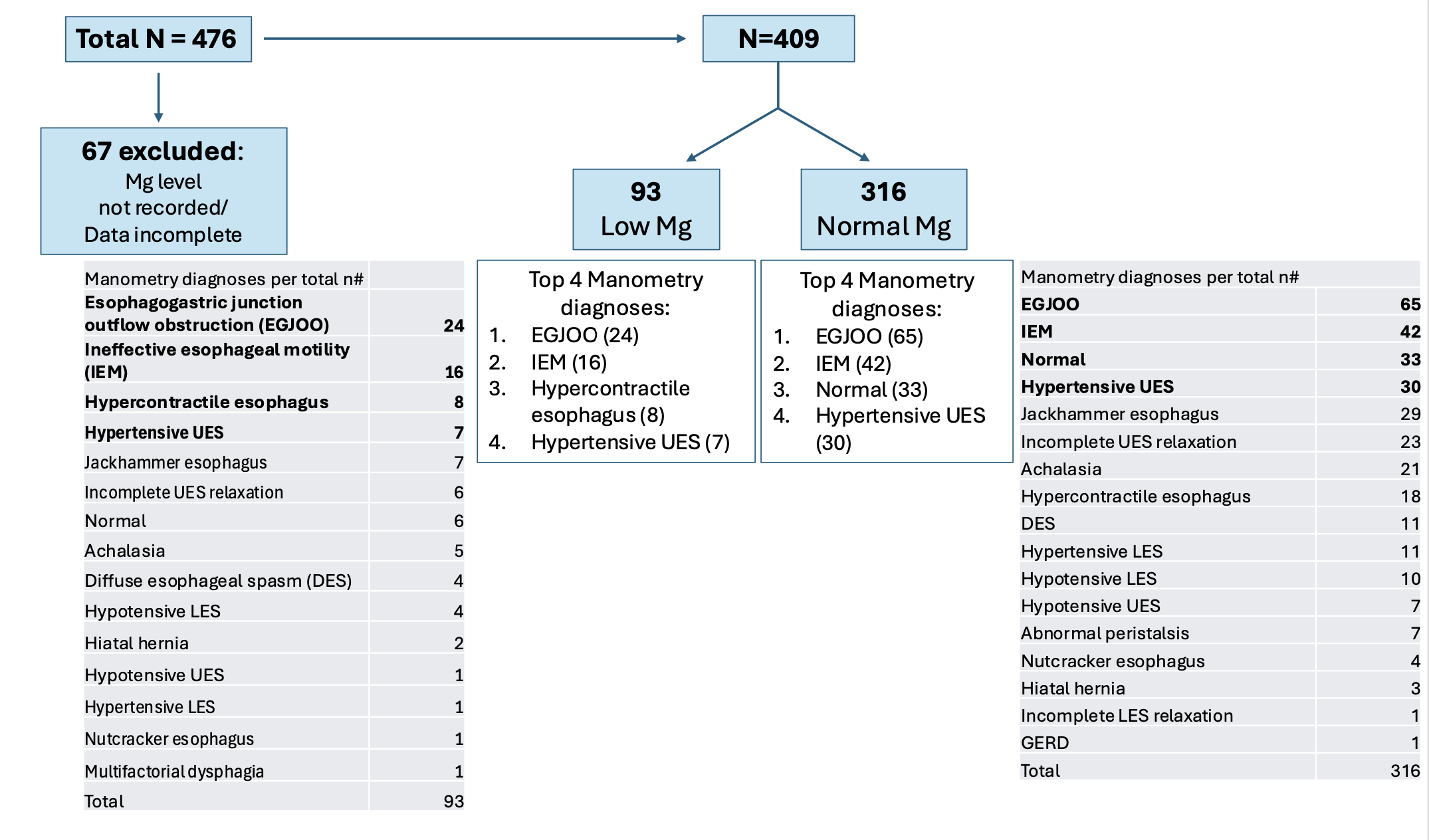
Figure: Figure 2. Distribution of Dysmotilities in Veterans with Low Mg vs. Normal Mg.
