Sunday Poster Session
Category: GI Bleeding
P0906 - Inappropriate Utilization of Fecal Occult Blood Testing in Acute Care Settings: A Quality Improvement Analysis of Impact on Clinical Decision Making
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall
- MS
Michelle Shi, MD
Northwell Health
Manhasset, NY
Presenting Author(s)
Michelle Shi, MD1, Jeffrey Lowell, MD1, Michael Attanasi, MD1, Justin Lin, MD2, Anthony Papale, MD1, Mark Cubillan, MD3, Jared Honigman, DO1
1Northwell Health, Manhasset, NY; 2Northwell Health, New Hyde Park, NY; 3Northwest Health, Manhasset, NY
Introduction: Fecal occult blood testing (FOBT) was validated as a colorectal cancer screening test in average risk patients. Despite lacking evidence for alternative uses, FOBT is frequently utilized off-label in acute care settings for evaluating anemia or suspected gastrointestinal (GI) hemorrhage. At our center, 1977 FOBT tests were performed in an off-label manner in a 12-month period. This pilot study investigated FOBT utility in detecting GI bleeding (GIB) in acute care settings and its impact on clinical decision-making.
Methods: This is a quality improvement project performed at a large tertiary academic medical center. We analyzed 100 patients who received an FOBT from 11/2022-10/2023 either in the emergency department or after admission. Data collection included FOBT results, hemoglobin levels, anemia workup, rectal examinations, endoscopic procedures, length of stay (LOS), and GI lesions. Statistical analyses included chi-square and U-test.
Results: Positive FOBT results were associated with a 19.5% endoscopic intervention rate (median time to endoscopy: 2 days) with 75% positive predictive value for hemorrhagic sources. Negative FOBT results had a 32.2% intervention rate (median time to endoscopy: 3 days) with a 63.2% false negative rate. Overall FOBT sensitivity for detecting endoscopic findings was 33.3%. FOBT positivity rates were similar between ED (26.3%) and inpatient (44.4%) settings (p=0.24), with comparable endoscopic intervention rates for both positive (20.0% vs 19.4%) and negative (28.6% vs 33.3%) results. GI consultation was more frequent with negative FOBT (61%) results than positive (39%) results (p=0.0498). However, endoscopic intervention rates did not significantly differ between positive and negative FOBT results (p=0.24). Median LOS was also comparable between positive (7 days, IQR 4-12) and negative (8 days, IQR 3-13.5) FOBT results (p=0.64). (Figure 1 & Figure 2)
Discussion: This study demonstrates that FOBT results in acute care settings neither effectively guide clinical management nor influence decisions regarding endoscopic intervention or length of stay. However, GI consultation rate was positively correlated with negative FOBT testing suggesting clinical suspicion often overrode FOBT test results. While larger studies are needed for comprehensive cost-effectiveness analysis measuring healthcare burden, the poor sensitivity and high false negative rate suggest FOBT provides minimal diagnostic value for investigating suspected GIB in hospitalized patients.
