Sunday Poster Session
Category: Esophagus
P0693 - From Gastric Relief (Prolonged PPI Use) to Mineral Grief (Euvolemic Hyponatremia): A Case Study of PPI-Induced Symptomatic Hyponatremia
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall
- MH
Muhammad Hammad ul HU Hassan, MD (he/him/his)
South Brooklyn Health
Brooklyn, NY
Presenting Author(s)
Muhammad Sheraz Hameed, MBBS1, Ali iqbal, MD2, Muhammad Hammad ul HU. Hassan, MD3, Syed Rafay H zaidi, MBBS4, Azeen Razzaq, MBBS1, Muhammad Usama Naveed, MBBS1, Farhan Ali, MD5
1Rawalpindi Medical University, Rawalpindi, Punjab, Pakistan; 2Thomas Jefferson University Hospital, Bensalem, PA; 3South Brooklyn Health, Brooklyn, NY; 4Parkview Medical Center, Pueblo, CO; 5Sinai Hospital, Baltimore, MD
Introduction: Proton pump inhibitors (PPIs) are commonly used for acid reflux-related conditions like GERD. Chronic use can lead to adverse effects, including hypomagnesemia and hypokalemia. Hyponatremia with euvolemia due to PPI use is rare and usually associated with omeprazole or pantoprazole. This case highlights the importance of electrolyte monitoring during prolonged PPI therapy.
Case Description/
Methods: A 54-year-old male with GERD, hypertension, and hyperlipidemia presented in April 2025 with worsening muscle cramps, confusion, and dizziness. He had been on pantoprazole 40 mg daily for over four years. On exam, he was disoriented but hemodynamically stable (BP: 126/88 mmHg, HR: 82 bpm), with no fluid overload or dehydration. Neuro exam revealed mild disorientation. He denied recent medication changes, GI loss, or excessive fluid intake.
Labs showed severe hyponatremia (Na⁺ 90 mmol/L), hypomagnesemia (Mg²⁺ 1.1 mg/dL), and hypokalemia (K⁺ 2.4 mEq/L), with serum osmolality of 243 mOsm/kg and urine sodium of 60 mmol/L, consistent with euvolemic hyponatremia. Thyroid and adrenal functions were normal. Treatment included 3% saline, fluid restriction (800 mL/day), and IV saline. Sodium normalized to 141 mmol/L within 48 hours. He was discharged on famotidine (20 mg BID), discontinuing pantoprazole.
One week later, sodium was stable (137 mmol/L), but GERD symptoms returned. Esomeprazole (40 mg daily) was started. Three weeks later, he was readmitted with hyponatremia (Na⁺ 113 mmol/L, osmolality 251 mOsm/kg). Reverting to famotidine normalized sodium at 4, 8, and 12-week follow-ups, indicating a class effect.
Discussion: PPIs commonly cause hypomagnesemia and hypokalemia. Symptomatic euvolemic hyponatremia is a rare but potentially life-threatening condition requiring prompt diagnosis and intervention. Sequential hyponatremia with two different PPIs suggests a class effect. Clinicians must monitor electrolytes in long-term PPI users, especially those presenting with neurological symptoms. Prompt management and consideration of alternatives, such as famotidine, are recommended. Further research is needed to better understand the mechanisms, such as ADH-like effects leading to impaired water excretion and dilutional hyponatremia, and to develop preventive strategies for PPI-induced hyponatremia.