EGJOO and IEM were the top 2 manometry diagnoses for both patients with low Mg and normal Mg levels (25.8% vs. 20.6%). Normal manometry finding was observed more frequently in patients with normal Mg levels (10.4% vs. 6.5%).
Disclosures:
Christine Son indicated no relevant financial relationships.
Promila Banerjee indicated no relevant financial relationships.
Joshua Kalapala indicated no relevant financial relationships.
Jeff Leya indicated no relevant financial relationships.
Jill Tolentino indicated no relevant financial relationships.
Maria Pobleti indicated no relevant financial relationships.
Teri Herzog indicated no relevant financial relationships.
Teresa Pope indicated no relevant financial relationships.
Micky Dalia indicated no relevant financial relationships.
Thomas Schnell indicated no relevant financial relationships.
Stephen Sontag indicated no relevant financial relationships.
Christine Son, MD1, Promila Banerjee, MD, FACG2, Joshua Kalapala, MD3, Jeff Leya, MD4, Jill Tolentino, CGRN4, Maria Pobleti, RN4, Teri Herzog, CGRN2, Teresa Pope, RN2, Micky Dalia, LPN2, Thomas Schnell, MD2, Stephen Sontag, MD2. P0618 - Does Low Magnesium in Veterans Make Esophageal Muscle Cramp?, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Loyola University Medical Center, Maywood, IL; 2Edward Hines Jr. Veterans Affairs Hospital, Hines, IL; 3Loyola University Chicago Stritch School of Medicine, Maywood, IL; 4Edward Hines Jr. Veterans Affairs Hospital, Maywood, IL
Introduction: Magnesium (Mg) serves an essential role in neuromuscular coordination, allowing for muscle relaxation by removing calcium back into storage. Role of Mg has been well characterized in neurological disorders. Dysphagia is one of the major presenting symptoms of Mg deficiency in addition to muscle cramps and spasms. However, the role of Mg in dysphagia and spastic esophageal disorders, compared to non-spastic or normal esophageal motility, remains unclear. This is the first study to assess whether a low Mg level is associated with spastic esophageal dysmotility, especially in U.S. Veterans who are commonly deficient in Mg.
Methods: Retrospective database study was conducted at Hines VA for all Veterans referred for High-Resolution Manometry (HRM) from 2013-2024 (Medtronic Manoview ESO 3.3 software). Patterns of dysmotility in Veterans with low Mg vs. normal Mg were compared. Chronic Mg deficiency was defined as a serum Mg < 1.7 mg/dL for >1 year duration. Findings were reported as descriptive statistics.
Results: Of 476 total patients, 406 patients were male (85.3%), average age was 62.3 yrs (23 - 100), 323 White (67.9%), 112 Black (23.5%), 32 unknown (6.7%), 6 Native Americans (1.3%), and 3 Asians (0.6%). 67 (0.14%) with incomplete Mg data excluded from analysis. Most common indication for HRM was dysphagia for both low Mg & normal Mg groups (Figure 1). Of remaining 409 patients, 22.7% of patients (93 of 409) had Mg deficiency. Average Mg values were 1.61 (median 1.6, range 1.13-2, SD 0.17) in low Mg vs. 2.12 (median 2.1, range 1.73-3.04, SD 0.16) in normal Mg group. Total number of manometric diagnoses is 110 for the 93 with low Mg and 376 for 316 normal Mg with some patients having overlapping motility diagnoses. Figure 2 shows distribution of dysmotilities among low Mg vs. normal Mg.
Discussion: This study is the first to raise awareness about the role of Mg in esophageal dysmotility, especially in Veterans. 23% of Veterans at our VA presenting for manometry have hypomagnesemia. Normal Mg group was more likely to have normal manometry results. EGJOO was the most common manometric diagnosis irrespective of Mg level. IEM was the second most common diagnosis among both groups. However, among Veterans with IEM in low Mg group, spastic esophageal contractions like hypertensive UES and DES were more prevalent compared to normal Mg group (Hypertensive UES, 31.25% vs. 20%; DES, 6.25% vs. 0%). These novel associations between low Mg and esophageal spastic dysmotility warrant further studies.
