Sunday Poster Session
Category: Esophagus
P0688 - Dysphagia Aortica-Induced Deglutition Syncope: A Fluoroscopic Diagnosis
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall

Brenton Davis, MD (he/him/his)
Kaiser Permanente
San Francisco, CA
Presenting Author(s)
Brenton Davis, MD1, Mitchell Liverant, MD2
1Kaiser Permanente, San Francisco, CA; 2Kaiser Permanente, Oakland, CA
Introduction: Dysphagia aortica (DA) is characterized by esophageal dysphagia due to extrinsic compression of the esophagus by the thoracic aorta. Common causes include aneurysmal dilation, tortuosity or congenital vascular anomalies. A multitude of pathologic conditions like aortic dissection, aortoesophageal fistula, and thoracic aneurysm can cause this phenomenon. Deglutition syncope (DS) is a rare neurally mediated form of syncope due to swallowing induced vasovagal response leading to bradycardia, hypotension, and loss of consciousness (LOC). We describe a rare case of dysphagia aortica presenting as an uncommonly encountered syndrome associated solely with eating out at restaurants.
Case Description/
Methods: An 83-year-old woman presented to the ED from a senior living facility after having a syncopal episode with nausea and vomiting while eating at a restaurant. Witnesses confirmed no seizure activity, focal deficits, or post-ictal state. Evaluation including CBC, BMP, EKG, and CXR were normal and she was discharged. One month later while eating at a church dinner she had another witnessed episode of nausea, emesis and LOC associated with eating. After a few minutes, she awoke without focal deficits. A 30-day heart monitor was normal. The patient was referred to GI after history revealed four episodes over the past year, all while dining at restaurants. Episodes occur after 1-2 food bites, followed by nausea, vomiting, and syncope without cardiac symptoms. No episodes occurred at her living facility. Barium esophagram with tablet