Sunday Poster Session
Category: General Endoscopy
P0845 - Proceduralist-Directed Sedation vs Anesthesia Care Team Sedation for Outpatient GI Endoscopy: A Retrospective Comparative Study
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall

Rohit Goyal, MD
Louisiana State University
Shreveport, LA
Presenting Author(s)
Rohit Goyal, MD1, Aditya Vyas, MD2, Shruti Jain, MBBS3, Karan Sachdeva, MD4, Hassaan Zia, MD5, Sudha Pandit, MD1
1Louisiana State University, Shreveport, LA; 2LSUHS, Shreveport, LA; 3Louisiana State University Health, Shreveport, LA; 4LSU Health, Shreveport, LA; 5Medical College of Wisconsin, Milwaukee, WI
Introduction: Proceduralist-directed sedation (PDS) is increasingly utilized to meet the rising demand for gastrointestinal procedures, offering rapid onset and recovery with propofol. Anesthesia care team (ACT) sedation, the traditional alternative, is still used for higher-risk patients. However, comparative data on sedation efficiency, drug wastage, and complication rates remain limited.
Methods: We conducted a retrospective chart review of consecutive outpatient endoscopic procedures at our tertiary care center and classified them into PDS and ACT cohorts. Only procedures using Propofol were included, and procedures with advanced interventions (e.g., POEM, ablations) were excluded. Data on baseline demographic characteristics, type and dosage of sedation used, and any post-procedural complications were collected, and using the Pearson's Chi-Square Test and Kruskal-Wallis Test, on the BlueSky Statistics Version 10.3.4. A significance level of p< 0.05 was applied.
Results: Of a total of 292 outpatient procedures, 240 procedures (PDS=190; ACT=50) were included. Baseline characteristics are summarized in Table 1. PDS patients were younger [52.13 years vs. 58.28 years (p=0.004)] and had significantly lower ASA and Mallampati scores. No significant differences were seen for gender, race, substance use, BMI, or the type of procedure. Table 2 summarizes the sedation usage and complications in the two cohorts. With propofol coming in a 200 mg vial, propofol wastage occurred less frequently in the PDS cohort (59.5% vs. 