Sunday Poster Session
Category: Esophagus
P0700 - Acute Esophageal Necrosis in the Elderly: The Dark Consequence of Hypoperfusion
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall

Gretchen C. Abarca-Riancho, MD (she/her/hers)
Damas Hospital
Guaynabo, PR
Presenting Author(s)
Gretchen C.. Abarca-Riancho, MD1, Lorimar Rodriguez, MD2, Milton M.. Rivera, MD2, Reinaldo Ramirez, MD2, Carlos Rosario, MD2
1Damas Hospital, Guaynabo, Puerto Rico; 2Damas Hospital, Ponce, Puerto Rico
Introduction: Acute esophageal necrosis (AEN) or black “esophagus” is a rare and serious condition with circumferential black discoloration of the distal esophagus mucosa with sharp demarcation at the gastroesophageal (GE) junction. Its pathogenesis is multifactorial, involving systemic hypoperfusion, impaired mucosal defenses, and gastric reflux. Other factors include microbial colonization (e.g., nasogastric tube, sepsis) and ischemia-reperfusion injury. AEN commonly occurs in critically ill patients, especially in shock, malnutrition, sepsis, or comorbidities like, diabetes, hypertension, and chronic kidney disease. Prevalence ranges from 0.1%-0.28% of endoscopies, highlighting its rarity despite severity. Mortality is 30%-35%, mainly due underlying illness.
Case Description/
Methods: An 85 y/o female with type 2 diabetes, hypertension, hypothyroidism, anemia, and multiple pressure ulcers admitted due to infected sacral ulcer. On hospital day three, the patient developed hematemesis followed by melena over the next three days. Appeared pale and chronically ill, with abdominal tenderness, dry oral mucosa, a nasogastric tube (NGT). She was kept nothing per mouth (NPO), NGT removed, and high-dose proton pump inhibitors (PPIs) started. Esophagogastroduodenoscopy (EGD) was placed once stable.
During this time, she had persistent hypotension (SBP 72-102 mmHg, DBP as low as 48 mmHg), and hemoglobin drop from 9.7 to 71. G/dL over 4 days. On hospital day seven, EGD showed black mucosal discoloration of the mid to distal esophagus with clear transition at GE junction, classic for AEN (Fig. 1). The stomach was unremarkable, but two large duodenal ulcers with hematin deposits were noted (Fig. 2). No biopsies were taken.
The patient received conservative treatment, including IV fluids, blood transfusions, IV PPIs, antibiotics and bowel rest. Despite management, her condition worsened and she died from progressive hemodynamic instability and multiorgan failure.
Discussion: AEN is a rare but severe disorder with distinctive endoscopic findings. In this case multiple risk factors like advanced age, diabetes, malnutrition, and hypotension, likely caused esophageal ischemia. Duodenal ulcers may have worsened bleeding and perfusion. While biopsy may aid with diagnosis, it is unnecessary when clinical and endoscopic findings are classic. Management is supportive, but prognosis depends on underlying illness. This case highlights the importance of early recognition and vigilance in high-risk patients with upper GI bleeding.
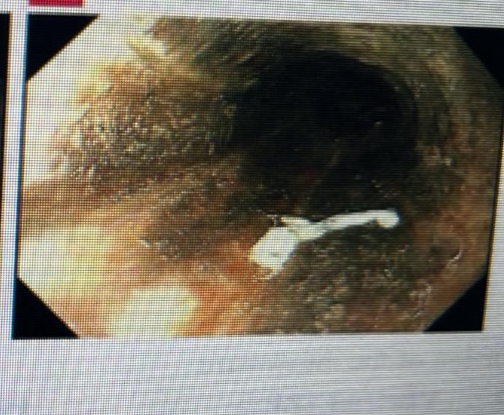
Figure: Esophageal necrosis
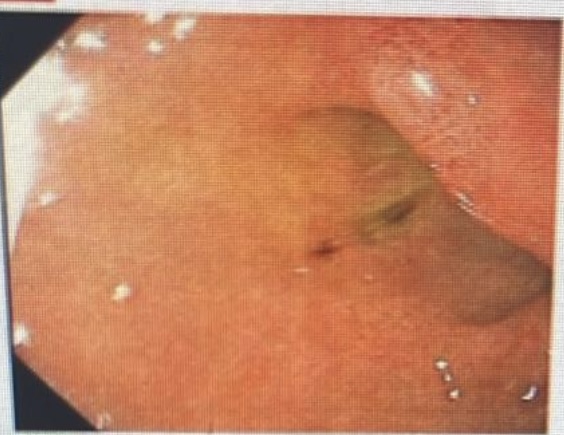
Figure: Duodenal ulcer
Disclosures:
Gretchen Abarca-Riancho indicated no relevant financial relationships.
Lorimar Rodriguez indicated no relevant financial relationships.
Milton Rivera indicated no relevant financial relationships.
Reinaldo Ramirez indicated no relevant financial relationships.
Carlos Rosario indicated no relevant financial relationships.
