Sunday Poster Session
Category: GI Bleeding
P0911 - The Conundrum of Managing Forrest Class IIb Ulcers: Real-World Findings From 2 Large Urban Medical Centers
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall

Sonia Mehra, MD
Mount Sinai West & Morningside, NY
Presenting Author(s)
Sonia Mehra, MD1, Soha Noorani, DO2, Bharati Dev, DO3, Michael S.. Smith, MD, MBA4
1Mount Sinai West & Morningside, New York, NY; 2Mount Sinai Morningside, Icahn School of Medicine at Mount Sinai, New York, NY; 3Mount Sinai West, Icahn School of Medicine at Mount Sinai, New York, NY; 4Icahn School of Medicine at Mount Sinai, New York, NY
Introduction: Management of Forrest II ulcers varies based on endoscopic appearance. Although IIa (non-bleeding visible vessel) and IIc (flat pigmented spot) ulcers have clear guidance on endoscopic hemostatic intervention, recommendations for IIb ulcers (adherent clot) are not well defined. Our aim is to evaluate real-world adherence to guidelines for Forrest II ulcers and to assess rebleeding risk based on guideline-appropriate intervention, including IIb ulcers where intervention is indeterminate.
Methods: A retrospective chart analysis was conducted on patients with Forrest II ulcers from 2019-2024 at two urban academic centers. Patient demographic characteristics and history of prior proton pump inhibitor (PPI) use were collected from electronic records. Ulcer class, site, and endoscopic intervention were obtained from procedure reports. The primary outcome was to assess 30-day rebleeding rate based on hemostatic intervention. Chi-square analysis was conducted to evaluate variables of interest.
Results: Of 172 patients with fully available data (65.7% male, mean age 67.6 years), the majority of patients had Forrest IIc ulcers (55.8%), with most located in the stomach (51.2%) or duodenum (46.5%) (Table 1). As per guidelines, endoscopic intervention was performed in 96.6% of Forrest IIa ulcers, while 80.2% of Forrest IIc ulcers had no intervention. Although most (61.1%) IIb ulcers were managed