90%, p< 0.001), although the amount wasted was not statistically significant (95.52 mg vs. 105.11 mg, p=0.11). Other sedatives used along with propofol in the two cohorts were significantly different, with a higher usage of midazolam (p< 0.001) in the PDS cohort, and fentanyl (p< 0.001) and lidocaine (p< 0.001) having a higher usage in the ACT cohort. Sedation-related complications were more commonly seen in the ACT cohort (28% vs. 1.6%, p< 0.001), with hypoxia requiring interventions (22% vs. 0.5%, p< 0.001) being the most common. One patient in the ACT developed aspiration pneumonia and required readmission.
Discussion: PDS is a safe and effective alternative to ACT sedation for outpatient endoscopy, with significantly fewer complications and reduced sedation wastage. These findings support the wider implementation of PDS in appropriately selected patients to improve safety and optimize resource utilization.
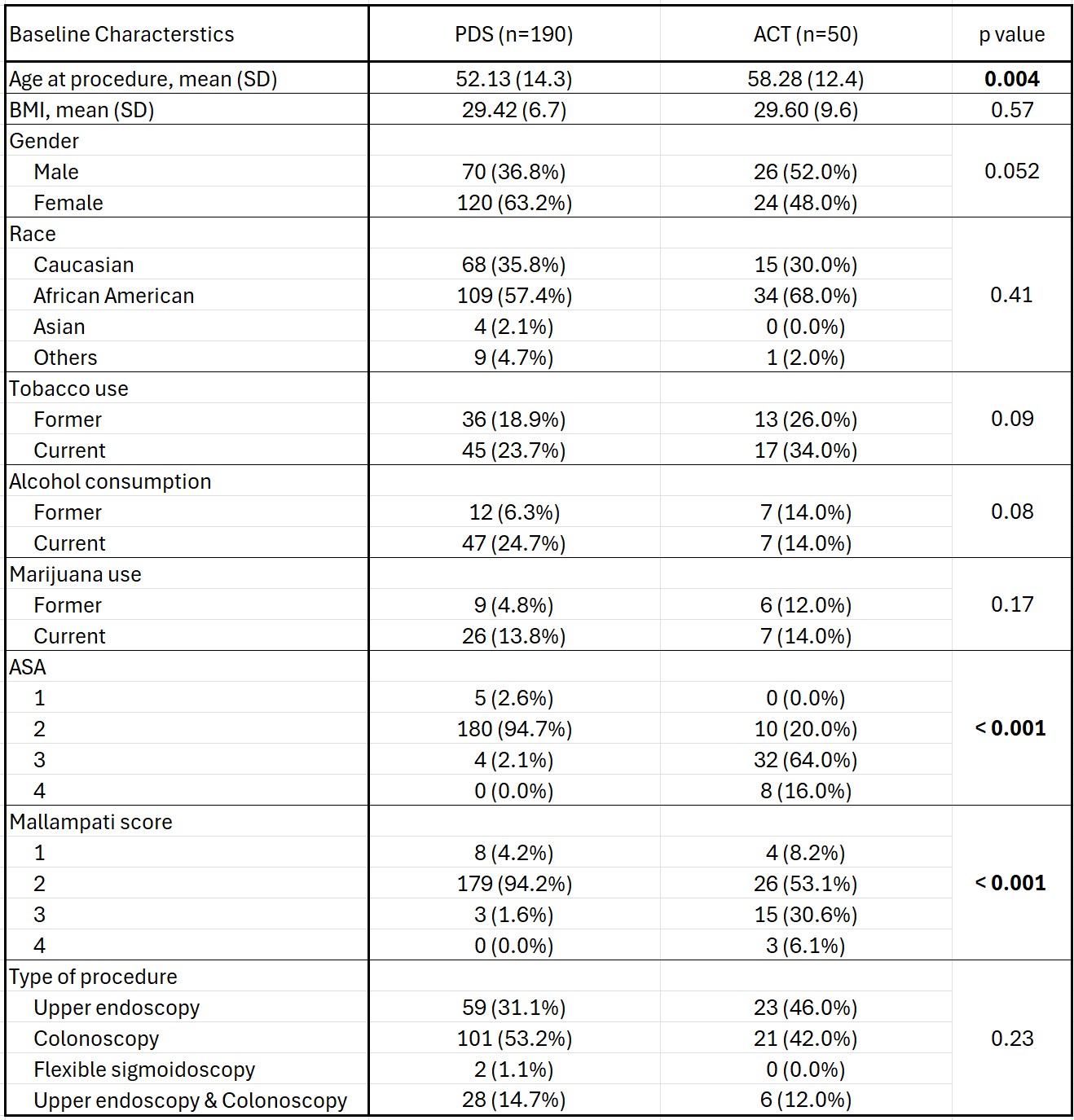
Figure: Figure 1: Baseline characteristics for patients undergoing outpatient endoscopy procedures with proceduralist-directed sedation (PDS) or anesthesia care team (ACT) sedation
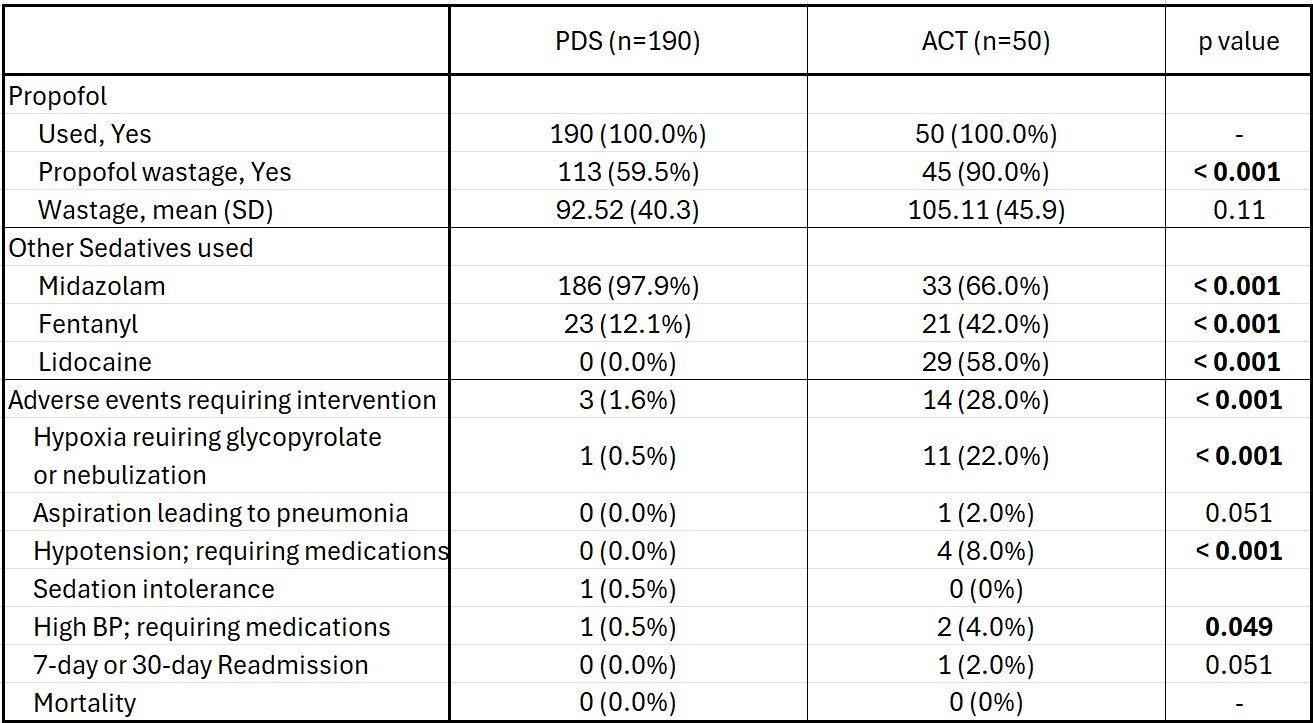
Figure: Table 2: Comparison of sedation usage and complications between proceduralist-directed sedation (PDS) and anesthesia care team (ACT) cohorts
Disclosures:
Rohit Goyal indicated no relevant financial relationships.
Aditya Vyas indicated no relevant financial relationships.
Shruti Jain indicated no relevant financial relationships.
Karan Sachdeva indicated no relevant financial relationships.
Hassaan Zia indicated no relevant financial relationships.
Sudha Pandit: Medtronic – Product feedback.
Rohit Goyal, MD1, Aditya Vyas, MD2, Shruti Jain, MBBS3, Karan Sachdeva, MD4, Hassaan Zia, MD5, Sudha Pandit, MD1. P0845 - Proceduralist-Directed Sedation vs Anesthesia Care Team Sedation for Outpatient GI Endoscopy: A Retrospective Comparative Study, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Louisiana State University, Shreveport, LA; 2LSUHS, Shreveport, LA; 3Louisiana State University Health, Shreveport, LA; 4LSU Health, Shreveport, LA; 5Medical College of Wisconsin, Milwaukee, WI
