Sunday Poster Session
Category: Esophagus
P0699 - Sealing the Leak: Esophageal Stent for a Mysterious Micro-Perforation
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall

Mohsin Chundrigar, MBBS (he/him/his)
Albany Medical Center
Albany, NY
Presenting Author(s)
Mohsin Chundrigar, MBBS, Anthony Passarella, MD, Shamayel Safdar, MBBS, Zarbakht Nisar, MBBS, T. Charles Martin, DO
Albany Medical Center, Albany, NY
Introduction: Anastomotic leaks are serious complications of gastrointestinal surgery and may remain undetectable despite multiple diagnostic evaluations. Persistent fluid collections with enteric characteristics can raise suspicion for a leak without confirmatory imaging. This case highlights how empiric esophageal stenting resulted in clinical resolution and illustrates limitations of conventional modalities in detecting post-surgical GI leaks.
Case Description/
Methods: A 58-year-old woman with prior Roux-en-Y gastric bypass developed persistent left pleural and perisplenic fluid collections. Despite serial percutaneous drainage and broad-spectrum antibiotics, collections remained refractory. Diagnostic workup included three upper GI series, three EGDs, and multiple CT scans without evidence of anastomotic leak. However, aspirated perisplenic fluid revealed rare enteric flora, few cutaneous organisms, and 4+ polymorphonuclear leukocytes per low-power field, raising concern for occult gastrointestinal contamination. Given proximity to the gastrojejunal anastomosis and persistent clinical concern, a fully covered esophageal stent (18mmx97mm) was placed empirically across the anastomosis. The patient demonstrated marked clinical improvement, with resolution of pleural drainage, significant reduction in perisplenic collections, and successful oral intake. She was weaned off antibiotics and discharged without further interventions.
Discussion: Anastomotic leaks are serious events requiring drainage and source control. Stent placement supports source control by diverting luminal contents away from the leak site. However, conventional diagnostics may fail to detect subtle or intermittent leaks, limiting their reliability. In this case, repeated imaging and endoscopy were negative despite persistent, anatomically suggestive collections and enteric organisms. High clinical suspicion, coupled with ongoing fluid reaccumulation, led to empiric stent placement. The intervention resulted in clear clinical improvement and resolution of refractory collections. This case shows that early empiric stenting should be considered in well-selected patients with high clinical suspicion and persistent imaging findings, even when conventional modalities are inconclusive. It highlights the role of clinical judgment in leak detection and demonstrates the need for further studies to define selection criteria for empiric stent use in occult gastrointestinal leaks.
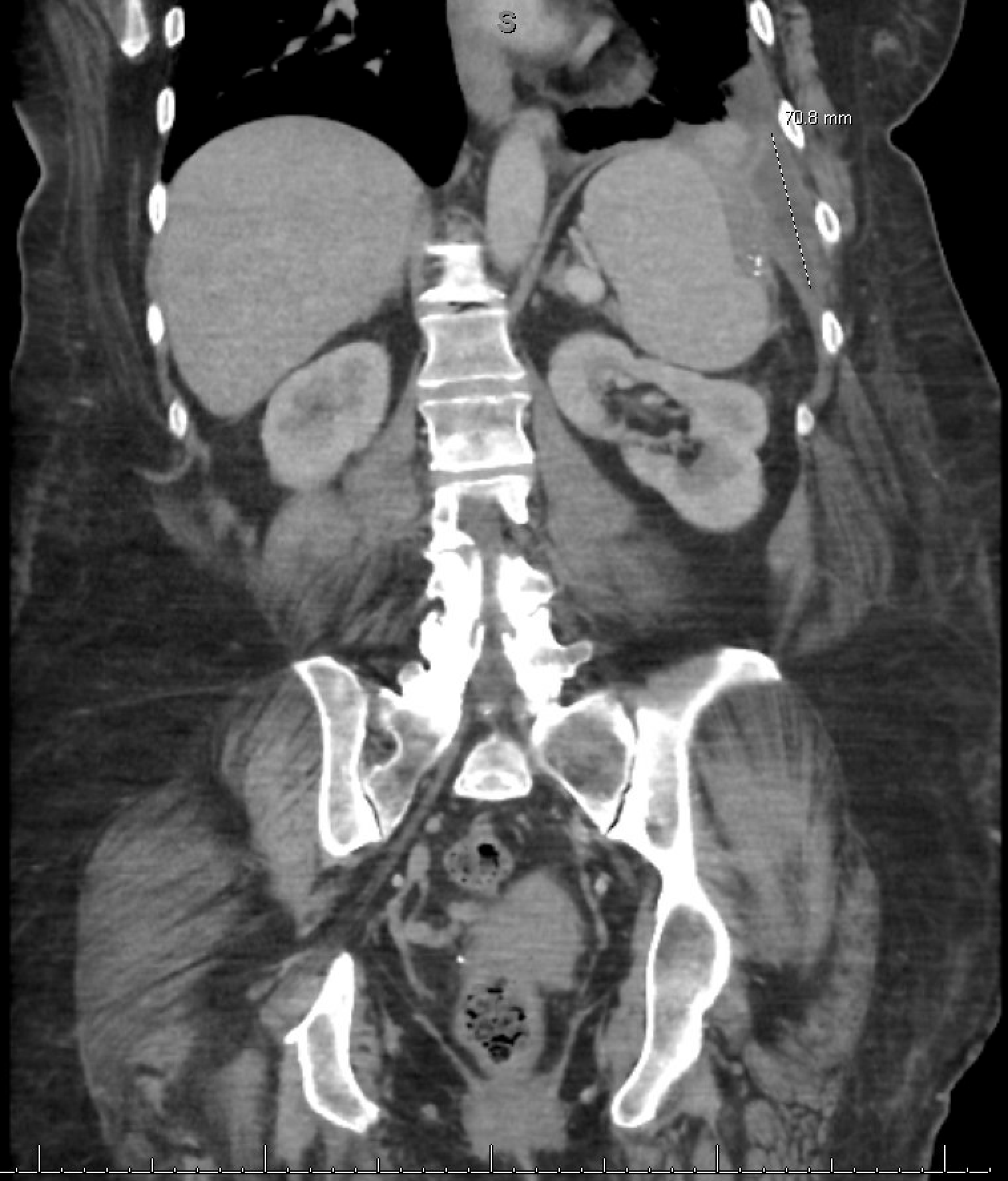
Figure: CT scan of the abdomen demonstrating perisplenic fluid collection prior to stent placement.

Figure: CT scan of the abdomen demonstrating perisplenic fluid collection post stent placement.