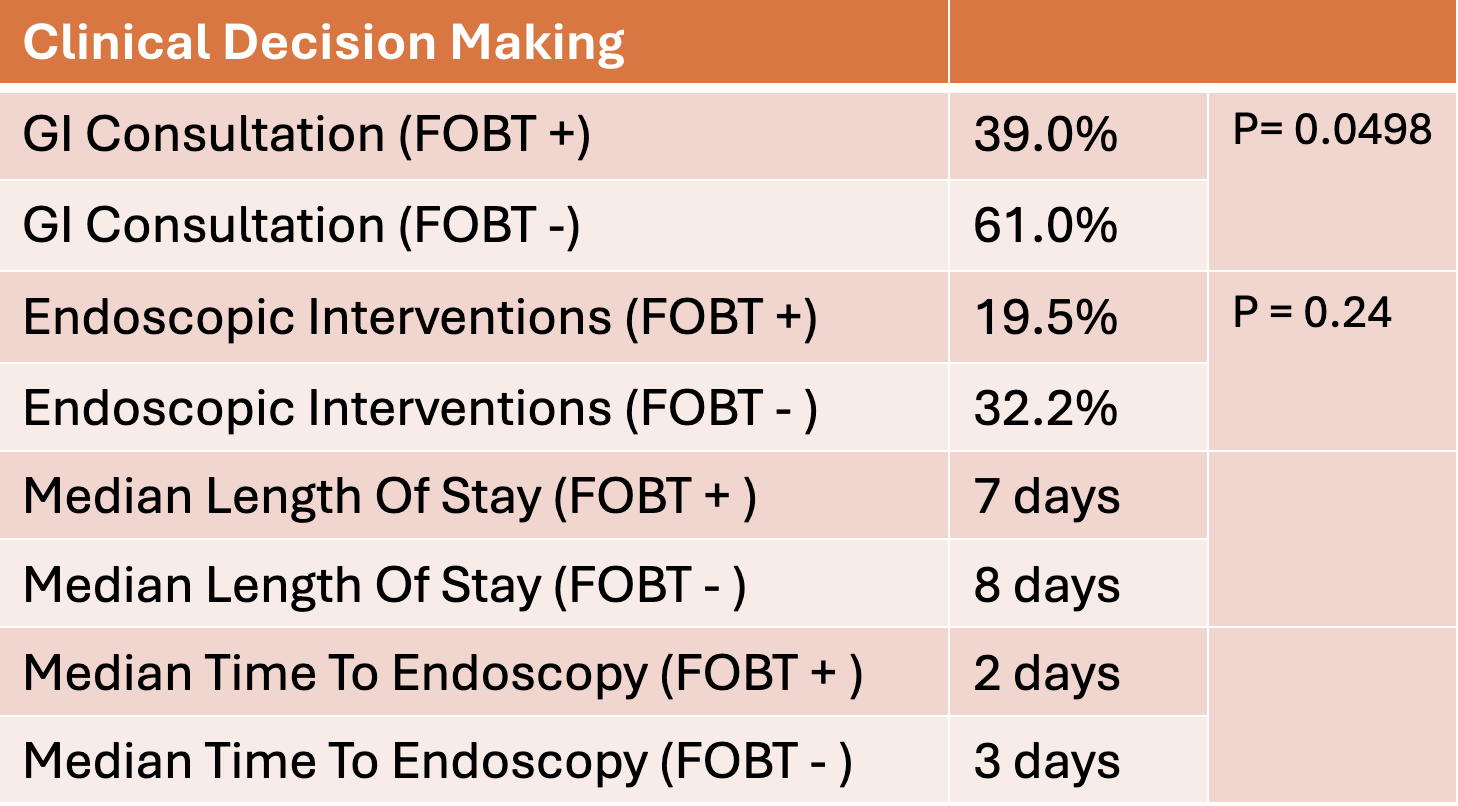
Figure: Diagnostic Value of FOBT in GI bleed Investigation
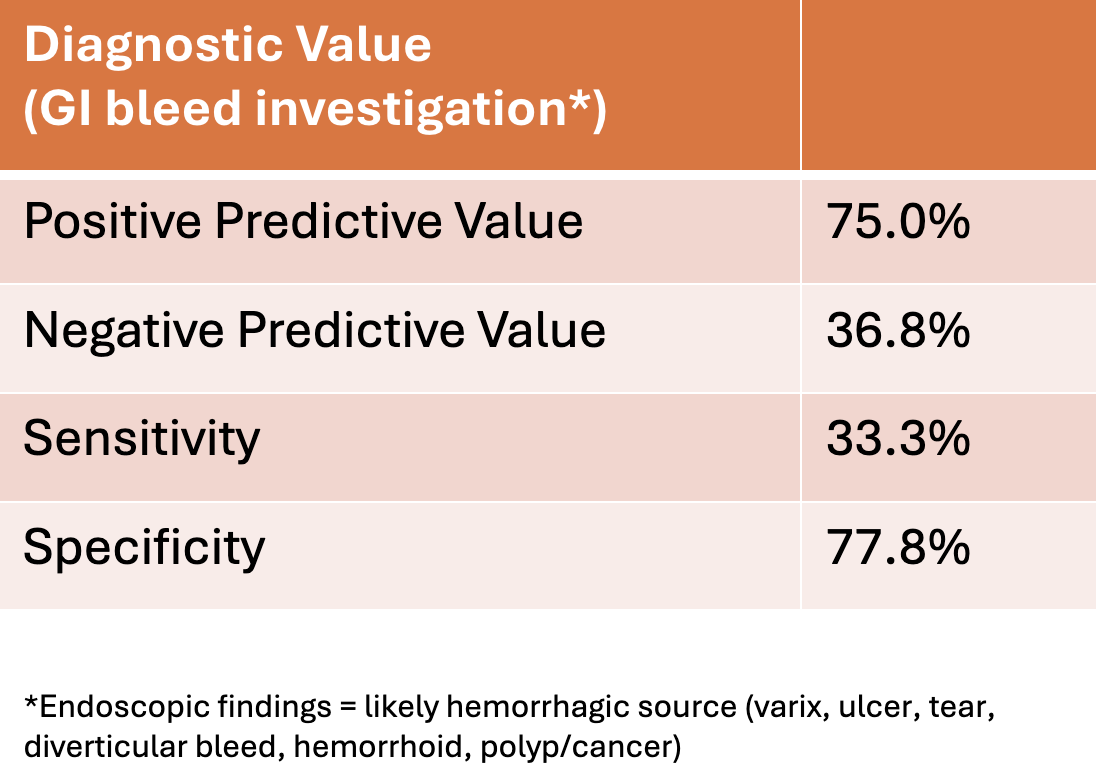
Figure: Diagnostic Value of FOBT in Clinical Decision Making
Disclosures:
Michelle Shi indicated no relevant financial relationships.
Jeffrey Lowell indicated no relevant financial relationships.
Michael Attanasi indicated no relevant financial relationships.
Justin Lin indicated no relevant financial relationships.
Anthony Papale indicated no relevant financial relationships.
Mark Cubillan indicated no relevant financial relationships.
Jared Honigman indicated no relevant financial relationships.
Michelle Shi, MD1, Jeffrey Lowell, MD1, Michael Attanasi, MD1, Justin Lin, MD2, Anthony Papale, MD1, Mark Cubillan, MD3, Jared Honigman, DO1. P0906 - Inappropriate Utilization of Fecal Occult Blood Testing in Acute Care Settings: A Quality Improvement Analysis of Impact on Clinical Decision Making, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Northwell Health, Manhasset, NY; 2Northwell Health, New Hyde Park, NY; 3Northwest Health, Manhasset, NY
Introduction: Fecal occult blood testing (FOBT) was validated as a colorectal cancer screening test in average risk patients. Despite lacking evidence for alternative uses, FOBT is frequently utilized off-label in acute care settings for evaluating anemia or suspected gastrointestinal (GI) hemorrhage. At our center, 1977 FOBT tests were performed in an off-label manner in a 12-month period. This pilot study investigated FOBT utility in detecting GI bleeding (GIB) in acute care settings and its impact on clinical decision-making.