Introduction: Proceduralist-directed sedation (PDS) is increasingly utilized to meet the rising demand for gastrointestinal procedures, offering rapid onset and recovery with propofol. Anesthesia care team (ACT) sedation, the traditional alternative, is still used for higher-risk patients. However, comparative data on sedation efficiency, drug wastage, and complication rates remain limited.
Methods: We conducted a retrospective chart review of consecutive outpatient endoscopic procedures at our tertiary care center and classified them into PDS and ACT cohorts. Only procedures using Propofol were included, and procedures with advanced interventions (e.g., POEM, ablations) were excluded. Data on baseline demographic characteristics, type and dosage of sedation used, and any post-procedural complications were collected, and using the Pearson's Chi-Square Test and Kruskal-Wallis Test, on the BlueSky Statistics Version 10.3.4. A significance level of p< 0.05 was applied.
Results: Of a total of 292 outpatient procedures, 240 procedures (PDS=190; ACT=50) were included. Baseline characteristics are summarized in Table 1. PDS patients were younger [52.13 years vs. 58.28 years (p=0.004)] and had significantly lower ASA and Mallampati scores. No significant differences were seen for gender, race, substance use, BMI, or the type of procedure. Table 2 summarizes the sedation usage and complications in the two cohorts. With propofol coming in a 200 mg vial, propofol wastage occurred less frequently in the PDS cohort (59.5% vs. 90%, p< 0.001), although the amount wasted was not statistically significant (95.52 mg vs. 105.11 mg, p=0.11). Other sedatives used along with propofol in the two cohorts were significantly different, with a higher usage of midazolam (p< 0.001) in the PDS cohort, and fentanyl (p< 0.001) and lidocaine (p< 0.001) having a higher usage in the ACT cohort. Sedation-related complications were more commonly seen in the ACT cohort (28% vs. 1.6%, p< 0.001), with hypoxia requiring interventions (22% vs. 0.5%, p< 0.001) being the most common. One patient in the ACT developed aspiration pneumonia and required readmission.