Disclosures:
Mohsin Chundrigar indicated no relevant financial relationships.
Anthony Passarella indicated no relevant financial relationships.
Shamayel Safdar indicated no relevant financial relationships.
Zarbakht Nisar indicated no relevant financial relationships.
T. Charles Martin indicated no relevant financial relationships.
Mohsin Chundrigar, MBBS, Anthony Passarella, MD, Shamayel Safdar, MBBS, Zarbakht Nisar, MBBS, T. Charles Martin, DO. P0699 - Sealing the Leak: Esophageal Stent for a Mysterious Micro-Perforation, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
Albany Medical Center, Albany, NY
Introduction: Anastomotic leaks are serious complications of gastrointestinal surgery and may remain undetectable despite multiple diagnostic evaluations. Persistent fluid collections with enteric characteristics can raise suspicion for a leak without confirmatory imaging. This case highlights how empiric esophageal stenting resulted in clinical resolution and illustrates limitations of conventional modalities in detecting post-surgical GI leaks.
Case Description/
Methods: A 58-year-old woman with prior Roux-en-Y gastric bypass developed persistent left pleural and perisplenic fluid collections. Despite serial percutaneous drainage and broad-spectrum antibiotics, collections remained refractory. Diagnostic workup included three upper GI series, three EGDs, and multiple CT scans without evidence of anastomotic leak. However, aspirated perisplenic fluid revealed rare enteric flora, few cutaneous organisms, and 4+ polymorphonuclear leukocytes per low-power field, raising concern for occult gastrointestinal contamination. Given proximity to the gastrojejunal anastomosis and persistent clinical concern, a fully covered esophageal stent (18mmx97mm) was placed empirically across the anastomosis. The patient demonstrated marked clinical improvement, with resolution of pleural drainage, significant reduction in perisplenic collections, and successful oral intake. She was weaned off antibiotics and discharged without further interventions.
Discussion: Anastomotic leaks are serious events requiring drainage and source control. Stent placement supports source control by diverting luminal contents away from the leak site. However, conventional diagnostics may fail to detect subtle or intermittent leaks, limiting their reliability. In this case, repeated imaging and endoscopy were negative despite persistent, anatomically suggestive collections and enteric organisms. High clinical suspicion, coupled with ongoing fluid reaccumulation, led to empiric stent placement. The intervention resulted in clear clinical improvement and resolution of refractory collections. This case shows that early empiric stenting should be considered in well-selected patients with high clinical suspicion and persistent imaging findings, even when conventional modalities are inconclusive. It highlights the role of clinical judgment in leak detection and demonstrates the need for further studies to define selection criteria for empiric stent use in occult gastrointestinal leaks.
