Sunday Poster Session
Category: GI Bleeding
P0967 - The Bleeding Duodenal Varix Dilemma: An Atypical Endoscopic Presentation of Duodenal Variceal Bleed
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall

Medora Doris Rodrigues, MD, MPH
The Ohio State University Wexner Medical Center
Columbus, OH
Presenting Author(s)
Medora Doris. Rodrigues, MD, MPH1, Mena Saad, DO2, Jonathan Scott, MD3, Wichit Srikureja, MD4, Khalid Mumtaz, MBBS, MSc1
1The Ohio State University Wexner Medical Center, Columbus, OH; 2Riverside University Health System, Moreno Valley, CA; 3Riverside University Health System, Riverside, CA; 4Providence Sacred Heart Medical Center, Spokane, WA
Introduction: Cirrhosis is a major risk factor for gastrointestinal bleeding (GIB), typically from esophageal (~70%) or gastric (10–30%) varices. Duodenal varices are rare (~0.4%) but carry high mortality (up to 40%), necessitating prompt recognition and management.
Case Description/
Methods: A 66-year-old obese woman (BMI 54.8) with newly diagnosed MASH cirrhosis was transferred with hematemesis, melena, and hypotension. Her history included type 2 diabetes, hypertension, and ovarian cancer (post-surgery/chemotherapy). She received blood products at the OSH but remained hypotensive and tachycardic. She denied alcohol or anticoagulant use but reported chronic NSAID use. She was admitted to the ICU and underwent intubation, resuscitation, and initiation of IV pantoprazole, octreotide, and ceftriaxone for SBP prophylaxis. Labs showed lactate 10, hemoglobin 8.8, platelets 96, AST 78, ALT 48, total bilirubin 3.1, albumin 2.9, total protein 5.6, and creatinine 0.79. MELD was 15. EGD showed no esophageal or gastric luminal stigmata of liver disease. An actively bleeding lesion was found in the second part of the duodenum: 4 mm submucosal bulge with central umbilication and clot (fig 1a), initially suspected to be a Dieulafoy’s lesion. Epinephrine injection worsened bleeding despite multiple aliquots. Two metallic hemoclips were ineffective; three additional clips (fig 1b,c) were placed, achieving partial hemostasis, and complete hemostasis was then achieved after Hemostatic powder was applied (fig 1d). Post-procedure CT A/P showed cirrhosis and a small non-bleeding duodenal varix with inflow from a duodenal branch of the SMV and outflow to the IVC near the right gonadal vein (fig 2a,b). She recovered with durable hemostasis, was extubated, and discharged in stable condition.
Discussion: This case underscores challenges in managing ectopic duodenal variceal bleeding. Duodenal varices can mimic Dieulafoy’s lesions, leading to misdiagnosis and inadequate interventions. In this case, misclassification of the lesion as a Dieulafoy’s prompted standard hemostatic techniques epinephrine injection and hemoclips which not only failed but exacerbated the bleeding.