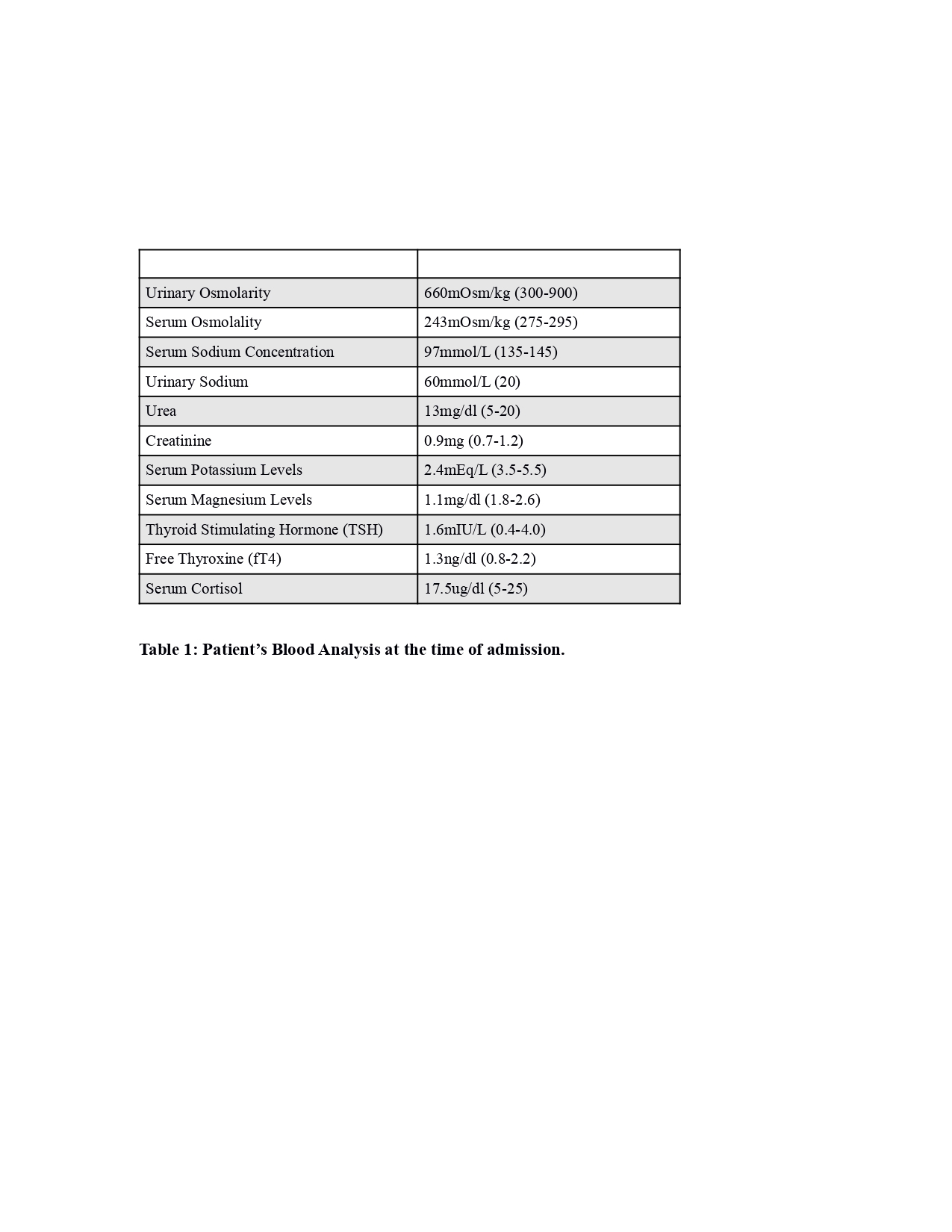
Figure: Patients Blood Analysis at the time of admission
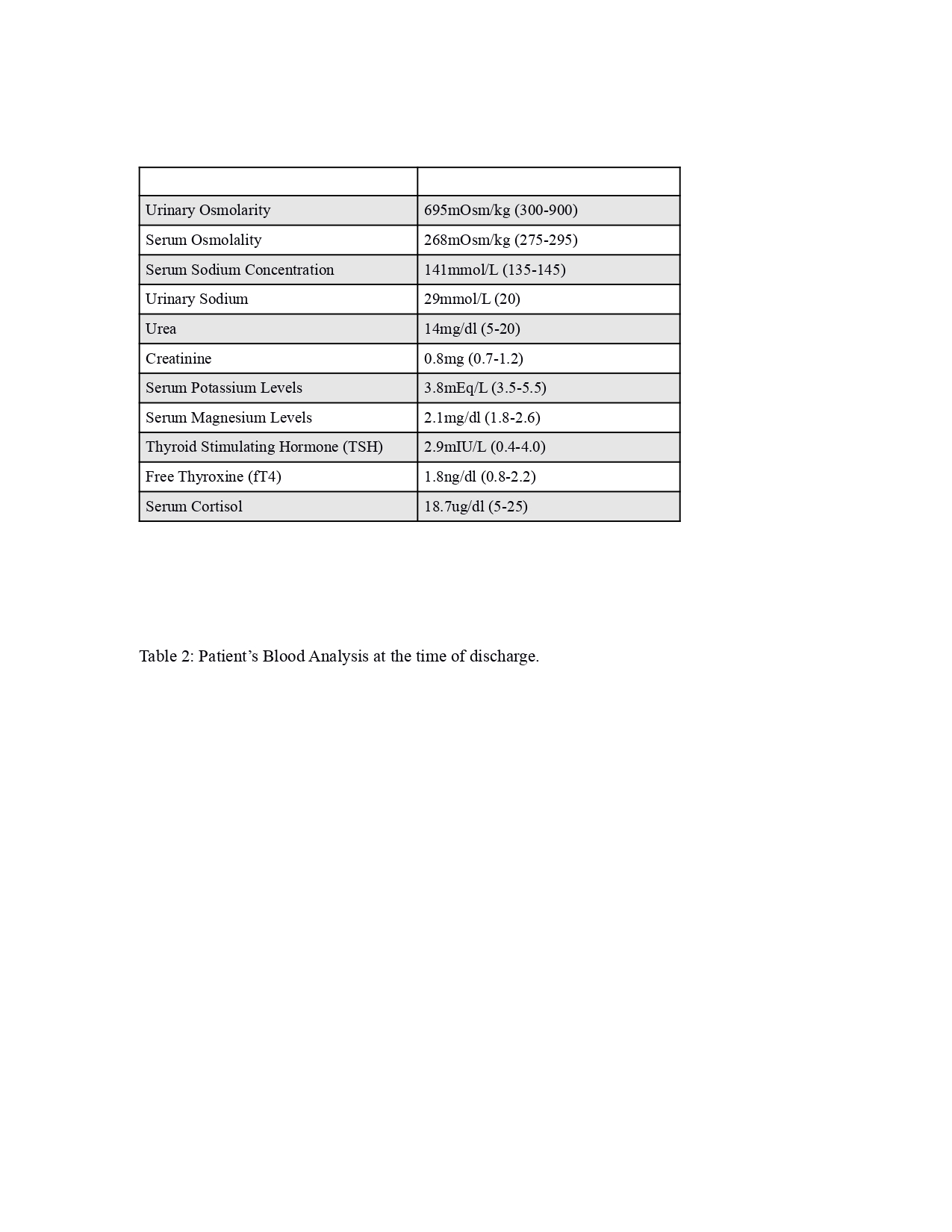
Figure: Patients Blood Analysis at the time of discharge
Disclosures:
Muhammad Sheraz Hameed indicated no relevant financial relationships.
Ali iqbal indicated no relevant financial relationships.
Muhammad Hammad ul Hassan indicated no relevant financial relationships.
Syed Rafay H zaidi indicated no relevant financial relationships.
Azeen Razzaq indicated no relevant financial relationships.
Muhammad Usama Naveed indicated no relevant financial relationships.
Farhan Ali indicated no relevant financial relationships.
