Sunday Poster Session
Category: Esophagus
P0697 - Black Esophagus in a Nonagenarian With Hematemesis: A Case of Acute Esophageal Necrosis With Mucosal Recovery
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall

Lan Nguyen, DO
University at Buffalo
Buffalo, NY
Presenting Author(s)
Mohammed Ayyad, MD1, Lan Nguyen, DO2, Maram Albandak, MD, MPH3, Joshua E. Pagán-Busigó, MD4, Rajiv Pulinthanathu, MD5, Dhanasekaran Ramasamy, MD1, Shiva Kumar, MD6
1Rutgers New Jersey Medical School, Newark, NJ; 2University at Buffalo, Buffalo, NY; 3Department of Internal Medicine, The University of Toledo, Toledo, OH, USA, Toledo, OH; 4Rutgers New Jersey Medical School, Kearny, NJ; 5Rutgers Robert Wood Johnson University Hospital, Newark, NJ; 6Cleveland Clinic Abu Dhabi, Cleveland, OH
Introduction: Acute esophageal necrosis (AEN), also known as "black esophagus," is a rare but serious manifestation of ischemic injury to the esophagus. It is characterized by diffuse circumferential black discoloration of the esophageal mucosa, most commonly affecting the distal esophagus with varying degrees of proximal extension. AEN is often multifactorial in origin, resulting from systemic hypoperfusion and critical illness that compromise mucosal integrity. Early recognition and timely supportive management are essential, particularly in patients with complex comorbidities that impair tissue perfusion.
Case Description/
Methods: A 93-year-old male with multiple co-morbid conditions of atrial fibrillation on anticoagulation, congestive heart failure, pulmonary hypertension, diabetes mellitus, and severe aortic stenosis presented with coffee-ground emesis and melena. Emergent esophagogastroduodenoscopy (EGD) revealed a confluence of necrotic-appearing mucosa in the mid-to-distal esophagus suggestive of AEN. Biopsies were obtained, which confirmed severe acute inflammation with prominent brown-black pigment deposition, consistent with necrotic tissue. The patient was managed conservatively with intravenous pantoprazole, total parenteral nutrition, hydration, and optimization of his underlying comorbidities. Given his advanced age and medical complexity, surgical intervention was deferred. Close hemodynamic monitoring and supportive management resulted in clinical stabilization and gradual recovery. A repeat EGD on day 7 demonstrated substantial mucosal healing. The patient was discharged on oral proton pump inhibitor therapy and has remained clinically stable without readmission.
Discussion: This case highlights the importance of recognizing AEN in the appropriate clinical context and compatible endoscopic findings. Co-morbid conditions such as heart failure, aortic stenosis, and atrial fibrillation can compromise esophageal perfusion and impair mucosal defenses, increasing susceptibility to ischemic injury. Management of AEN involves not only measures to hasten mucosal healing, but also optimization of systemic perfusion and underlying medical conditions. Our patient’s successful recovery without surgical intervention illustrates the value of prompt recognition, diligent supportive care, and multidisciplinary in achieving favorable outcomes.
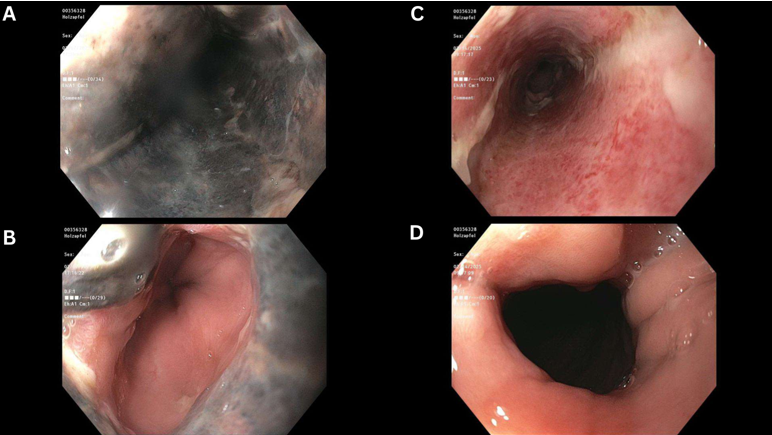
Figure: Figure 1: Serial endoscopic images of the distal esophagus in a 93-year-old male presenting with hematemesis and melena. (A–B) Initial EGD on hospital day 1 showing diffuse black discoloration and friable necrotic mucosa in the distal esophagus consistent with acute esophageal necrosis (black esophagus). (C–D) Follow-up EGD on hospital day 7 demonstrating significant mucosal healing with resolution of necrosis and persistent but improving esophagitis.