Gretchen C.. Abarca-Riancho, MD1, Lorimar Rodriguez, MD2, Milton M.. Rivera, MD2, Reinaldo Ramirez, MD2, Carlos Rosario, MD2. P0700 - Acute Esophageal Necrosis in the Elderly: The Dark Consequence of Hypoperfusion, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Damas Hospital, Guaynabo, Puerto Rico; 2Damas Hospital, Ponce, Puerto Rico
Introduction: Acute esophageal necrosis (AEN) or black “esophagus” is a rare and serious condition with circumferential black discoloration of the distal esophagus mucosa with sharp demarcation at the gastroesophageal (GE) junction. Its pathogenesis is multifactorial, involving systemic hypoperfusion, impaired mucosal defenses, and gastric reflux. Other factors include microbial colonization (e.g., nasogastric tube, sepsis) and ischemia-reperfusion injury. AEN commonly occurs in critically ill patients, especially in shock, malnutrition, sepsis, or comorbidities like, diabetes, hypertension, and chronic kidney disease. Prevalence ranges from 0.1%-0.28% of endoscopies, highlighting its rarity despite severity. Mortality is 30%-35%, mainly due underlying illness.
Case Description/
Methods: An 85 y/o female with type 2 diabetes, hypertension, hypothyroidism, anemia, and multiple pressure ulcers admitted due to infected sacral ulcer. On hospital day three, the patient developed hematemesis followed by melena over the next three days. Appeared pale and chronically ill, with abdominal tenderness, dry oral mucosa, a nasogastric tube (NGT). She was kept nothing per mouth (NPO), NGT removed, and high-dose proton pump inhibitors (PPIs) started. Esophagogastroduodenoscopy (EGD) was placed once stable.
During this time, she had persistent hypotension (SBP 72-102 mmHg, DBP as low as 48 mmHg), and hemoglobin drop from 9.7 to 71. G/dL over 4 days. On hospital day seven, EGD showed black mucosal discoloration of the mid to distal esophagus with clear transition at GE junction, classic for AEN (Fig. 1). The stomach was unremarkable, but two large duodenal ulcers with hematin deposits were noted (Fig. 2). No biopsies were taken.
The patient received conservative treatment, including IV fluids, blood transfusions, IV PPIs, antibiotics and bowel rest. Despite management, her condition worsened and she died from progressive hemodynamic instability and multiorgan failure.
Discussion: AEN is a rare but severe disorder with distinctive endoscopic findings. In this case multiple risk factors like advanced age, diabetes, malnutrition, and hypotension, likely caused esophageal ischemia. Duodenal ulcers may have worsened bleeding and perfusion. While biopsy may aid with diagnosis, it is unnecessary when clinical and endoscopic findings are classic. Management is supportive, but prognosis depends on underlying illness. This case highlights the importance of early recognition and vigilance in high-risk patients with upper GI bleeding.
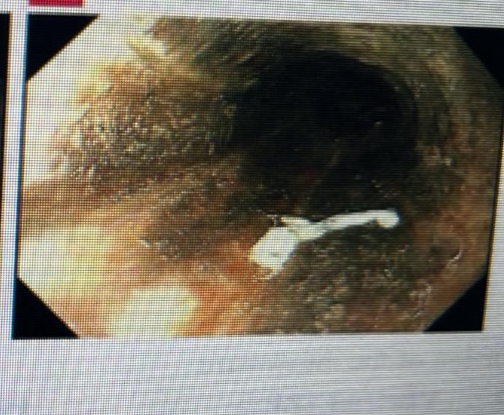
Figure: Esophageal necrosis
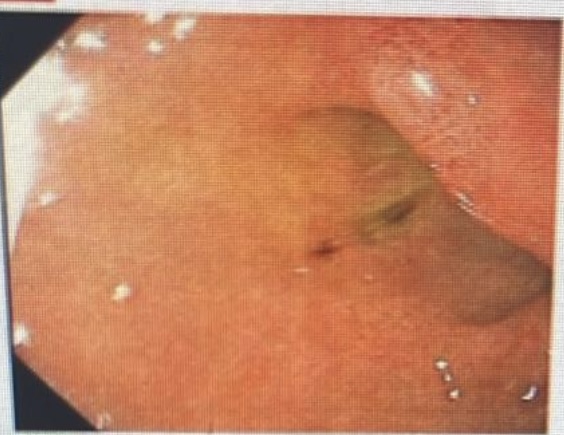
Figure: Duodenal ulcer
Disclosures:
Gretchen Abarca-Riancho indicated no relevant financial relationships.
Lorimar Rodriguez indicated no relevant financial relationships.
Milton Rivera indicated no relevant financial relationships.
Reinaldo Ramirez indicated no relevant financial relationships.
Carlos Rosario indicated no relevant financial relationships.
Gretchen C.. Abarca-Riancho, MD1, Lorimar Rodriguez, MD2, Milton M.. Rivera, MD2, Reinaldo Ramirez, MD2, Carlos Rosario, MD2. P0700 - Acute Esophageal Necrosis in the Elderly: The Dark Consequence of Hypoperfusion, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