Methods: This is a quality improvement project performed at a large tertiary academic medical center. We analyzed 100 patients who received an FOBT from 11/2022-10/2023 either in the emergency department or after admission. Data collection included FOBT results, hemoglobin levels, anemia workup, rectal examinations, endoscopic procedures, length of stay (LOS), and GI lesions. Statistical analyses included chi-square and U-test.
Results: Positive FOBT results were associated with a 19.5% endoscopic intervention rate (median time to endoscopy: 2 days) with 75% positive predictive value for hemorrhagic sources. Negative FOBT results had a 32.2% intervention rate (median time to endoscopy: 3 days) with a 63.2% false negative rate. Overall FOBT sensitivity for detecting endoscopic findings was 33.3%. FOBT positivity rates were similar between ED (26.3%) and inpatient (44.4%) settings (p=0.24), with comparable endoscopic intervention rates for both positive (20.0% vs 19.4%) and negative (28.6% vs 33.3%) results. GI consultation was more frequent with negative FOBT (61%) results than positive (39%) results (p=0.0498). However, endoscopic intervention rates did not significantly differ between positive and negative FOBT results (p=0.24). Median LOS was also comparable between positive (7 days, IQR 4-12) and negative (8 days, IQR 3-13.5) FOBT results (p=0.64). (Figure 1 & Figure 2)
Discussion: This study demonstrates that FOBT results in acute care settings neither effectively guide clinical management nor influence decisions regarding endoscopic intervention or length of stay. However, GI consultation rate was positively correlated with negative FOBT testing suggesting clinical suspicion often overrode FOBT test results. While larger studies are needed for comprehensive cost-effectiveness analysis measuring healthcare burden, the poor sensitivity and high false negative rate suggest FOBT provides minimal diagnostic value for investigating suspected GIB in hospitalized patients.