Discussion: PDS is a safe and effective alternative to ACT sedation for outpatient endoscopy, with significantly fewer complications and reduced sedation wastage. These findings support the wider implementation of PDS in appropriately selected patients to improve safety and optimize resource utilization.
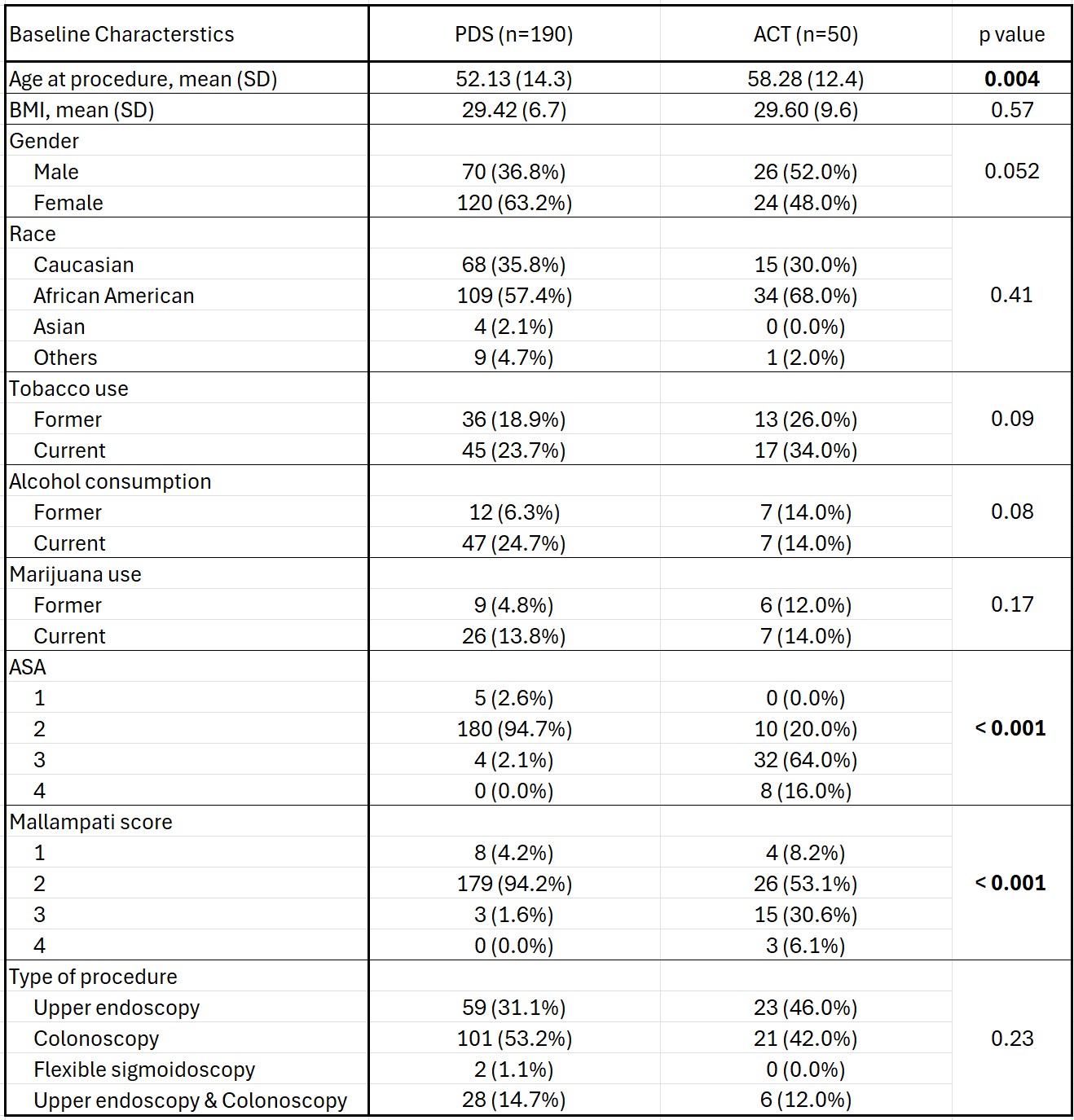
Figure: Figure 1: Baseline characteristics for patients undergoing outpatient endoscopy procedures with proceduralist-directed sedation (PDS) or anesthesia care team (ACT) sedation
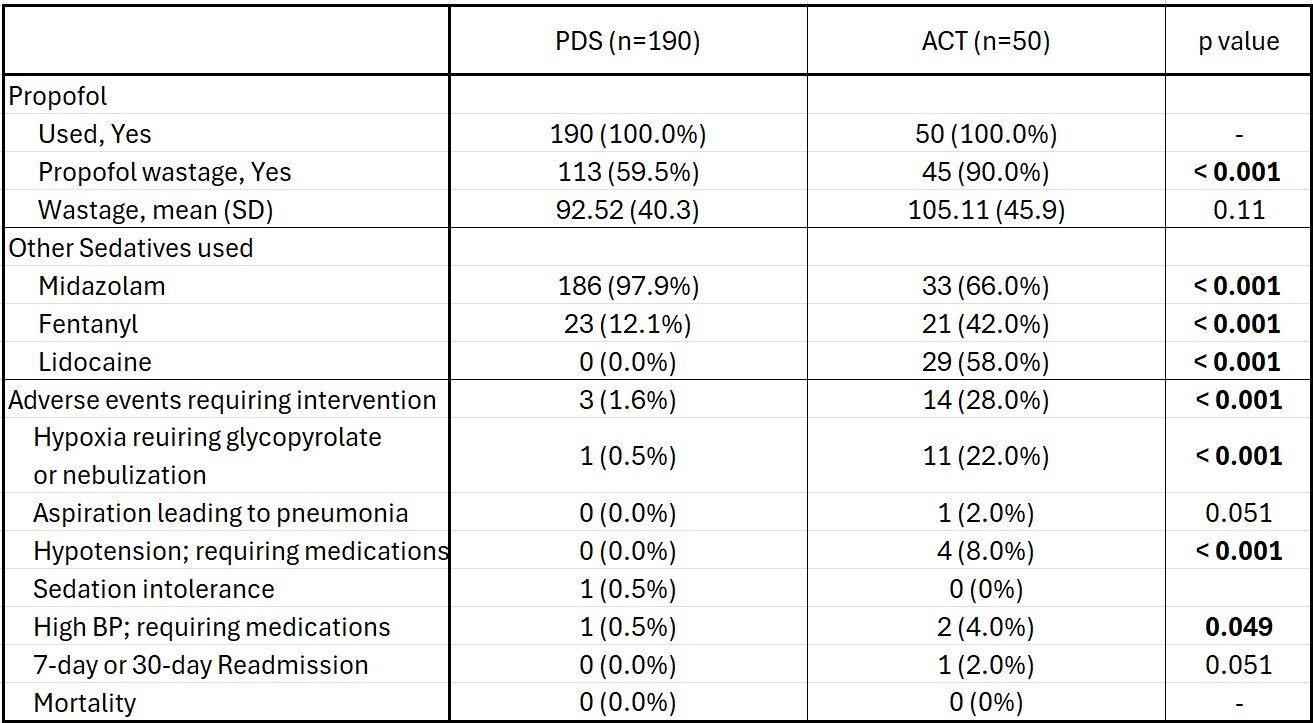
Figure: Table 2: Comparison of sedation usage and complications between proceduralist-directed sedation (PDS) and anesthesia care team (ACT) cohorts
Disclosures:
Rohit Goyal indicated no relevant financial relationships.
Aditya Vyas indicated no relevant financial relationships.
Shruti Jain indicated no relevant financial relationships.
Karan Sachdeva indicated no relevant financial relationships.
Hassaan Zia indicated no relevant financial relationships.
Sudha Pandit: Medtronic – Product feedback.
Rohit Goyal, MD1, Aditya Vyas, MD2, Shruti Jain, MBBS3, Karan Sachdeva, MD4, Hassaan Zia, MD5, Sudha Pandit, MD1. P0845 - Proceduralist-Directed Sedation vs Anesthesia Care Team Sedation for Outpatient GI Endoscopy: A Retrospective Comparative Study, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
