Sunday Poster Session
Category: Esophagus
P0607 - Proportions and Comparative Outcomes of Post-Endoscopy Esophageal Cancer and Prevalent Esophageal Cancer: A Multi-Institutional Propensity-Matched Cohort Study
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall

Himsikhar Khataniar, MD (he/him/his)
Allegheny General Hospital
Pittsburgh, PA
Presenting Author(s)
Himsikhar Khataniar, MD1, Rahul Karna, MD2, Manal Asif, MD3, Mohammad Bilal, MD, FACG4
1Allegheny General Hospital, Pittsburgh, PA; 2University of Minnesota Medical Center, Minneapolis, MN; 3Kabir Medical College, Peshawar, North-West Frontier, Pakistan; 4University of Colorado Anschutz Medical Campus, Denver, CO
Introduction: Despite high quality esophagogastroduodenoscopy in patients with Barrett’s esophagus (BE), post endoscopy esophageal cancer (PEEC) can occur due to missed lesions or rapidly growing tumors. It’s unknown if PEEC has different natural history and course of disease compared to esophageal cancer (EC) diagnosed at endoscopy. We aim to assess 5- year outcomes of PEEC compared to prevalent esophageal cancer (EC).
Methods: We queried the TriNetX U.S. Collaborative Network for adults (18–90 yr) given an ICD code for EC between June 2005 and June 2025. PEEC was defined as EC in which an EGD occurred 6–36 months before diagnosis in which no EC was detected, while the diagnosis of prevalent EC required an EGD within the preceding 6 months. Patients of both the cohorts needed to have a diagnosis of Barrett’s esophagus without dysplasia atleast 6 months before the diagnosis of EC. Patients with any prior malignancies, major surgeries were excluded. Outcomes (esophagectomy, chemotherapy, radiation, hospitalization, mortality) were tracked from the index cancer date to 5 years. Propensity scores incorporating age, sex, race/ethnicity, cardiometabolic disease and smoking were matched 1:1 and Cox models generated hazard ratios (HR) with 95% CIs.