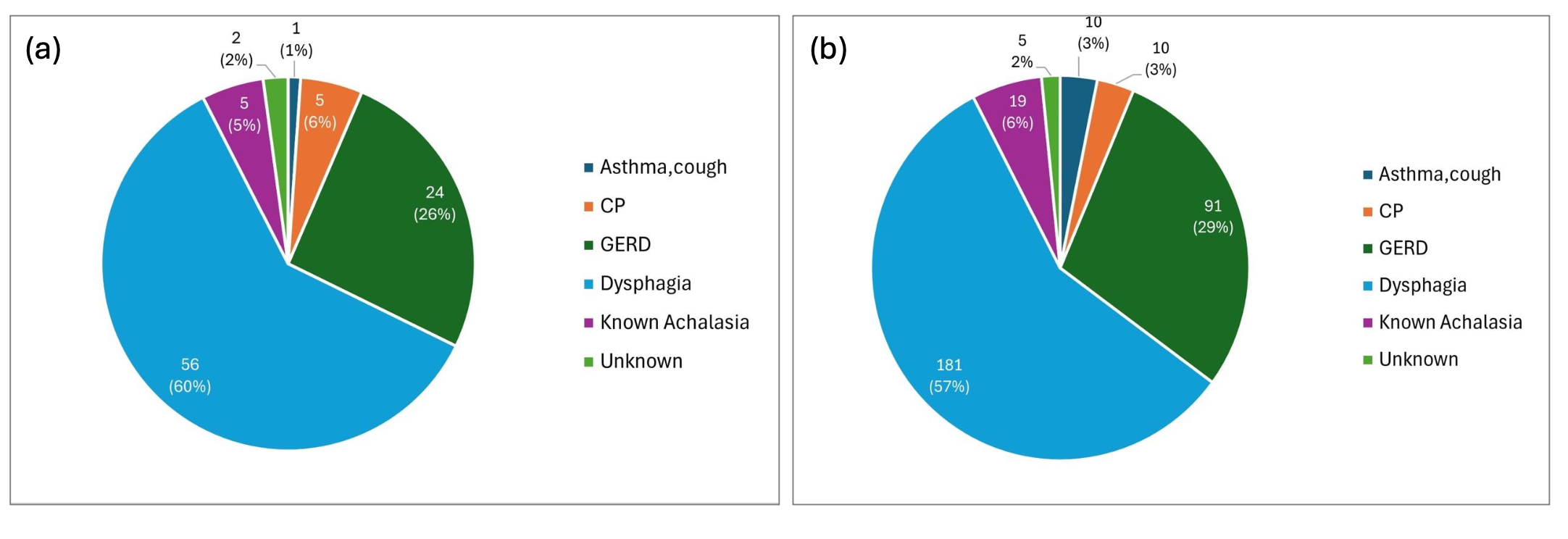
Figure: Figure 1. Distribution of Manometry Indications in Veterans with Low Mg (a) vs. Normal Mg (b).
Dysphagia was the most common indication for manometry for both groups, 60% in low Mg (a) vs. 57% in normal Mg (b).