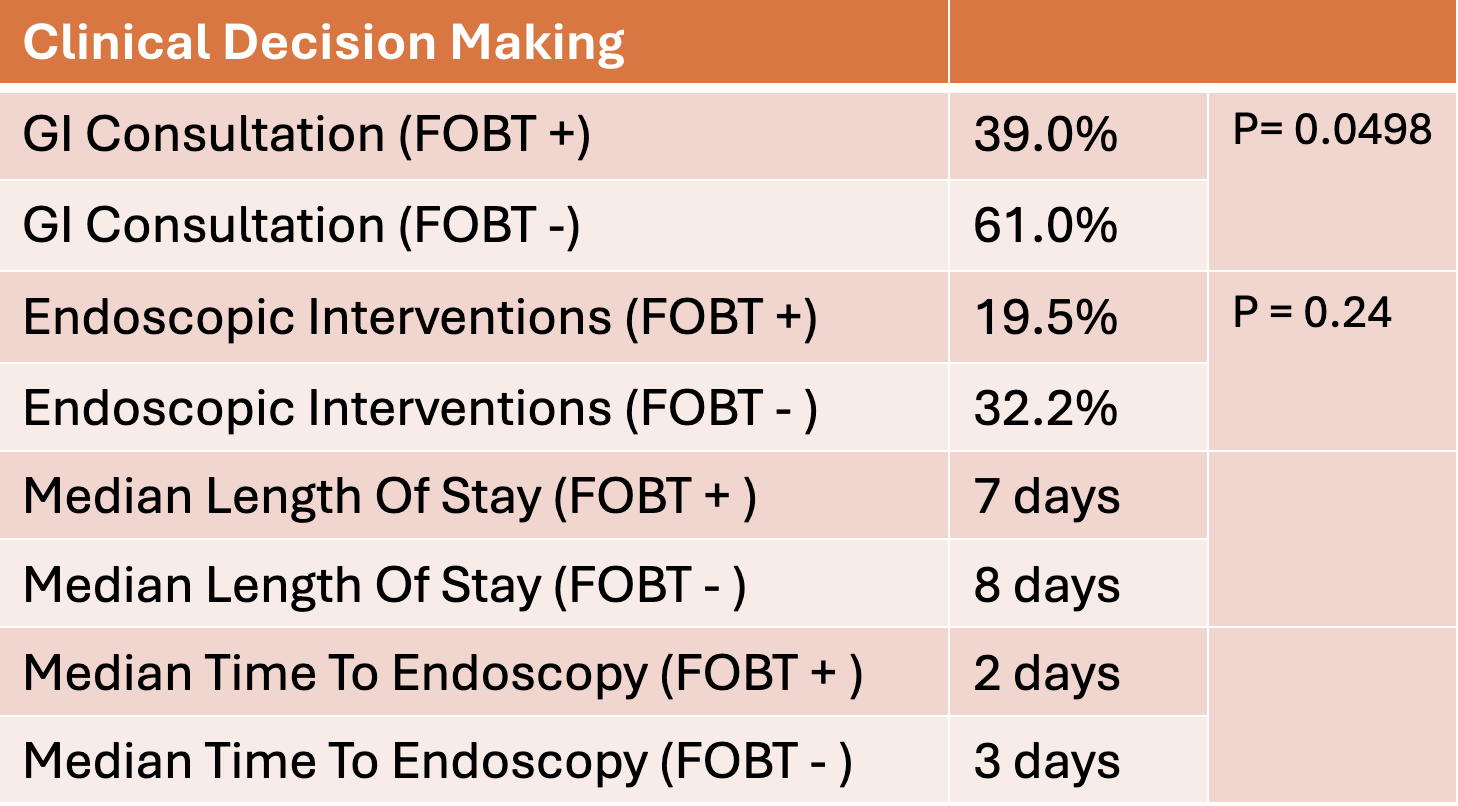
Figure: Diagnostic Value of FOBT in GI bleed Investigation
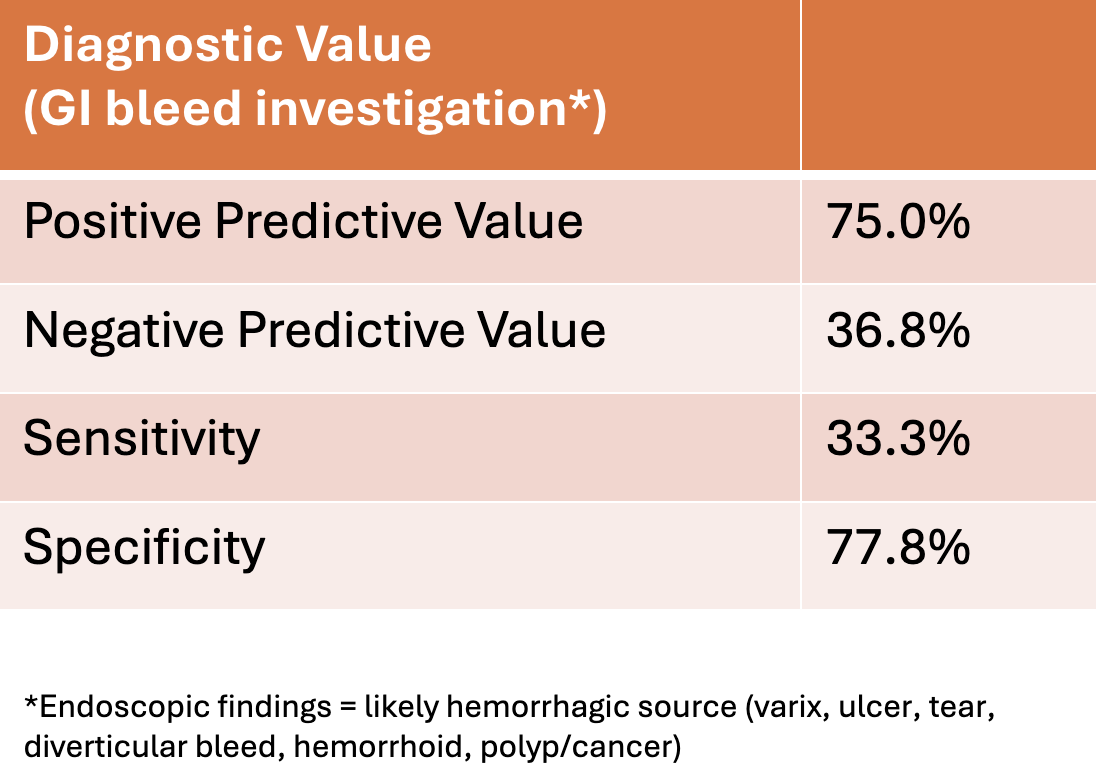
Figure: Diagnostic Value of FOBT in Clinical Decision Making
Disclosures:
Michelle Shi indicated no relevant financial relationships.
Jeffrey Lowell indicated no relevant financial relationships.
Michael Attanasi indicated no relevant financial relationships.
Justin Lin indicated no relevant financial relationships.
Anthony Papale indicated no relevant financial relationships.
Mark Cubillan indicated no relevant financial relationships.
Jared Honigman indicated no relevant financial relationships.
Michelle Shi, MD1, Jeffrey Lowell, MD1, Michael Attanasi, MD1, Justin Lin, MD2, Anthony Papale, MD1, Mark Cubillan, MD3, Jared Honigman, DO1. P0906 - Inappropriate Utilization of Fecal Occult Blood Testing in Acute Care Settings: A Quality Improvement Analysis of Impact on Clinical Decision Making, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