endoscopically, there was a higher relative overall 30-day post-endoscopy rebleeding risk (27.8%) in this group than observed in Forrest IIa (12.1%) or IIc (13.5%) ulcers. There was a lower 30-day rate of rebleeding in patients with Forrest IIb ulcers receiving intervention (18.2%) compared to IIb patients without intervention (42.9%) (Table 2). Of note, 30-day rebleeding rates for Forrest IIc ulcers were similar to those of IIa ulcers, regardless of intervention.
Discussion: Treatment of Forrest IIa and IIc ulcers generally followed current guidelines. Forrest IIb ulcers were much less commonly identified and provided a management dilemma, as there are no strict guidelines on the use of hemostatic therapy. These results suggest that intervention may decrease 30-day Class IIb rebleeding rates to around those seen with other Forrest II lesions. When feasible, unroofing adherent clot to expose the ulcer bed and any visible vessel may permit reclassification to IIa or IIc, and therefore provide better guidance on appropriate management with an increased risk of rebleeding.
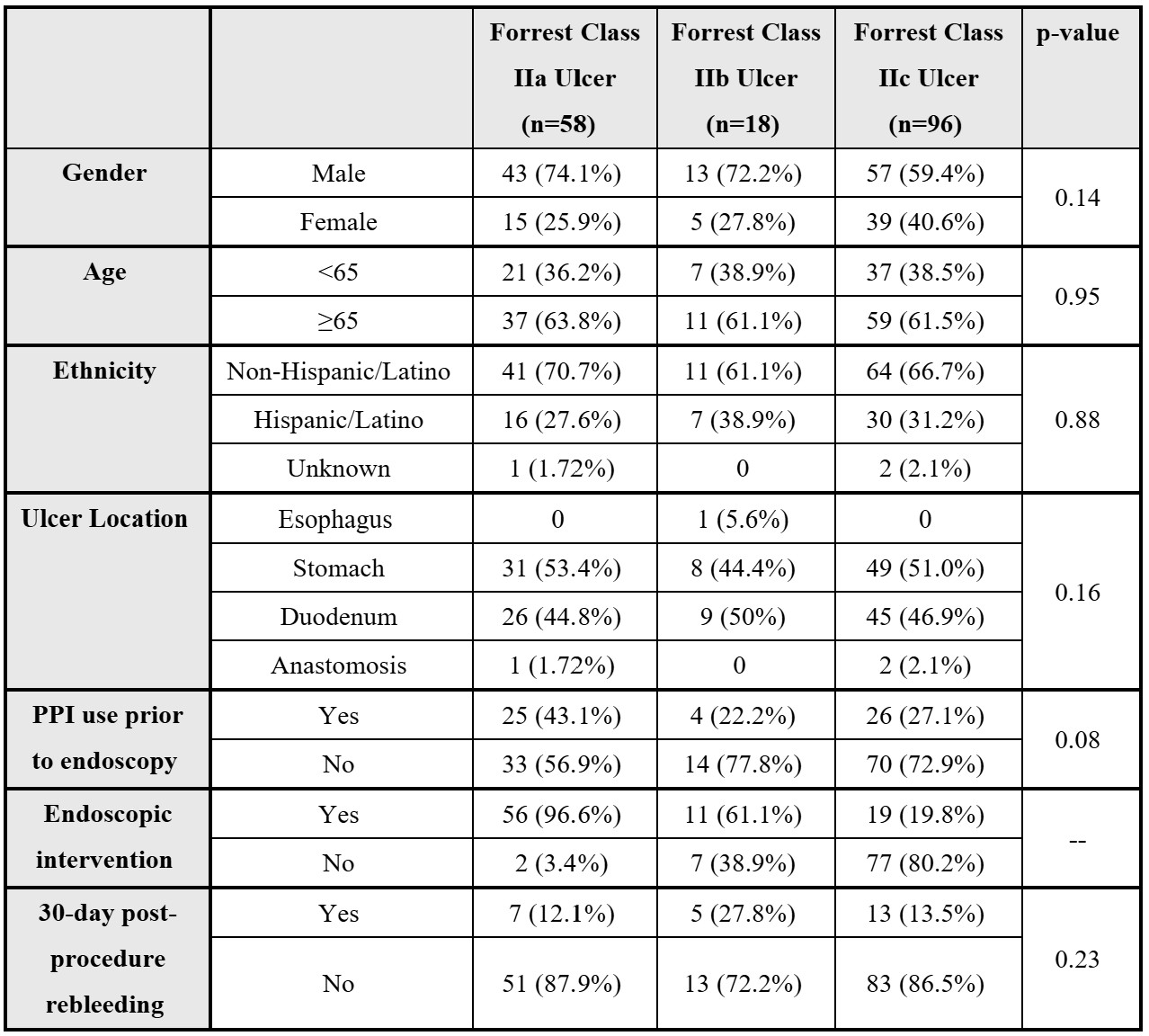
Figure: Table 1: Patient Characteristics Based On Forrest Classification
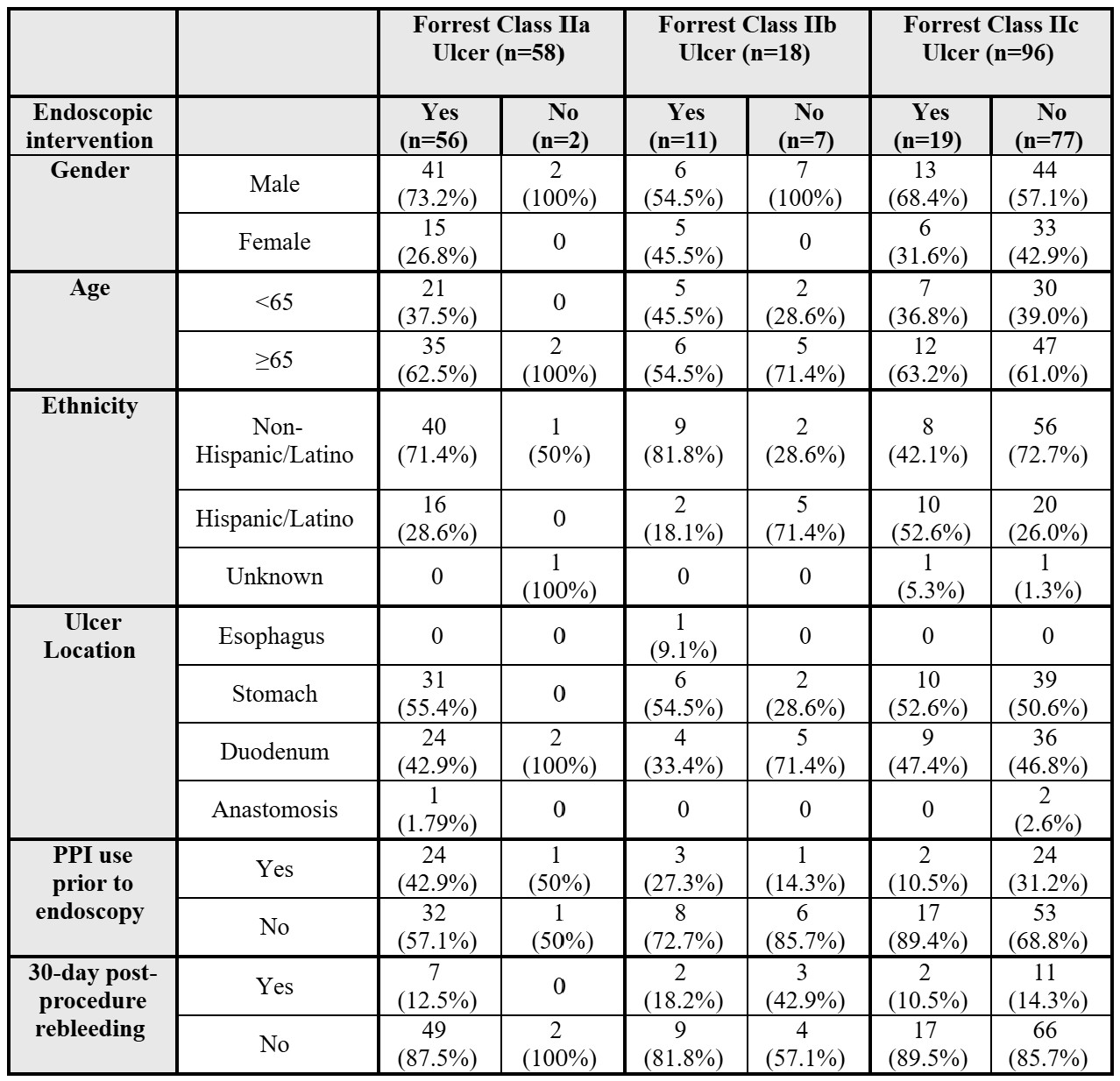
Figure: Table 2: Endoscopic Intervention and Rebleeding Rates Based on Forrest Classification
Disclosures:
Sonia Mehra indicated no relevant financial relationships.
Soha Noorani indicated no relevant financial relationships.
Bharati Dev indicated no relevant financial relationships.
Michael Smith: Castle Biosciences – Consultant. CDx Diagnostics – Consultant. Lucid Diagnostics – Consultant. Provation Software – Consultant. Sanofi – Consultant. Steris Endoscopy – Consultant.
Sonia Mehra, MD1, Soha Noorani, DO2, Bharati Dev, DO3, Michael S.. Smith, MD, MBA4. P0911 - The Conundrum of Managing Forrest Class IIb Ulcers: Real-World Findings From 2 Large Urban Medical Centers, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Mount Sinai West & Morningside, New York, NY; 2Mount Sinai Morningside, Icahn School of Medicine at Mount Sinai, New York, NY; 3Mount Sinai West, Icahn School of Medicine at Mount Sinai, New York, NY; 4Icahn School of Medicine at Mount Sinai, New York, NY