Results: Among 830 ECs recorded during the last three years, 134 met PEEC criteria, with an overall proportion of 16.1%. Baseline characteristics of included population is demonstrated in Table 1. After propensity score matching, 126 patients were included for outcome assessment in PEEC and prevalent EC cohort. PEEC was associated with a greater need for systemic therapy: 5-year chemotherapy HR 1.88 (1.04–3.39, P = 0.033) and radiotherapy(HR 2.39, 0.97–5.87). Risks were directionally higher, though nonsignificant, for esophagectomy HR 1.20 (0.51–2.83), hospitalization HR 1.48 (0.81–2.72) and mortality HR 1.32 (0.80–2.20) [Table 2].
Discussion: In a large U.S. real-world cohort, one in six esophageal cancers qualified as PEEC and demonstrated higher odds of chemotherapy and radiotherapy with uptrend in odds of esophagectomy and mortality. Our study suggests aggressive tumor biology of PEEC may be possible reason for greater need for chemo-radiotherapy compared to prevalent EC.
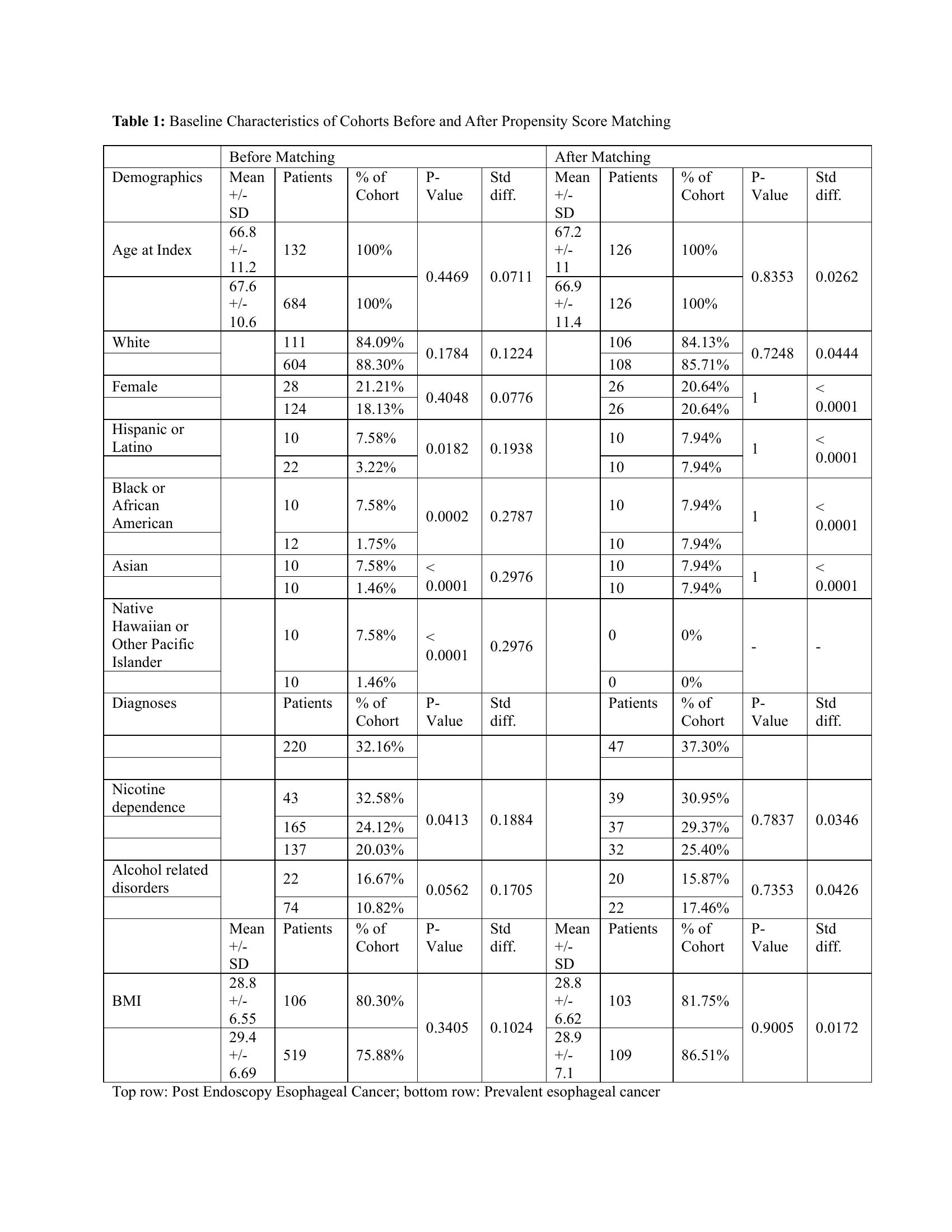
Figure: Table 1: Baseline Characteristics of Cohorts Before and After Propensity Score Matching
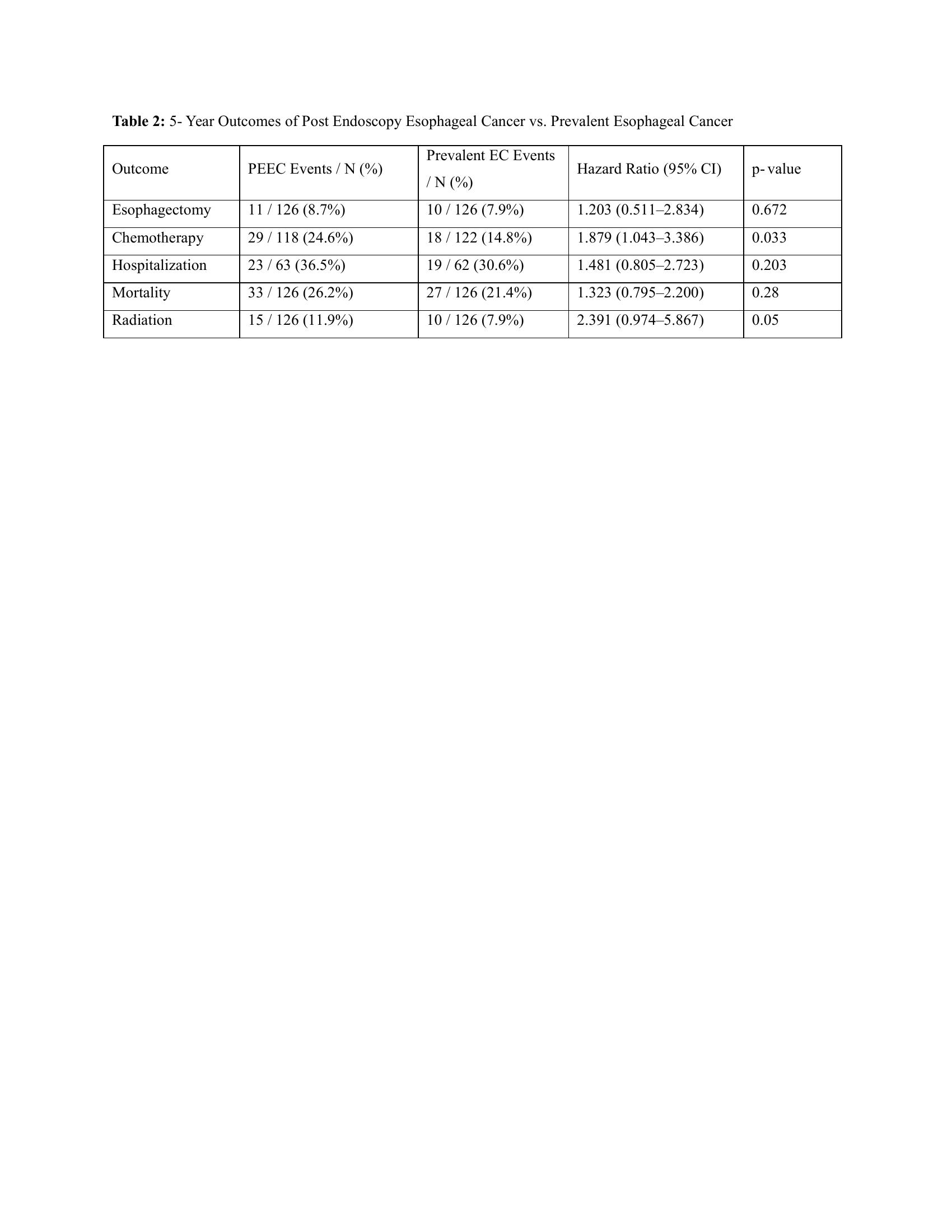
Figure: Table 2: 5- Year Outcomes of Post Endoscopy Esophageal Cancer vs. Prevalent Esophageal Cancer
Disclosures:
Himsikhar Khataniar indicated no relevant financial relationships.
Rahul Karna indicated no relevant financial relationships.
Manal Asif indicated no relevant financial relationships.
Mohammad Bilal: Boston Scientific – Consultant. Cook endoscopy – Paid speaker. Steris Endoscopy – Consultant.
Himsikhar Khataniar, MD1, Rahul Karna, MD2, Manal Asif, MD3, Mohammad Bilal, MD, FACG4. P0607 - Proportions and Comparative Outcomes of Post-Endoscopy Esophageal Cancer and Prevalent Esophageal Cancer: A Multi-Institutional Propensity-Matched Cohort Study, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Allegheny General Hospital, Pittsburgh, PA; 2University of Minnesota Medical Center, Minneapolis, MN; 3Kabir Medical College, Peshawar, North-West Frontier, Pakistan; 4University of Colorado Anschutz Medical Campus, Denver, CO