Muhammad Sheraz Hameed, MBBS1, Ali iqbal, MD2, Muhammad Hammad ul HU. Hassan, MD3, Syed Rafay H zaidi, MBBS4, Azeen Razzaq, MBBS1, Muhammad Usama Naveed, MBBS1, Farhan Ali, MD5. P0693 - From Gastric Relief (Prolonged PPI Use) to Mineral Grief (Euvolemic Hyponatremia): A Case Study of PPI-Induced Symptomatic Hyponatremia, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Rawalpindi Medical University, Rawalpindi, Punjab, Pakistan; 2Thomas Jefferson University Hospital, Bensalem, PA; 3South Brooklyn Health, Brooklyn, NY; 4Parkview Medical Center, Pueblo, CO; 5Sinai Hospital, Baltimore, MD
Introduction: Proton pump inhibitors (PPIs) are commonly used for acid reflux-related conditions like GERD. Chronic use can lead to adverse effects, including hypomagnesemia and hypokalemia. Hyponatremia with euvolemia due to PPI use is rare and usually associated with omeprazole or pantoprazole. This case highlights the importance of electrolyte monitoring during prolonged PPI therapy.
Case Description/
Methods: A 54-year-old male with GERD, hypertension, and hyperlipidemia presented in April 2025 with worsening muscle cramps, confusion, and dizziness. He had been on pantoprazole 40 mg daily for over four years. On exam, he was disoriented but hemodynamically stable (BP: 126/88 mmHg, HR: 82 bpm), with no fluid overload or dehydration. Neuro exam revealed mild disorientation. He denied recent medication changes, GI loss, or excessive fluid intake.
Labs showed severe hyponatremia (Na⁺ 90 mmol/L), hypomagnesemia (Mg²⁺ 1.1 mg/dL), and hypokalemia (K⁺ 2.4 mEq/L), with serum osmolality of 243 mOsm/kg and urine sodium of 60 mmol/L, consistent with euvolemic hyponatremia. Thyroid and adrenal functions were normal. Treatment included 3% saline, fluid restriction (800 mL/day), and IV saline. Sodium normalized to 141 mmol/L within 48 hours. He was discharged on famotidine (20 mg BID), discontinuing pantoprazole.
One week later, sodium was stable (137 mmol/L), but GERD symptoms returned. Esomeprazole (40 mg daily) was started. Three weeks later, he was readmitted with hyponatremia (Na⁺ 113 mmol/L, osmolality 251 mOsm/kg). Reverting to famotidine normalized sodium at 4, 8, and 12-week follow-ups, indicating a class effect.
Discussion: PPIs commonly cause hypomagnesemia and hypokalemia. Symptomatic euvolemic hyponatremia is a rare but potentially life-threatening condition requiring prompt diagnosis and intervention. Sequential hyponatremia with two different PPIs suggests a class effect. Clinicians must monitor electrolytes in long-term PPI users, especially those presenting with neurological symptoms. Prompt management and consideration of alternatives, such as famotidine, are recommended. Further research is needed to better understand the mechanisms, such as ADH-like effects leading to impaired water excretion and dilutional hyponatremia, and to develop preventive strategies for PPI-induced hyponatremia.