Introduction: Management of Forrest II ulcers varies based on endoscopic appearance. Although IIa (non-bleeding visible vessel) and IIc (flat pigmented spot) ulcers have clear guidance on endoscopic hemostatic intervention, recommendations for IIb ulcers (adherent clot) are not well defined. Our aim is to evaluate real-world adherence to guidelines for Forrest II ulcers and to assess rebleeding risk based on guideline-appropriate intervention, including IIb ulcers where intervention is indeterminate.
Methods: A retrospective chart analysis was conducted on patients with Forrest II ulcers from 2019-2024 at two urban academic centers. Patient demographic characteristics and history of prior proton pump inhibitor (PPI) use were collected from electronic records. Ulcer class, site, and endoscopic intervention were obtained from procedure reports. The primary outcome was to assess 30-day rebleeding rate based on hemostatic intervention. Chi-square analysis was conducted to evaluate variables of interest.
Results: Of 172 patients with fully available data (65.7% male, mean age 67.6 years), the majority of patients had Forrest IIc ulcers (55.8%), with most located in the stomach (51.2%) or duodenum (46.5%) (Table 1). As per guidelines, endoscopic intervention was performed in 96.6% of Forrest IIa ulcers, while 80.2% of Forrest IIc ulcers had no intervention. Although most (61.1%) IIb ulcers were managed endoscopically, there was a higher relative overall 30-day post-endoscopy rebleeding risk (27.8%) in this group than observed in Forrest IIa (12.1%) or IIc (13.5%) ulcers. There was a lower 30-day rate of rebleeding in patients with Forrest IIb ulcers receiving intervention (18.2%) compared to IIb patients without intervention (42.9%) (Table 2). Of note, 30-day rebleeding rates for Forrest IIc ulcers were similar to those of IIa ulcers, regardless of intervention.