showed prominent aortic knob with retention of the tablet requiring additional water to clear (Figure 1). CT Chest confirmed esophageal compression from thoracic aorta (Figure 2). Per patient preference, given her comorbidities and likely low diagnostic yield, endoscopy was deferred. For treatment the patient was instructed to take smaller bites and avoid large food boluses. Since initiating behavioral changes there has been no recurrence of DS.
Discussion: Elderly patients with meal-associated syncope warrant DA suspicion. Large food boluses compress aortic-esophageal structures pressuring vagal-aortic plexus causing vasovagal response. Barium swallow with tablet is crucial for diagnosis. Risk factors include elderly females with kyphosis and short stature. Management can range from behavioral interventions to surgery and
a detailed eating history is paramount to diagnosis. Behavioral interventions can provide significant benefit with minimal risk in the correct patient.
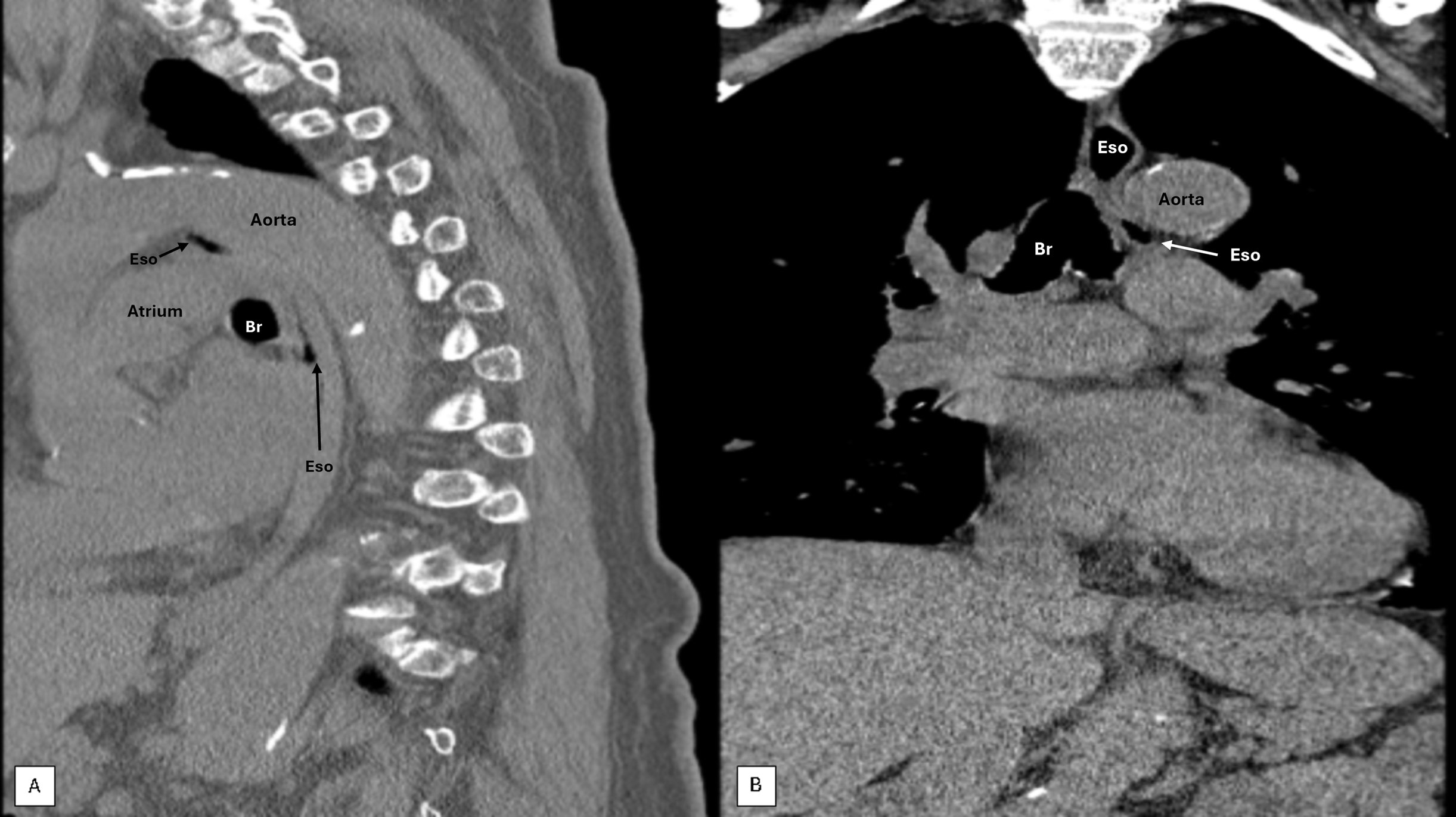
Figure: Figure 1. A) Barium esophagram showing prominent aortic knob with noted extrinsic compression. B) Barium tablet stuck on Aortic knob which required additional water to swallow.
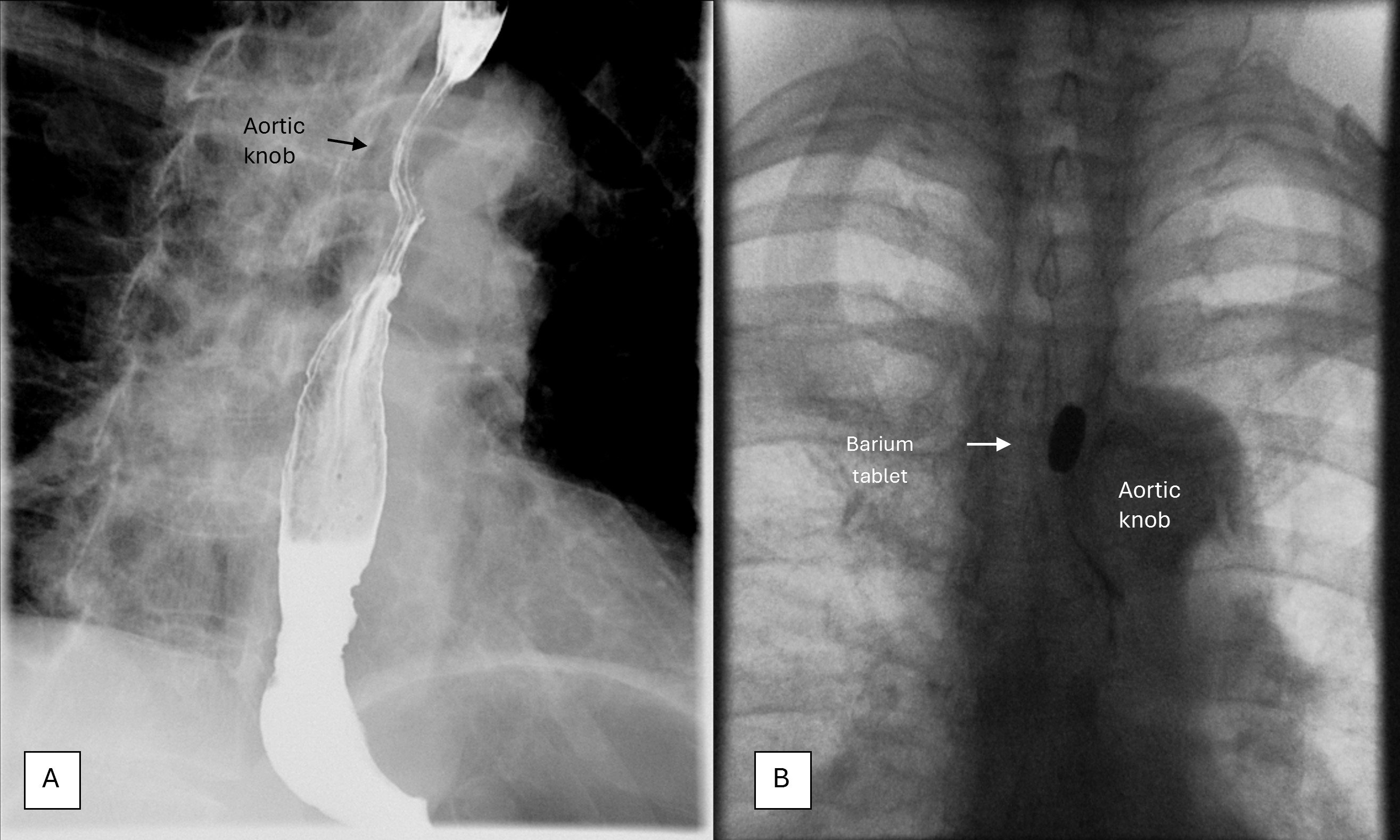
Figure: Figure 2. A) Sagittal CTAP showing esophagus (Eso) compressed by aorta along with atherosclerosis and thoracic kyphosis. B) Coronal CTAP showing focal luminal narrowing of esophagus from extrinsic compression.
Br – bronchus, Eso - esophagus
Disclosures:
Brenton Davis indicated no relevant financial relationships.
Mitchell Liverant indicated no relevant financial relationships.
Brenton Davis, MD1, Mitchell Liverant, MD2. P0688 - Dysphagia Aortica-Induced Deglutition Syncope: A Fluoroscopic Diagnosis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Kaiser Permanente, San Francisco, CA; 2Kaiser Permanente, Oakland, CA