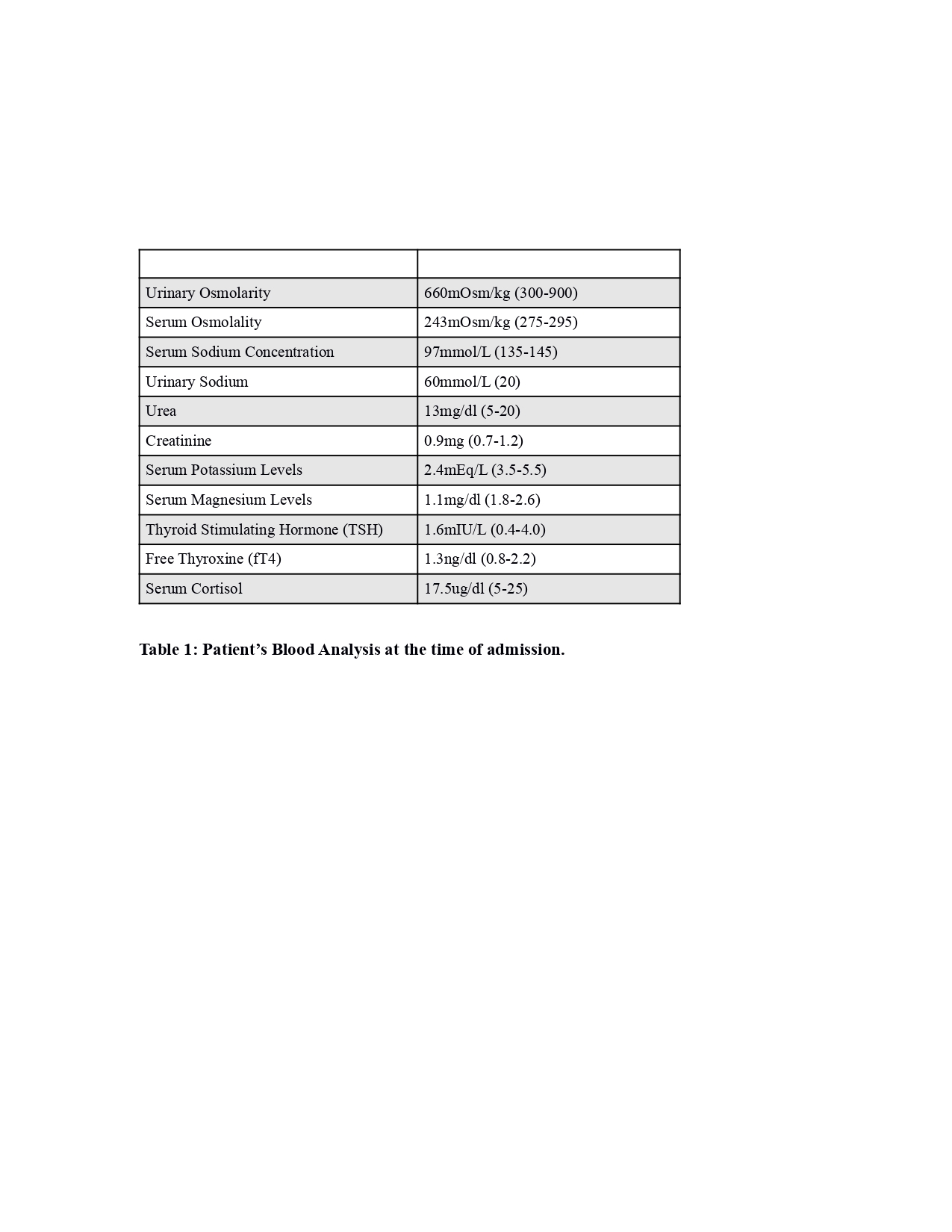
Figure: Patients Blood Analysis at the time of admission
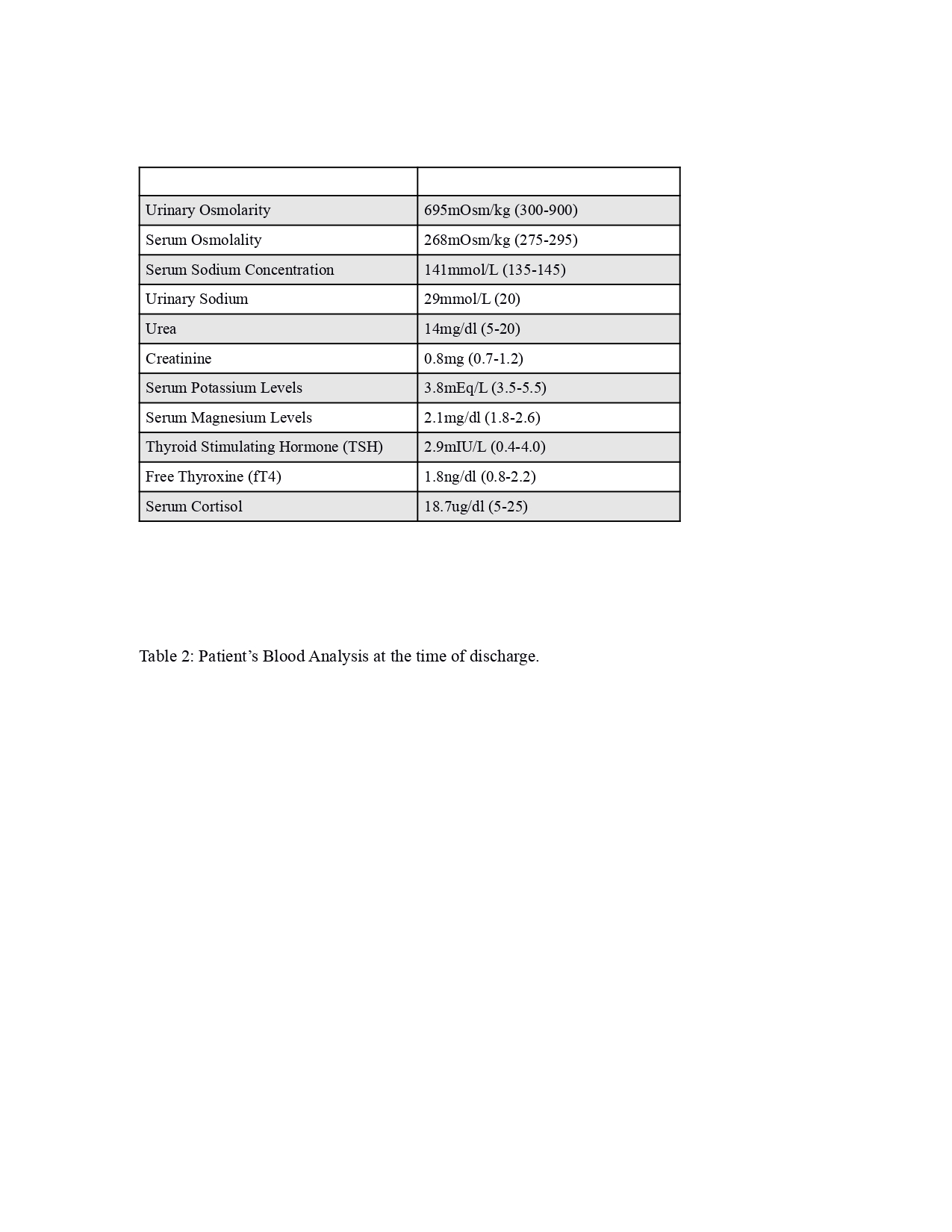
Figure: Patients Blood Analysis at the time of discharge
Disclosures:
Muhammad Sheraz Hameed indicated no relevant financial relationships.
Ali iqbal indicated no relevant financial relationships.
Muhammad Hammad ul Hassan indicated no relevant financial relationships.
Syed Rafay H zaidi indicated no relevant financial relationships.
Azeen Razzaq indicated no relevant financial relationships.
Muhammad Usama Naveed indicated no relevant financial relationships.
Farhan Ali indicated no relevant financial relationships.
Muhammad Sheraz Hameed, MBBS1, Ali iqbal, MD2, Muhammad Hammad ul HU. Hassan, MD3, Syed Rafay H zaidi, MBBS4, Azeen Razzaq, MBBS1, Muhammad Usama Naveed, MBBS1, Farhan Ali, MD5. P0693 - From Gastric Relief (Prolonged PPI Use) to Mineral Grief (Euvolemic Hyponatremia): A Case Study of PPI-Induced Symptomatic Hyponatremia, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