Discussion: Treatment of Forrest IIa and IIc ulcers generally followed current guidelines. Forrest IIb ulcers were much less commonly identified and provided a management dilemma, as there are no strict guidelines on the use of hemostatic therapy. These results suggest that intervention may decrease 30-day Class IIb rebleeding rates to around those seen with other Forrest II lesions. When feasible, unroofing adherent clot to expose the ulcer bed and any visible vessel may permit reclassification to IIa or IIc, and therefore provide better guidance on appropriate management with an increased risk of rebleeding.
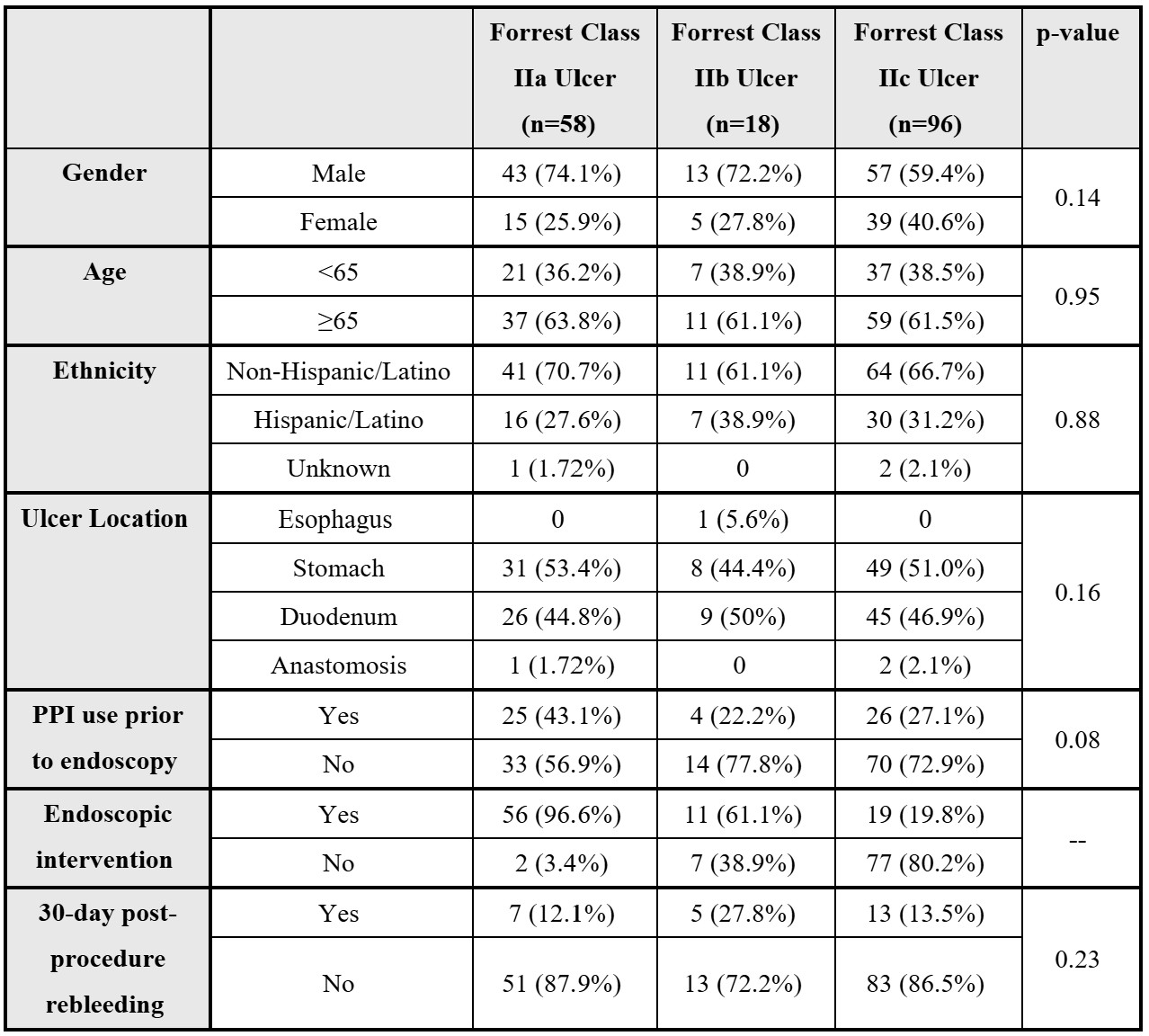
Figure: Table 1: Patient Characteristics Based On Forrest Classification
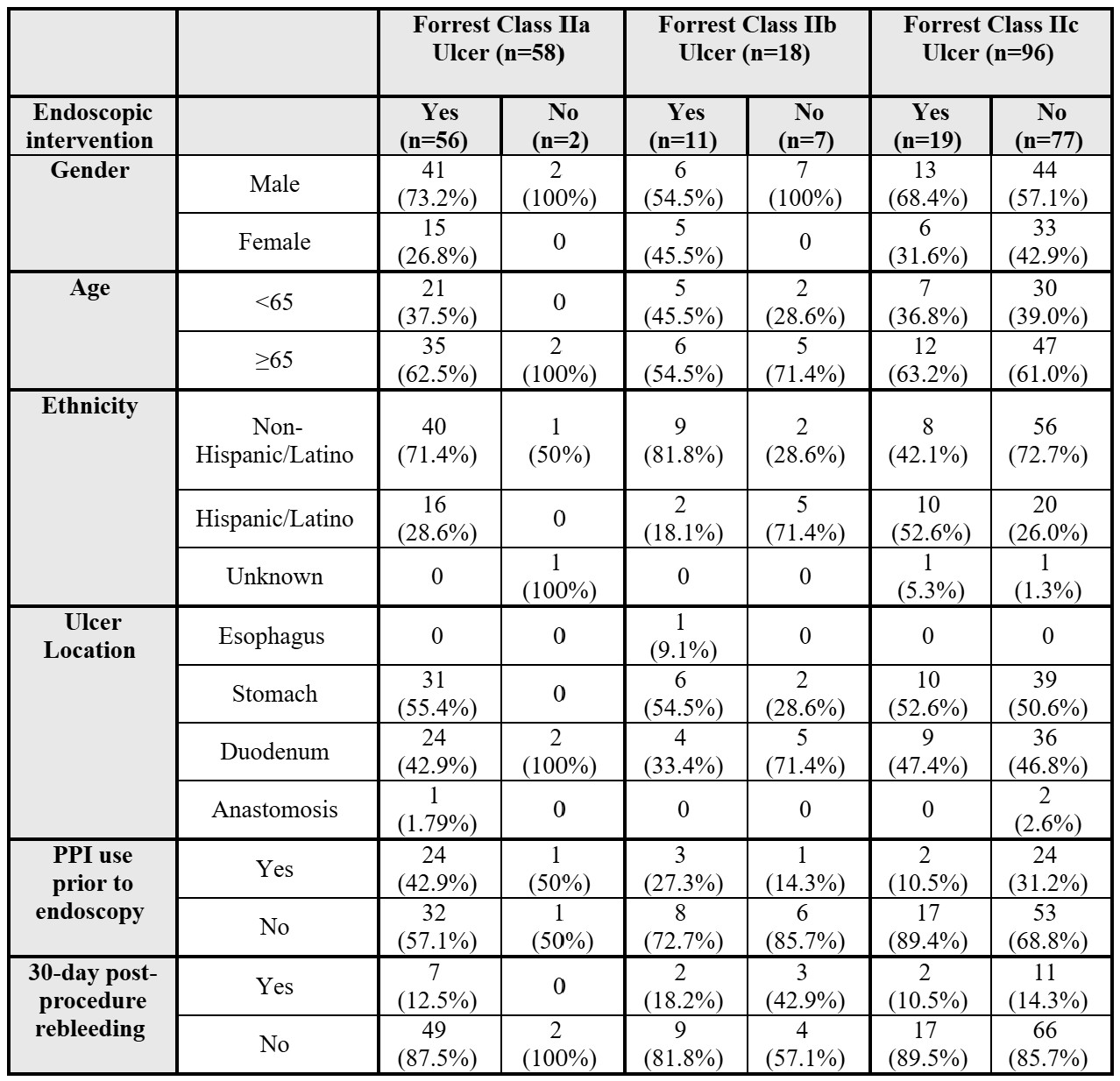
Figure: Table 2: Endoscopic Intervention and Rebleeding Rates Based on Forrest Classification
Disclosures:
Sonia Mehra indicated no relevant financial relationships.
Soha Noorani indicated no relevant financial relationships.
Bharati Dev indicated no relevant financial relationships.
Michael Smith: Castle Biosciences – Consultant. CDx Diagnostics – Consultant. Lucid Diagnostics – Consultant. Provation Software – Consultant. Sanofi – Consultant. Steris Endoscopy – Consultant.
Sonia Mehra, MD1, Soha Noorani, DO2, Bharati Dev, DO3, Michael S.. Smith, MD, MBA4. P0911 - The Conundrum of Managing Forrest Class IIb Ulcers: Real-World Findings From 2 Large Urban Medical Centers, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.