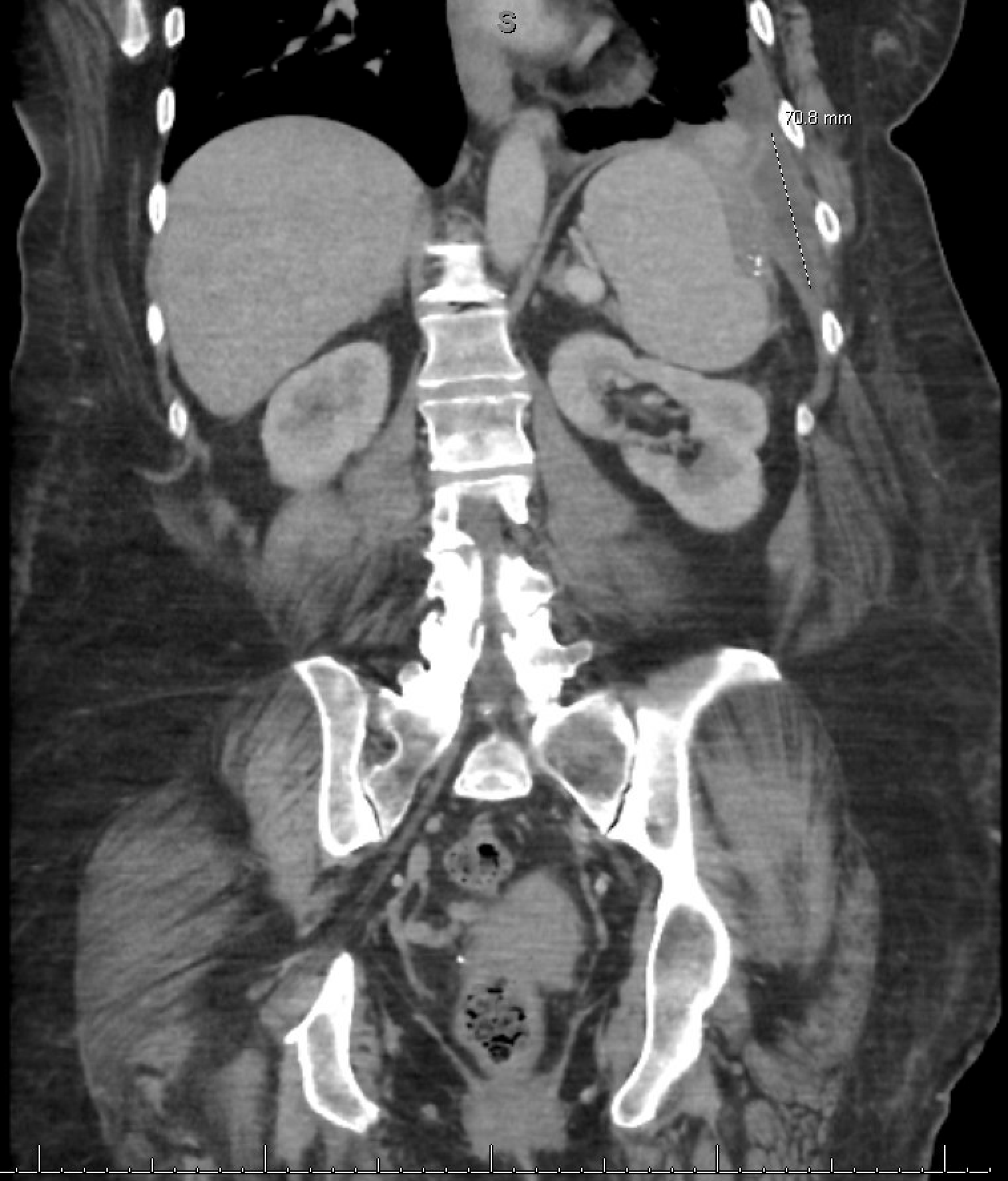
Figure: CT scan of the abdomen demonstrating perisplenic fluid collection prior to stent placement.

Figure: CT scan of the abdomen demonstrating perisplenic fluid collection post stent placement.
Disclosures:
Mohsin Chundrigar indicated no relevant financial relationships.
Anthony Passarella indicated no relevant financial relationships.
Shamayel Safdar indicated no relevant financial relationships.
Zarbakht Nisar indicated no relevant financial relationships.
T. Charles Martin indicated no relevant financial relationships.
Mohsin Chundrigar, MBBS, Anthony Passarella, MD, Shamayel Safdar, MBBS, Zarbakht Nisar, MBBS, T. Charles Martin, DO. P0699 - Sealing the Leak: Esophageal Stent for a Mysterious Micro-Perforation, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
