Sunday Poster Session
Category: GI Bleeding
P0969 - A Rare Case of a Portal Vein Pseudoaneurysm
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall
- TL
Tayna Latortue, MD (she/her/hers)
University of Florida
Gainesville, FL
Presenting Author(s)
Tayna Latortue, MD1, Michael Ali, MD1, Jack Burcher, MD1, Manuel Amaris, MD2
1University of Florida, Gainesville, FL; 2University of Florida, Division of Gastroenterology, Hepatology and Nutrition, Gainesville, FL
Introduction: Pseudoaneurysms arise due to trauma, inflammation, infection or iatrogenic causes including procedures. The prevalence of portal venous aneurysms, which include pseudoaneurysms, is less than 0.4%. We present a case of a portal venous pseudoaneurysm secondary to a Whipple procedure that caused recurrent bleeding.
Case Description/
Methods: A 61-year-old female with a past medical history of cholangiocarcinoma status post Whipple procedure with Billroth II and portal vein repair in December 2022 presented to the hospital in September 2024 with hematochezia. A computed tomography (CT) of the abdomen and pelvis (A/P) with gastrointestinal bleed (GI) protocol showed a large pseudoaneurysm at the portal vein confluence anteriorly that was 28x20x22mm in size. Operative management was not offered due to the location of the bleed. The patient had no further drops in hemoglobin or ongoing melena and was discharged home. She represented in January and February 2025 with melena and hematochezia. Workup included a CT A/P showed the portal vein pseudoaneurysm at 20x20x25mm in size, an upper endoscopy, colonoscopy, double balloon anterograde enteroscopy and double balloon retrograde enteroscopy that were all negative for a bleed, and a video capsule endoscopy that showed an illeal angioectasia without bleeding. She was sent home on subcutaneous octreotide. She then presented from clinic due to melena. She had hematemesis that led to hemorrhagic shock. Small bowel enteroscopy showed mucosal changes in the efferent jejunum, concerning for active bleeding. A CT GI bleed did not show active bleeding. Pancreatobiliary surgery was consulted due to concern a fistula between the portal vein pseudoaneurysm and pancreaticojejenum anastomosis site. She underwent a complete pancreatectomy, portal vein reconstruction with a peritoneal patch, and a splenectomy.
Discussion: Portal vein pseudoaneurysms are a rare phenomenon after a Whipple procedure. More conservative measurements were tried in this patient given the limitations of procedural management. The decision was made to send the patient home since her bleeding resolved after initial presentation with the recommendation to present back to the ER if she had more bleeding. She presented three more times for bleeding over six months, requiring the massive transfusion protocol and admission to the medical intensive care unit for hemorrhagic shock. Her course highlights how symptomatic a portal vein pseudoaneurysm can be, as well as the intermittent of the bleeding.
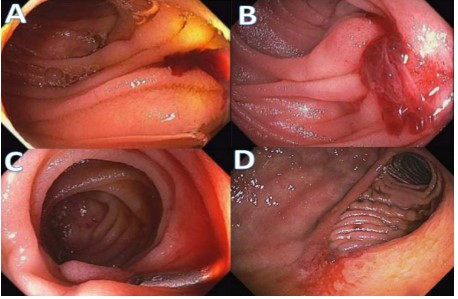
Figure: Figure 1: CT A/P with intravenous contrast showing portal vein pseudoaneurysm measuring 20.1x 28.1 x 21.8 mm on a transverse and coronal view (from 9/30/2024)
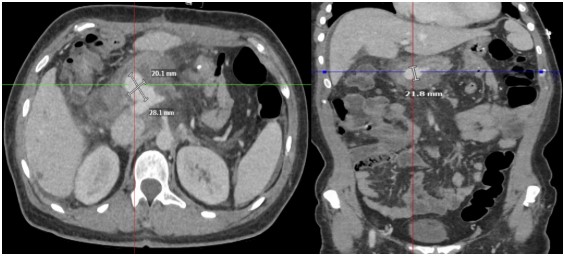
Figure: Figure 2: Results from small bowel enteroscopy. A. Bleeding in jejunal limb near pancreatojejunal anastomsis B. Bleeding in jejunal limb near pancreatojejunal anastomosis C. Bleeding in jejunal limb near pancreatojejunal anastomosis with clip placed both proximal and distal D. Friable mucosa at gastrojejunal anastomosis site
Disclosures:
Tayna Latortue indicated no relevant financial relationships.
Michael Ali indicated no relevant financial relationships.
Jack Burcher indicated no relevant financial relationships.
Manuel Amaris indicated no relevant financial relationships.