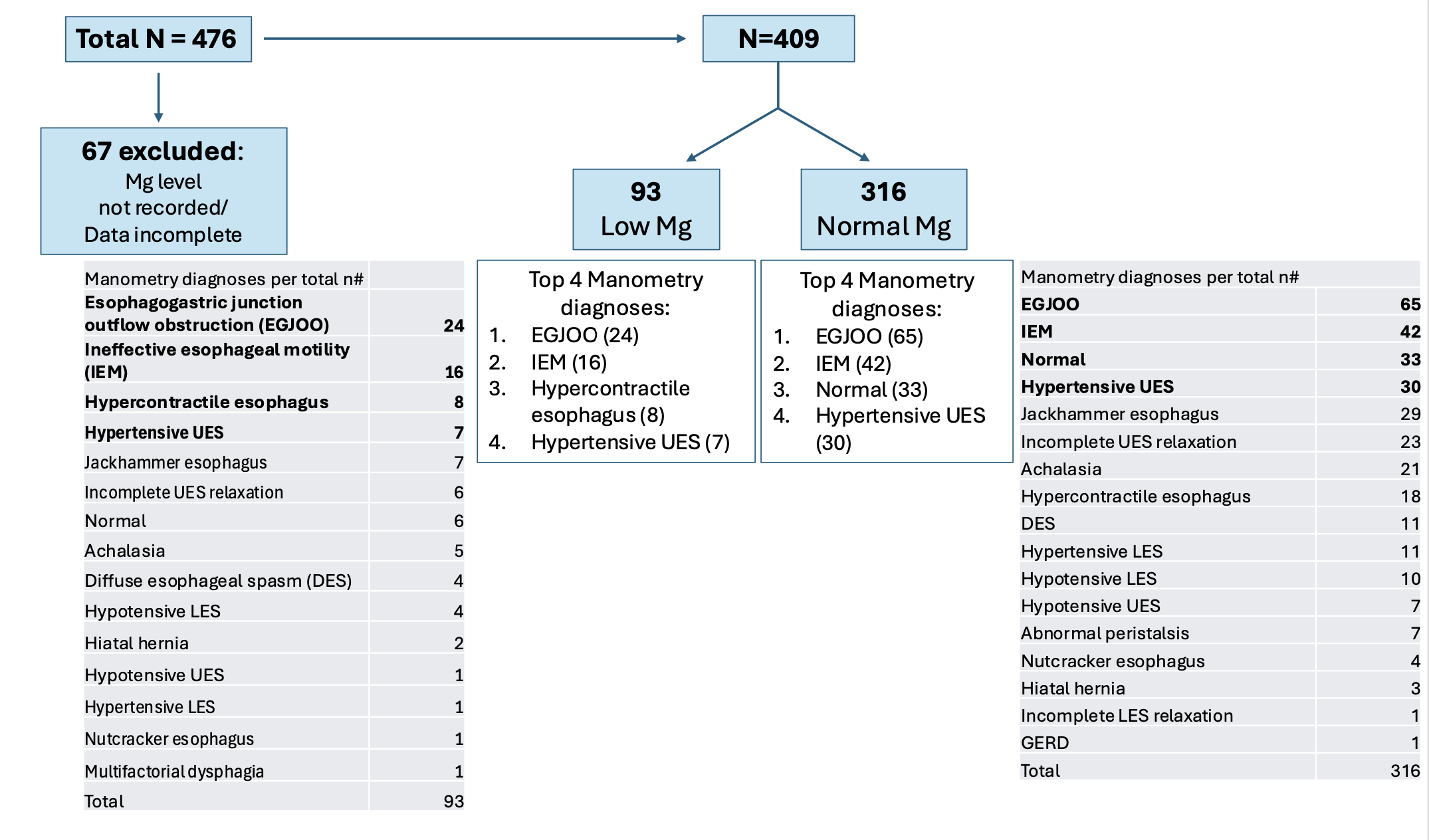
Figure: Figure 2. Distribution of Dysmotilities in Veterans with Low Mg vs. Normal Mg.
EGJOO and IEM were the top 2 manometry diagnoses for both patients with low Mg and normal Mg levels (25.8% vs. 20.6%). Normal manometry finding was observed more frequently in patients with normal Mg levels (10.4% vs. 6.5%).
Disclosures:
Christine Son indicated no relevant financial relationships.
Promila Banerjee indicated no relevant financial relationships.
Joshua Kalapala indicated no relevant financial relationships.
Jeff Leya indicated no relevant financial relationships.
Jill Tolentino indicated no relevant financial relationships.
Maria Pobleti indicated no relevant financial relationships.
Teri Herzog indicated no relevant financial relationships.
Teresa Pope indicated no relevant financial relationships.
Micky Dalia indicated no relevant financial relationships.
Thomas Schnell indicated no relevant financial relationships.
Stephen Sontag indicated no relevant financial relationships.
Christine Son, MD1, Promila Banerjee, MD, FACG2, Joshua Kalapala, MD3, Jeff Leya, MD4, Jill Tolentino, CGRN4, Maria Pobleti, RN4, Teri Herzog, CGRN2, Teresa Pope, RN2, Micky Dalia, LPN2, Thomas Schnell, MD2, Stephen Sontag, MD2. P0618 - Does Low Magnesium in Veterans Make Esophageal Muscle Cramp?, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