Introduction: Dysphagia aortica (DA) is characterized by esophageal dysphagia due to extrinsic compression of the esophagus by the thoracic aorta. Common causes include aneurysmal dilation, tortuosity or congenital vascular anomalies. A multitude of pathologic conditions like aortic dissection, aortoesophageal fistula, and thoracic aneurysm can cause this phenomenon. Deglutition syncope (DS) is a rare neurally mediated form of syncope due to swallowing induced vasovagal response leading to bradycardia, hypotension, and loss of consciousness (LOC). We describe a rare case of dysphagia aortica presenting as an uncommonly encountered syndrome associated solely with eating out at restaurants.
Case Description/
Methods: An 83-year-old woman presented to the ED from a senior living facility after having a syncopal episode with nausea and vomiting while eating at a restaurant. Witnesses confirmed no seizure activity, focal deficits, or post-ictal state. Evaluation including CBC, BMP, EKG, and CXR were normal and she was discharged. One month later while eating at a church dinner she had another witnessed episode of nausea, emesis and LOC associated with eating. After a few minutes, she awoke without focal deficits. A 30-day heart monitor was normal. The patient was referred to GI after history revealed four episodes over the past year, all while dining at restaurants. Episodes occur after 1-2 food bites, followed by nausea, vomiting, and syncope without cardiac symptoms. No episodes occurred at her living facility. Barium esophagram with tablet showed prominent aortic knob with retention of the tablet requiring additional water to clear (Figure 1). CT Chest confirmed esophageal compression from thoracic aorta (Figure 2). Per patient preference, given her comorbidities and likely low diagnostic yield, endoscopy was deferred. For treatment the patient was instructed to take smaller bites and avoid large food boluses. Since initiating behavioral changes there has been no recurrence of DS.
