Sunday Poster Session
Category: Esophagus
P0771 - Refractory Esophagitis and Stricture Mistreated With Fundoplication: Think About Lichen Planus
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall
- TL
Tian Li, MD, MS (she/her/hers)
Mayo Clinic
Jacksonville, FL
Presenting Author(s)
Tian Li, MD, MS, Andree Koop, MD
Mayo Clinic, Jacksonville, FL
Introduction: Esophageal lichen planus (ELP) is a chronic immune-mediated inflammatory condition which primarily affects middle-aged to older women and often coexists with oral or genital lichen planus. Due to its nonspecific symptoms and overlap with other esophageal disorders, ELP is often under recognized and misdiagnosed. We present two cases initially misdiagnosed and treated with fundoplication.
Case Description/
Methods: Case 1: A 67-year-old female presented with a 2-year history of progressive dysphagia to solids and liquids without heartburn or regurgitation. Prior endoscopy showed diffuse esophageal inflammation and ulcers. She failed high-dose PPI therapy and underwent robotic hiatal hernia with Nissen fundoplication. Postoperative symptoms persisted. Barium esophagram revealed a diffusely narrowed esophagus with a 4cm stricture in the upper thoracic esophagus and a lodged barium tablet (Figure 1A). Repeated endoscopy showed severe mucosal friability, sloughing, and ulceration (Figure 1B). ELP was diagnosed. She started on low dose oral tacrolimus and endoscopic steroid injection.
Case 2: A 66-year-old female was referred for refractory esophageal stricture and dysphagia without reflux symptoms. She had previously undergone Nissen fundoplication for presumed reflux-related stricture. Despite one month budesonide and daily dexlansoprazole, symptoms and inflammation persisted, requiring monthly dilations. Esophagram showed a narrow thoracic esophagus with a barium table lodged above the aortic arch (Figure 2A.). Repeated endoscopy identified a proximal stenosis impassable by the scope, dilated to 12mm using a Savary dilator, diffuse mucosal sloughing, altered texture, decreased vascularity, and narrow caliber (Figure 2B) . Biopsy showed superficial squamous mucosa with lymphocytic inflammation and minimal submucosal tissue. Immunofluorescence was negative for immunoglobulins but positive for strong shaggy fibrinogen deposition along the basement membrane, consistent with a lichenoid tissue reaction. She was diagnosed with esophageal lichen planus. She started treatment with topical steroids.
Discussion: Diagnosing ELP requires clinical, endoscopic, and histologic correlation with high index of suspicion. It is essential to biopsy both affected and adjacent mucosa. ELP should be considered in atypical or refractory esophagitis or stricturing diseases, particularly in middle-aged or older white women. Management involves topical or systemic immunosuppression and serial esophageal dilation.
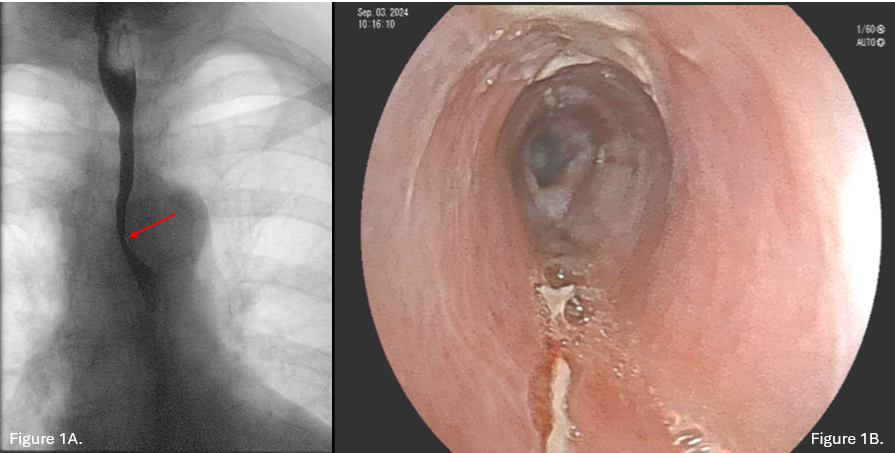
Figure: Figure 1A. Barium esophagram shows 4 cm stricture in the upper thoracic esophagus. Figure 1B. Endoscopy revealing sloughing mucosa and extensive ulceration.