Tayna Latortue, MD1, Michael Ali, MD1, Jack Burcher, MD1, Manuel Amaris, MD2. P0969 - A Rare Case of a Portal Vein Pseudoaneurysm, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1University of Florida, Gainesville, FL; 2University of Florida, Division of Gastroenterology, Hepatology and Nutrition, Gainesville, FL
Introduction: Pseudoaneurysms arise due to trauma, inflammation, infection or iatrogenic causes including procedures. The prevalence of portal venous aneurysms, which include pseudoaneurysms, is less than 0.4%. We present a case of a portal venous pseudoaneurysm secondary to a Whipple procedure that caused recurrent bleeding.
Case Description/
Methods: A 61-year-old female with a past medical history of cholangiocarcinoma status post Whipple procedure with Billroth II and portal vein repair in December 2022 presented to the hospital in September 2024 with hematochezia. A computed tomography (CT) of the abdomen and pelvis (A/P) with gastrointestinal bleed (GI) protocol showed a large pseudoaneurysm at the portal vein confluence anteriorly that was 28x20x22mm in size. Operative management was not offered due to the location of the bleed. The patient had no further drops in hemoglobin or ongoing melena and was discharged home. She represented in January and February 2025 with melena and hematochezia. Workup included a CT A/P showed the portal vein pseudoaneurysm at 20x20x25mm in size, an upper endoscopy, colonoscopy, double balloon anterograde enteroscopy and double balloon retrograde enteroscopy that were all negative for a bleed, and a video capsule endoscopy that showed an illeal angioectasia without bleeding. She was sent home on subcutaneous octreotide. She then presented from clinic due to melena. She had hematemesis that led to hemorrhagic shock. Small bowel enteroscopy showed mucosal changes in the efferent jejunum, concerning for active bleeding. A CT GI bleed did not show active bleeding. Pancreatobiliary surgery was consulted due to concern a fistula between the portal vein pseudoaneurysm and pancreaticojejenum anastomosis site. She underwent a complete pancreatectomy, portal vein reconstruction with a peritoneal patch, and a splenectomy.
Discussion: Portal vein pseudoaneurysms are a rare phenomenon after a Whipple procedure. More conservative measurements were tried in this patient given the limitations of procedural management. The decision was made to send the patient home since her bleeding resolved after initial presentation with the recommendation to present back to the ER if she had more bleeding. She presented three more times for bleeding over six months, requiring the massive transfusion protocol and admission to the medical intensive care unit for hemorrhagic shock. Her course highlights how symptomatic a portal vein pseudoaneurysm can be, as well as the intermittent of the bleeding.
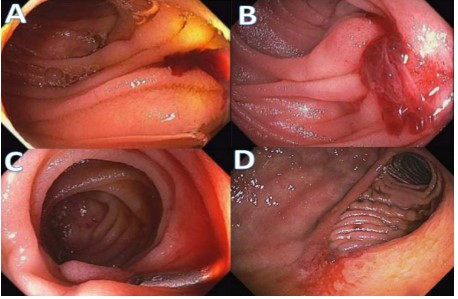
Figure: Figure 1: CT A/P with intravenous contrast showing portal vein pseudoaneurysm measuring 20.1x 28.1 x 21.8 mm on a transverse and coronal view (from 9/30/2024)
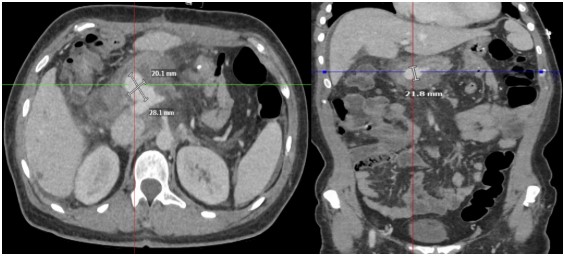
Figure: Figure 2: Results from small bowel enteroscopy. A. Bleeding in jejunal limb near pancreatojejunal anastomsis B. Bleeding in jejunal limb near pancreatojejunal anastomosis C. Bleeding in jejunal limb near pancreatojejunal anastomosis with clip placed both proximal and distal D. Friable mucosa at gastrojejunal anastomosis site
Disclosures:
Tayna Latortue indicated no relevant financial relationships.
Michael Ali indicated no relevant financial relationships.
Jack Burcher indicated no relevant financial relationships.
Manuel Amaris indicated no relevant financial relationships.
Tayna Latortue, MD1, Michael Ali, MD1, Jack Burcher, MD1, Manuel Amaris, MD2. P0969 - A Rare Case of a Portal Vein Pseudoaneurysm, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