Introduction: Despite high quality esophagogastroduodenoscopy in patients with Barrett’s esophagus (BE), post endoscopy esophageal cancer (PEEC) can occur due to missed lesions or rapidly growing tumors. It’s unknown if PEEC has different natural history and course of disease compared to esophageal cancer (EC) diagnosed at endoscopy. We aim to assess 5- year outcomes of PEEC compared to prevalent esophageal cancer (EC).
Methods: We queried the TriNetX U.S. Collaborative Network for adults (18–90 yr) given an ICD code for EC between June 2005 and June 2025. PEEC was defined as EC in which an EGD occurred 6–36 months before diagnosis in which no EC was detected, while the diagnosis of prevalent EC required an EGD within the preceding 6 months. Patients of both the cohorts needed to have a diagnosis of Barrett’s esophagus without dysplasia atleast 6 months before the diagnosis of EC. Patients with any prior malignancies, major surgeries were excluded. Outcomes (esophagectomy, chemotherapy, radiation, hospitalization, mortality) were tracked from the index cancer date to 5 years. Propensity scores incorporating age, sex, race/ethnicity, cardiometabolic disease and smoking were matched 1:1 and Cox models generated hazard ratios (HR) with 95% CIs.
Results: Among 830 ECs recorded during the last three years, 134 met PEEC criteria, with an overall proportion of 16.1%. Baseline characteristics of included population is demonstrated in Table 1. After propensity score matching, 126 patients were included for outcome assessment in PEEC and prevalent EC cohort. PEEC was associated with a greater need for systemic therapy: 5-year chemotherapy HR 1.88 (1.04–3.39, P = 0.033) and radiotherapy(HR 2.39, 0.97–5.87). Risks were directionally higher, though nonsignificant, for esophagectomy HR 1.20 (0.51–2.83), hospitalization HR 1.48 (0.81–2.72) and mortality HR 1.32 (0.80–2.20) [Table 2].