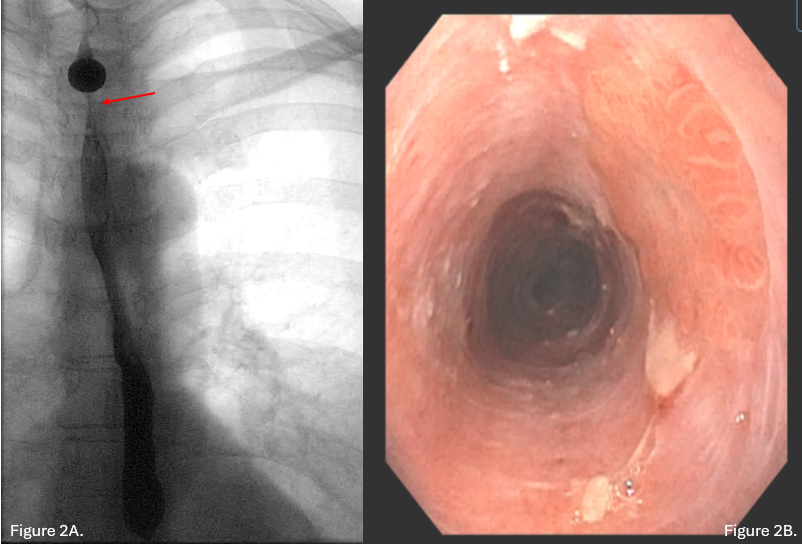
Figure: Figure 2A. Esophagram showed a narrow thoracic esophagus with a barium table lodged above the aortic arch. Figure 2B. Repeat endoscopy revealed diffuse mucosal abnormalities including sloughing, altered texture, decreased vascularity, and a uniformly narrow caliber esophagus.
Disclosures:
Tian Li indicated no relevant financial relationships.
Andree Koop indicated no relevant financial relationships.
Tian Li, MD, MS, Andree Koop, MD. P0771 - Refractory Esophagitis and Stricture Mistreated With Fundoplication: Think About Lichen Planus, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
Mayo Clinic, Jacksonville, FL
Introduction: Esophageal lichen planus (ELP) is a chronic immune-mediated inflammatory condition which primarily affects middle-aged to older women and often coexists with oral or genital lichen planus. Due to its nonspecific symptoms and overlap with other esophageal disorders, ELP is often under recognized and misdiagnosed. We present two cases initially misdiagnosed and treated with fundoplication.
Case Description/
Methods: Case 1: A 67-year-old female presented with a 2-year history of progressive dysphagia to solids and liquids without heartburn or regurgitation. Prior endoscopy showed diffuse esophageal inflammation and ulcers. She failed high-dose PPI therapy and underwent robotic hiatal hernia with Nissen fundoplication. Postoperative symptoms persisted. Barium esophagram revealed a diffusely narrowed esophagus with a 4cm stricture in the upper thoracic esophagus and a lodged barium tablet (Figure 1A). Repeated endoscopy showed severe mucosal friability, sloughing, and ulceration (Figure 1B). ELP was diagnosed. She started on low dose oral tacrolimus and endoscopic steroid injection.
Case 2: A 66-year-old female was referred for refractory esophageal stricture and dysphagia without reflux symptoms. She had previously undergone Nissen fundoplication for presumed reflux-related stricture. Despite one month budesonide and daily dexlansoprazole, symptoms and inflammation persisted, requiring monthly dilations. Esophagram showed a narrow thoracic esophagus with a barium table lodged above the aortic arch (Figure 2A.). Repeated endoscopy identified a proximal stenosis impassable by the scope, dilated to 12mm using a Savary dilator, diffuse mucosal sloughing, altered texture, decreased vascularity, and narrow caliber (Figure 2B) . Biopsy showed superficial squamous mucosa with lymphocytic inflammation and minimal submucosal tissue. Immunofluorescence was negative for immunoglobulins but positive for strong shaggy fibrinogen deposition along the basement membrane, consistent with a lichenoid tissue reaction. She was diagnosed with esophageal lichen planus. She started treatment with topical steroids.