Discussion: Elderly patients with meal-associated syncope warrant DA suspicion. Large food boluses compress aortic-esophageal structures pressuring vagal-aortic plexus causing vasovagal response. Barium swallow with tablet is crucial for diagnosis. Risk factors include elderly females with kyphosis and short stature. Management can range from behavioral interventions to surgery and
a detailed eating history is paramount to diagnosis. Behavioral interventions can provide significant benefit with minimal risk in the correct patient.
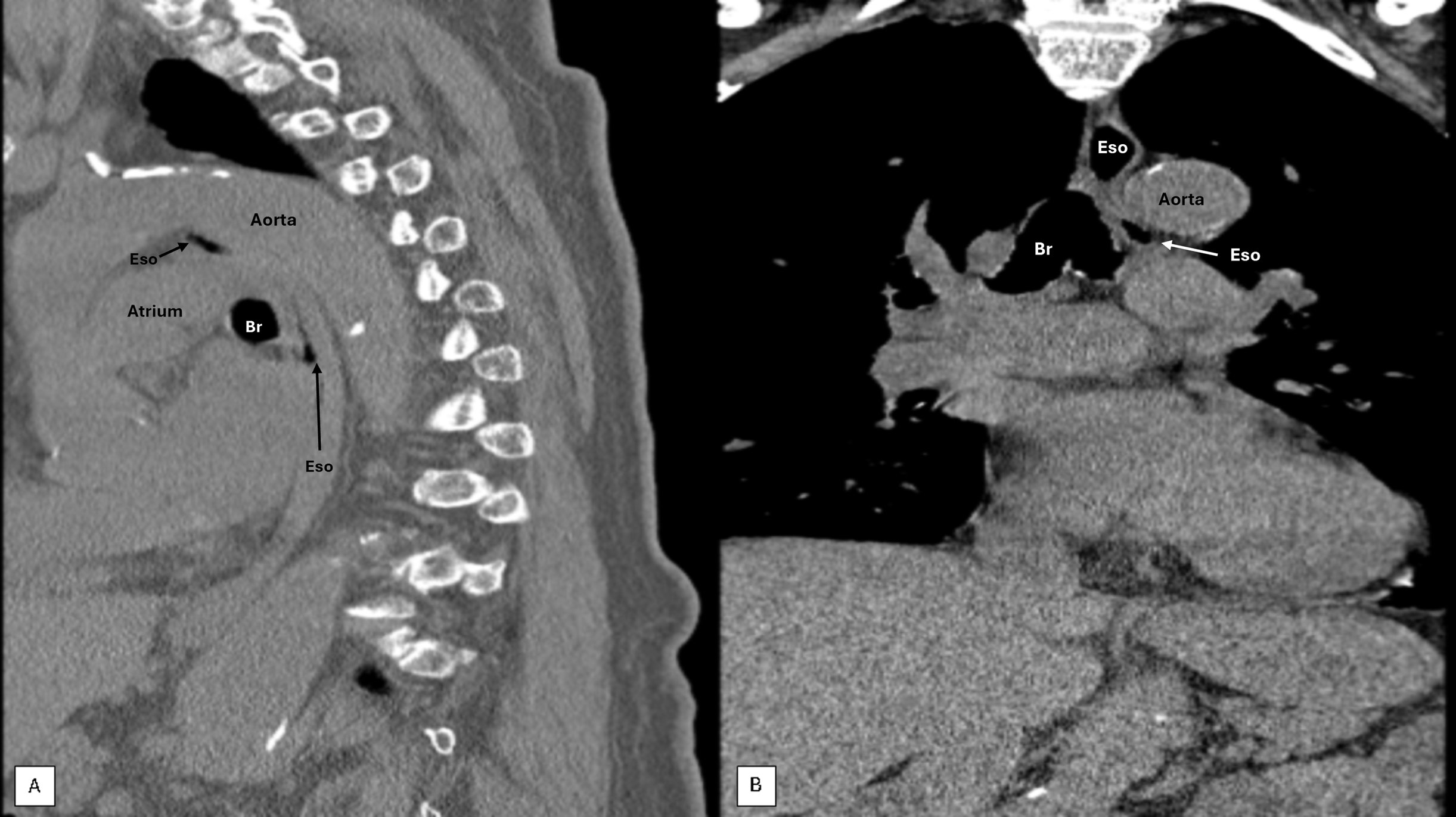
Figure: Figure 1. A) Barium esophagram showing prominent aortic knob with noted extrinsic compression. B) Barium tablet stuck on Aortic knob which required additional water to swallow.