Figure: Figure 2: Histopathologic evaluation of esophageal biopsies: (A) Low-power view showing no residual normal esophageal squamous epithelium with extensive mucosal necrosis and tissue fragmentation. (B) High-power view demonstrating acute inflammation with micro-abscess formation and necrotic debris. (C) High-power image highlighting severe acute inflammation with prominent brown-black pigment deposition, consistent with necrotic tissue.
Disclosures:
Mohammed Ayyad indicated no relevant financial relationships.
Lan Nguyen indicated no relevant financial relationships.
Maram Albandak indicated no relevant financial relationships.
Joshua Pagán-Busigó indicated no relevant financial relationships.
Rajiv Pulinthanathu indicated no relevant financial relationships.
Dhanasekaran Ramasamy indicated no relevant financial relationships.
Shiva Kumar indicated no relevant financial relationships.
Mohammed Ayyad, MD1, Lan Nguyen, DO2, Maram Albandak, MD, MPH3, Joshua E. Pagán-Busigó, MD4, Rajiv Pulinthanathu, MD5, Dhanasekaran Ramasamy, MD1, Shiva Kumar, MD6. P0697 - Black Esophagus in a Nonagenarian With Hematemesis: A Case of Acute Esophageal Necrosis With Mucosal Recovery, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Rutgers New Jersey Medical School, Newark, NJ; 2University at Buffalo, Buffalo, NY; 3Department of Internal Medicine, The University of Toledo, Toledo, OH, USA, Toledo, OH; 4Rutgers New Jersey Medical School, Kearny, NJ; 5Rutgers Robert Wood Johnson University Hospital, Newark, NJ; 6Cleveland Clinic Abu Dhabi, Cleveland, OH
Introduction: Acute esophageal necrosis (AEN), also known as "black esophagus," is a rare but serious manifestation of ischemic injury to the esophagus. It is characterized by diffuse circumferential black discoloration of the esophageal mucosa, most commonly affecting the distal esophagus with varying degrees of proximal extension. AEN is often multifactorial in origin, resulting from systemic hypoperfusion and critical illness that compromise mucosal integrity. Early recognition and timely supportive management are essential, particularly in patients with complex comorbidities that impair tissue perfusion.
Case Description/
Methods: A 93-year-old male with multiple co-morbid conditions of atrial fibrillation on anticoagulation, congestive heart failure, pulmonary hypertension, diabetes mellitus, and severe aortic stenosis presented with coffee-ground emesis and melena. Emergent esophagogastroduodenoscopy (EGD) revealed a confluence of necrotic-appearing mucosa in the mid-to-distal esophagus suggestive of AEN. Biopsies were obtained, which confirmed severe acute inflammation with prominent brown-black pigment deposition, consistent with necrotic tissue. The patient was managed conservatively with intravenous pantoprazole, total parenteral nutrition, hydration, and optimization of his underlying comorbidities. Given his advanced age and medical complexity, surgical intervention was deferred. Close hemodynamic monitoring and supportive management resulted in clinical stabilization and gradual recovery. A repeat EGD on day 7 demonstrated substantial mucosal healing. The patient was discharged on oral proton pump inhibitor therapy and has remained clinically stable without readmission.
Discussion: This case highlights the importance of recognizing AEN in the appropriate clinical context and compatible endoscopic findings. Co-morbid conditions such as heart failure, aortic stenosis, and atrial fibrillation can compromise esophageal perfusion and impair mucosal defenses, increasing susceptibility to ischemic injury. Management of AEN involves not only measures to hasten mucosal healing, but also optimization of systemic perfusion and underlying medical conditions. Our patient’s successful recovery without surgical intervention illustrates the value of prompt recognition, diligent supportive care, and multidisciplinary in achieving favorable outcomes.
Figure: Figure 1: Serial endoscopic images of the distal esophagus in a 93-year-old male presenting with hematemesis and melena. (A–B) Initial EGD on hospital day 1 showing diffuse black discoloration and friable necrotic mucosa in the distal esophagus consistent with acute esophageal necrosis (black esophagus). (C–D) Follow-up EGD on hospital day 7 demonstrating significant mucosal healing with resolution of necrosis and persistent but improving esophagitis.

Figure: Figure 2: Histopathologic evaluation of esophageal biopsies: (A) Low-power view showing no residual normal esophageal squamous epithelium with extensive mucosal necrosis and tissue fragmentation. (B) High-power view demonstrating acute inflammation with micro-abscess formation and necrotic debris. (C) High-power image highlighting severe acute inflammation with prominent brown-black pigment deposition, consistent with necrotic tissue.
Disclosures:
Mohammed Ayyad indicated no relevant financial relationships.
Lan Nguyen indicated no relevant financial relationships.
Maram Albandak indicated no relevant financial relationships.
Joshua Pagán-Busigó indicated no relevant financial relationships.
Rajiv Pulinthanathu indicated no relevant financial relationships.
Dhanasekaran Ramasamy indicated no relevant financial relationships.
Shiva Kumar indicated no relevant financial relationships.
Mohammed Ayyad, MD1, Lan Nguyen, DO2, Maram Albandak, MD, MPH3, Joshua E. Pagán-Busigó, MD4, Rajiv Pulinthanathu, MD5, Dhanasekaran Ramasamy, MD1, Shiva Kumar, MD6. P0697 - Black Esophagus in a Nonagenarian With Hematemesis: A Case of Acute Esophageal Necrosis With Mucosal Recovery, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
