Sunday Poster Session
Category: Esophagus
P0613 - Functional Lumen Imaging Probe Measurement Post-Pneumatic Dilation in Patients with Achalasia
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall

Zachary Mitchell, MD (he/him/his)
Wake Forest University School of Medicine
Winston-Salem, NC
Presenting Author(s)
Zachary Mitchell, MD1, James Miller, MD1, Elizabeth Armstrong, MD2, Robert M. Treadway, BS2, Steven B. Clayton, MD1
1Wake Forest University School of Medicine, Winston-Salem, NC; 2Atrium Health Wake Forest Baptist, Winston-Salem, NC
Introduction: Pneumatic dilation (PD) is a well-established therapeutic option for achalasia. Functional lumen impedance planimetry (FLIP) offers real-time assessment of lower esophageal sphincter (LES) distensibility and diameter. This retrospective cohort study aimed to assess whether FLIP measurements changed with symptom improvement post-PD in patients with achalasia. A secondary aim was to evaluate whether post-PD FLIP measurements correlated with the need for repeat dilation.
Methods: Patients with a confirmed diagnosis of achalasia based on manometry, timed barium esophagram (TBE), and FLIP who underwent PD were included. Pre- and post-dilation FLIP parameters, including distensibility index (DI) and diameter were recorded. Post-PD FLIP was performed during the same endoscopy session following PD. Clinical response was assessed with Eckardt scores pre-PD and post-PD. Patients were stratified based on the need for repeat PD during the follow-up period. Additional stratification was performed based on achalasia subtypes. Per guidelines for post-procedural follow-up, post-PD Eckardt scores were obtained at 6-8 week follow-up visit.
Results: A total of 21 patients were included in the study. After PD, average DI increased from 1.5 mm²/mmHg to 4.3 mm²/mmHg (p < 0.001), and diameter improved from 9.04 mm to 15.9 mm (p < 0.001). Similar post-PD changes were observed among each achalasia subtype (Table 1). The average post-PD Eckardt score was 1.78, which decreased from an average pre-PD score of 4.66. Among patients requiring repeat PD, average post-PD DI and diameter were 4.03 mm²/mmHg and 14.74 mm, respectively, which were not significantly different compared to those who did not require repeat dilation (p = 0.45, 0.14, respectively). Average Eckardt scores at 6–8 weeks were not statistically different from patients who did not require repeat dilation (p = 0.278).
Discussion: In patients with achalasia, PD is associated with improved DI and diameter as measured by FLIP, which is consistent with symptomatic improvement shown by Eckardt score. However, post-PD FLIP parameters did not identify a correlation with the need for subsequent dilation. Further investigation is warranted to establish FLIP-based thresholds that may guide treatment and follow-up planning.
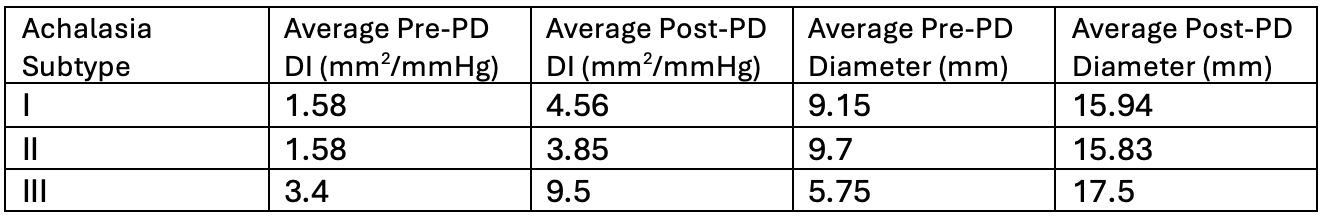
Figure: Table 1. Achalasia Subtype FLIP Measurements
Disclosures:
Zachary Mitchell indicated no relevant financial relationships.
James Miller indicated no relevant financial relationships.
Elizabeth Armstrong indicated no relevant financial relationships.
Robert Treadway indicated no relevant financial relationships.
Steven Clayton indicated no relevant financial relationships.