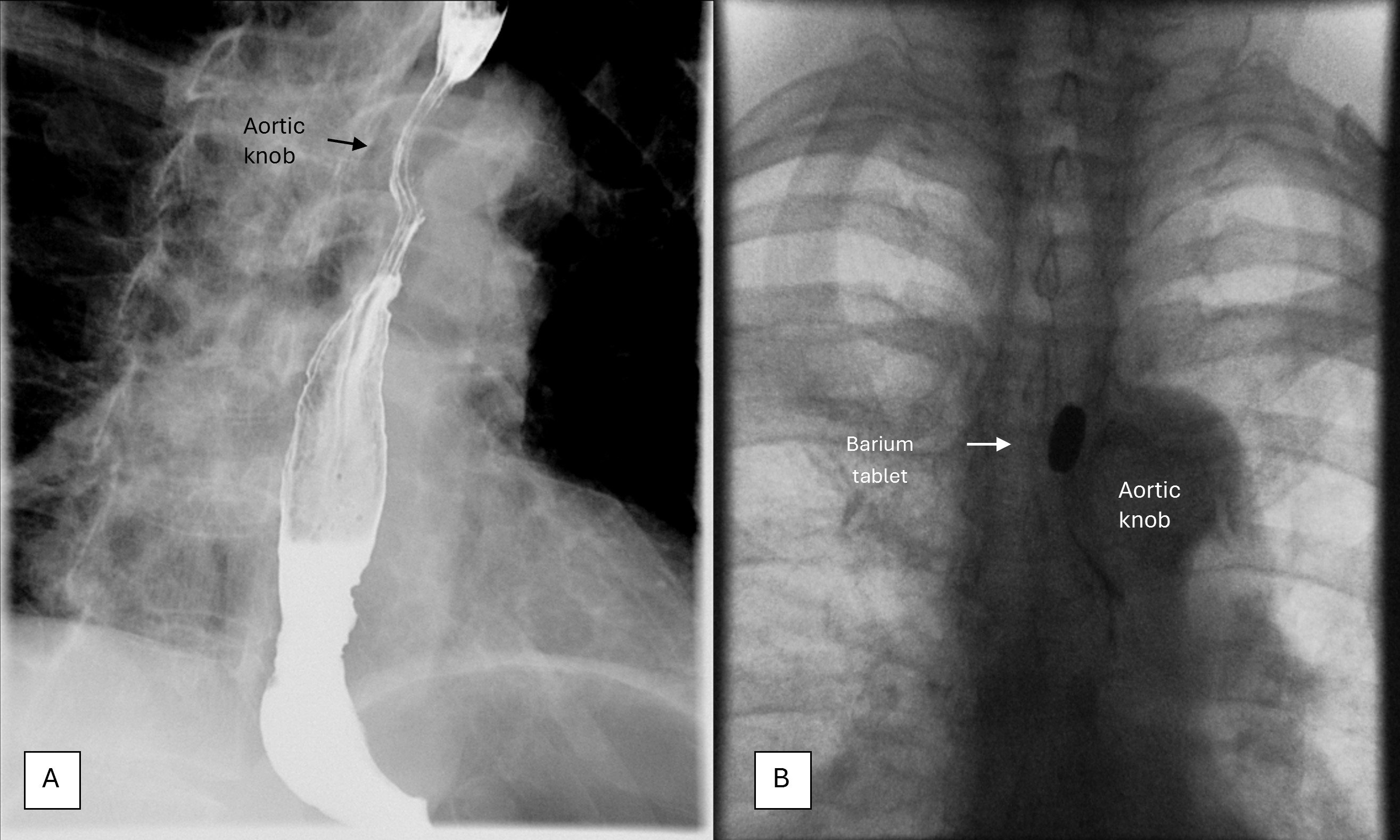
Figure: Figure 2. A) Sagittal CTAP showing esophagus (Eso) compressed by aorta along with atherosclerosis and thoracic kyphosis. B) Coronal CTAP showing focal luminal narrowing of esophagus from extrinsic compression.
Br – bronchus, Eso - esophagus
Disclosures:
Brenton Davis indicated no relevant financial relationships.
Mitchell Liverant indicated no relevant financial relationships.
Brenton Davis, MD1, Mitchell Liverant, MD2. P0688 - Dysphagia Aortica-Induced Deglutition Syncope: A Fluoroscopic Diagnosis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