Discussion: In a large U.S. real-world cohort, one in six esophageal cancers qualified as PEEC and demonstrated higher odds of chemotherapy and radiotherapy with uptrend in odds of esophagectomy and mortality. Our study suggests aggressive tumor biology of PEEC may be possible reason for greater need for chemo-radiotherapy compared to prevalent EC.
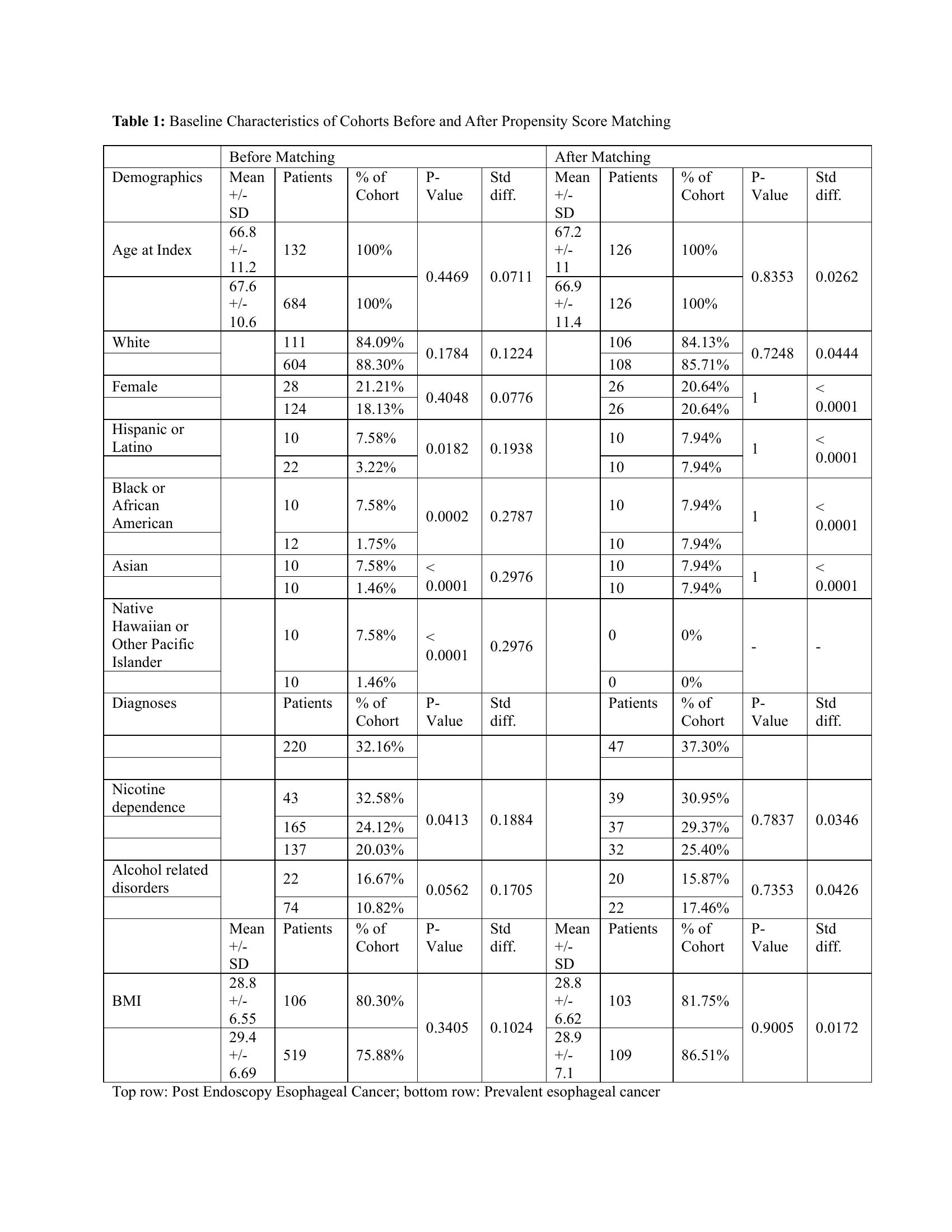
Figure: Table 1: Baseline Characteristics of Cohorts Before and After Propensity Score Matching
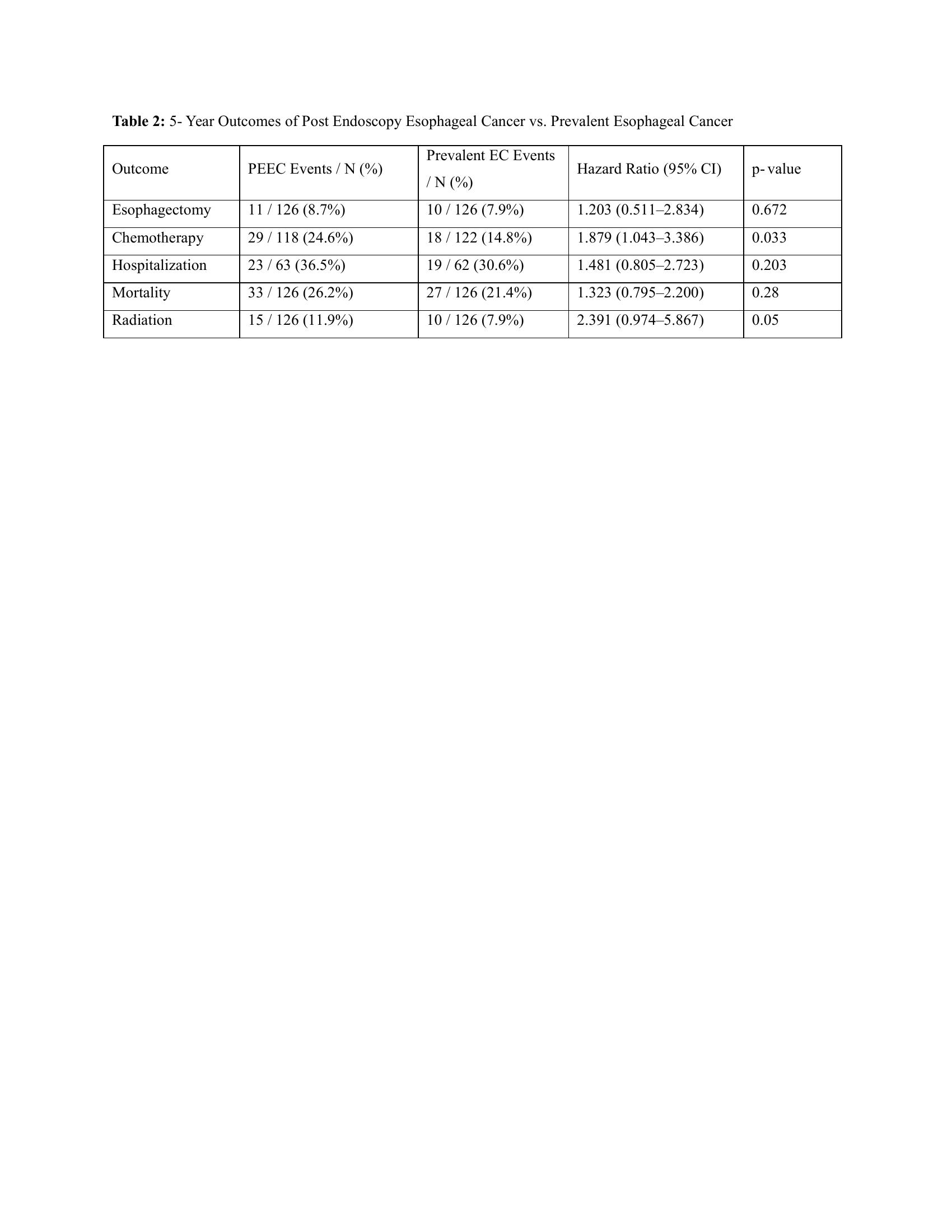
Figure: Table 2: 5- Year Outcomes of Post Endoscopy Esophageal Cancer vs. Prevalent Esophageal Cancer
Disclosures:
Himsikhar Khataniar indicated no relevant financial relationships.
Rahul Karna indicated no relevant financial relationships.
Manal Asif indicated no relevant financial relationships.
Mohammad Bilal: Boston Scientific – Consultant. Cook endoscopy – Paid speaker. Steris Endoscopy – Consultant.
Himsikhar Khataniar, MD1, Rahul Karna, MD2, Manal Asif, MD3, Mohammad Bilal, MD, FACG4. P0607 - Proportions and Comparative Outcomes of Post-Endoscopy Esophageal Cancer and Prevalent Esophageal Cancer: A Multi-Institutional Propensity-Matched Cohort Study, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