Zachary Mitchell, MD1, James Miller, MD1, Elizabeth Armstrong, MD2, Robert M. Treadway, BS2, Steven B. Clayton, MD1. P0613 - Functional Lumen Imaging Probe Measurement Post-Pneumatic Dilation in Patients with Achalasia, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Wake Forest University School of Medicine, Winston-Salem, NC; 2Atrium Health Wake Forest Baptist, Winston-Salem, NC
Introduction: Pneumatic dilation (PD) is a well-established therapeutic option for achalasia. Functional lumen impedance planimetry (FLIP) offers real-time assessment of lower esophageal sphincter (LES) distensibility and diameter. This retrospective cohort study aimed to assess whether FLIP measurements changed with symptom improvement post-PD in patients with achalasia. A secondary aim was to evaluate whether post-PD FLIP measurements correlated with the need for repeat dilation.
Methods: Patients with a confirmed diagnosis of achalasia based on manometry, timed barium esophagram (TBE), and FLIP who underwent PD were included. Pre- and post-dilation FLIP parameters, including distensibility index (DI) and diameter were recorded. Post-PD FLIP was performed during the same endoscopy session following PD. Clinical response was assessed with Eckardt scores pre-PD and post-PD. Patients were stratified based on the need for repeat PD during the follow-up period. Additional stratification was performed based on achalasia subtypes. Per guidelines for post-procedural follow-up, post-PD Eckardt scores were obtained at 6-8 week follow-up visit.
Results: A total of 21 patients were included in the study. After PD, average DI increased from 1.5 mm²/mmHg to 4.3 mm²/mmHg (p < 0.001), and diameter improved from 9.04 mm to 15.9 mm (p < 0.001). Similar post-PD changes were observed among each achalasia subtype (Table 1). The average post-PD Eckardt score was 1.78, which decreased from an average pre-PD score of 4.66. Among patients requiring repeat PD, average post-PD DI and diameter were 4.03 mm²/mmHg and 14.74 mm, respectively, which were not significantly different compared to those who did not require repeat dilation (p = 0.45, 0.14, respectively). Average Eckardt scores at 6–8 weeks were not statistically different from patients who did not require repeat dilation (p = 0.278).
Discussion: In patients with achalasia, PD is associated with improved DI and diameter as measured by FLIP, which is consistent with symptomatic improvement shown by Eckardt score. However, post-PD FLIP parameters did not identify a correlation with the need for subsequent dilation. Further investigation is warranted to establish FLIP-based thresholds that may guide treatment and follow-up planning.
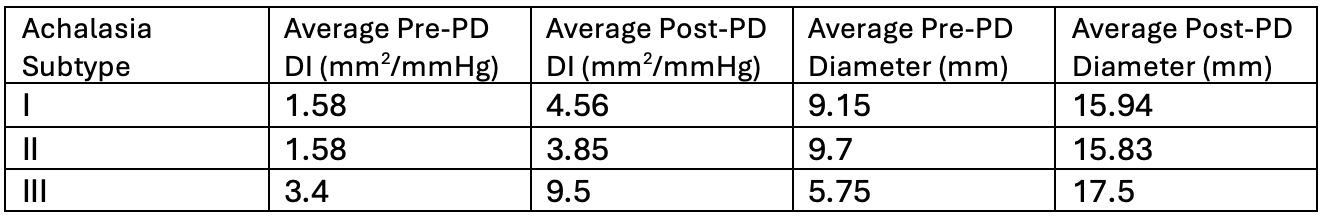
Figure: Table 1. Achalasia Subtype FLIP Measurements
Disclosures:
Zachary Mitchell indicated no relevant financial relationships.
James Miller indicated no relevant financial relationships.
Elizabeth Armstrong indicated no relevant financial relationships.
Robert Treadway indicated no relevant financial relationships.
Steven Clayton indicated no relevant financial relationships.
Zachary Mitchell, MD1, James Miller, MD1, Elizabeth Armstrong, MD2, Robert M. Treadway, BS2, Steven B. Clayton, MD1. P0613 - Functional Lumen Imaging Probe Measurement Post-Pneumatic Dilation in Patients with Achalasia, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