Discussion: Diagnosing ELP requires clinical, endoscopic, and histologic correlation with high index of suspicion. It is essential to biopsy both affected and adjacent mucosa. ELP should be considered in atypical or refractory esophagitis or stricturing diseases, particularly in middle-aged or older white women. Management involves topical or systemic immunosuppression and serial esophageal dilation.
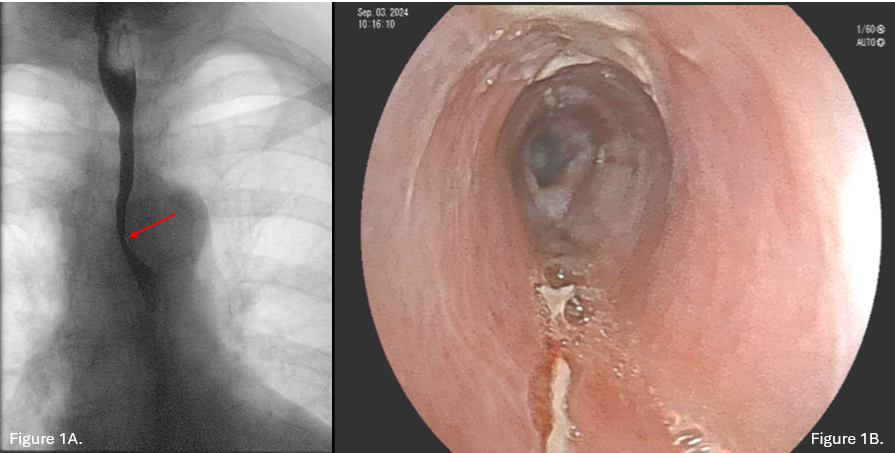
Figure: Figure 1A. Barium esophagram shows 4 cm stricture in the upper thoracic esophagus. Figure 1B. Endoscopy revealing sloughing mucosa and extensive ulceration.
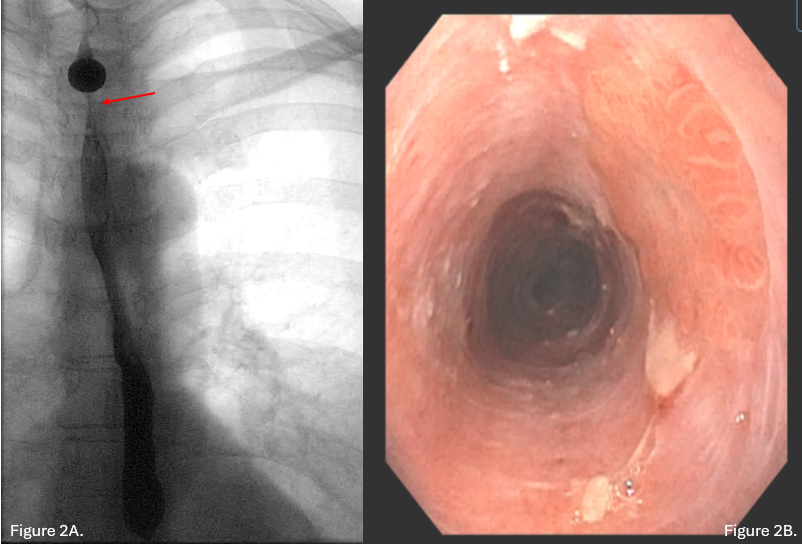
Figure: Figure 2A. Esophagram showed a narrow thoracic esophagus with a barium table lodged above the aortic arch. Figure 2B. Repeat endoscopy revealed diffuse mucosal abnormalities including sloughing, altered texture, decreased vascularity, and a uniformly narrow caliber esophagus.
Disclosures:
Tian Li indicated no relevant financial relationships.
Andree Koop indicated no relevant financial relationships.
Tian Li, MD, MS, Andree Koop, MD. P0771 - Refractory Esophagitis and Stricture Mistreated With Fundoplication: Think About Lichen Planus, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