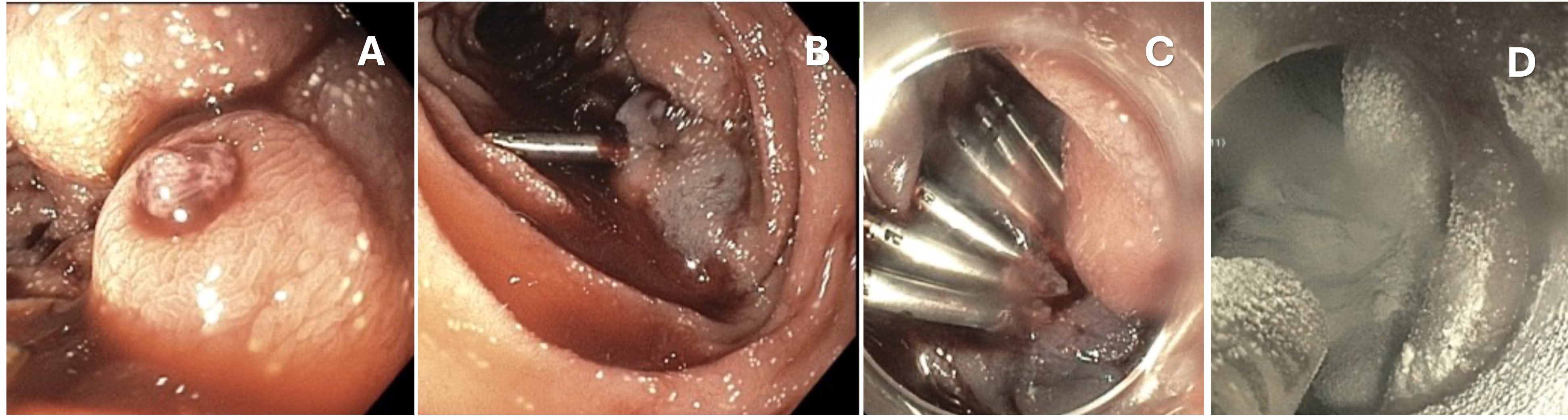
Figure: Figure 1: 1A Focal 4 mm sub-mucosal bulge with a central umbilication with an embedded clot. 1B Incomplete
hemostasis with epinephrine injection and singular hemostatic clip placement. Hemostasis achieved with multiple
clips (1C) placement and hemospray (1D)
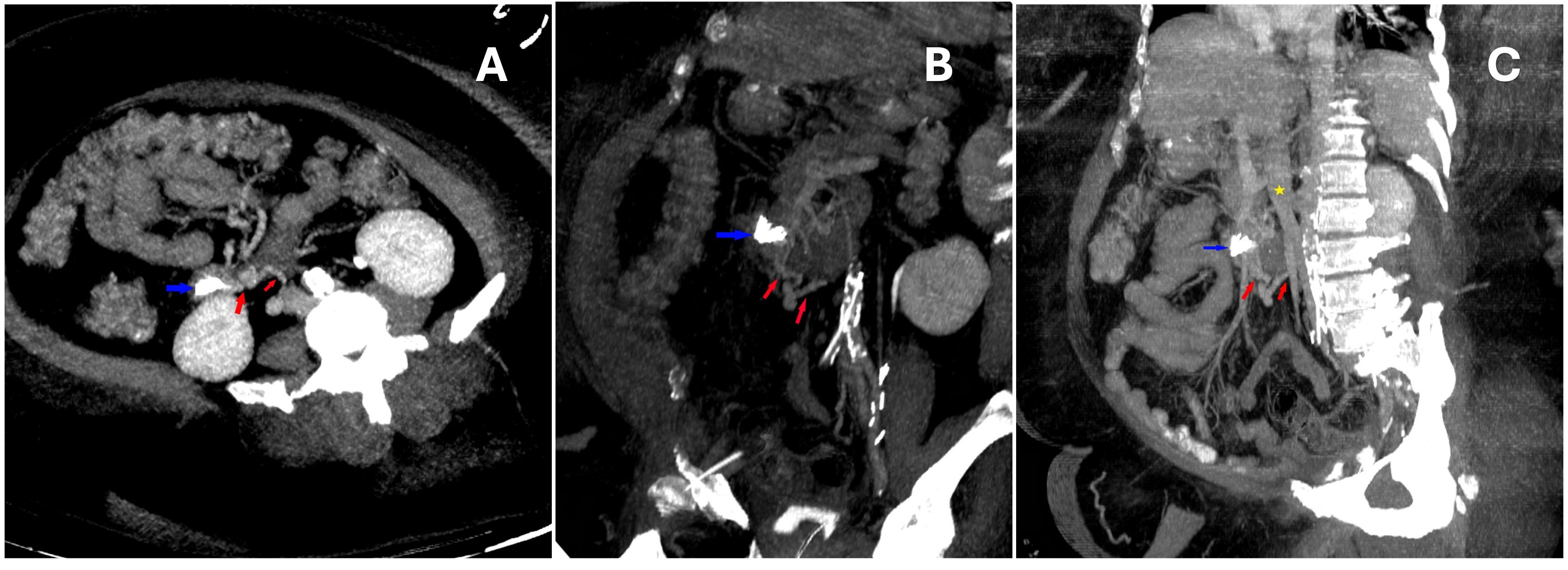
Figure: Figure 2: 2A&B Axial and Coronal CT demonstrating endoscopic clips in the wall of the duodenum(blue arrow) with varix complex and draining outflow vein (red arrows). 2C Maximum intensity oblique coronal CT image demonstrating endoscopic clips in the wall of the duodenum(blue arrow) with varix complex and draining outflow vein (red arrows). Inferior vena cava (yellow star).
Disclosures:
Medora Rodrigues indicated no relevant financial relationships.
Mena Saad indicated no relevant financial relationships.
Jonathan Scott indicated no relevant financial relationships.
Wichit Srikureja indicated no relevant financial relationships.
Khalid Mumtaz indicated no relevant financial relationships.
Medora Doris. Rodrigues, MD, MPH1, Mena Saad, DO2, Jonathan Scott, MD3, Wichit Srikureja, MD4, Khalid Mumtaz, MBBS, MSc1. P0967 - The Bleeding Duodenal Varix Dilemma: An Atypical Endoscopic Presentation of Duodenal Variceal Bleed, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1The Ohio State University Wexner Medical Center, Columbus, OH; 2Riverside University Health System, Moreno Valley, CA; 3Riverside University Health System, Riverside, CA; 4Providence Sacred Heart Medical Center, Spokane, WA
Introduction: Cirrhosis is a major risk factor for gastrointestinal bleeding (GIB), typically from esophageal (~70%) or gastric (10–30%) varices. Duodenal varices are rare (~0.4%) but carry high mortality (up to 40%), necessitating prompt recognition and management.
Case Description/
Methods: A 66-year-old obese woman (BMI 54.8) with newly diagnosed MASH cirrhosis was transferred with hematemesis, melena, and hypotension. Her history included type 2 diabetes, hypertension, and ovarian cancer (post-surgery/chemotherapy). She received blood products at the OSH but remained hypotensive and tachycardic. She denied alcohol or anticoagulant use but reported chronic NSAID use. She was admitted to the ICU and underwent intubation, resuscitation, and initiation of IV pantoprazole, octreotide, and ceftriaxone for SBP prophylaxis. Labs showed lactate 10, hemoglobin 8.8, platelets 96, AST 78, ALT 48, total bilirubin 3.1, albumin 2.9, total protein 5.6, and creatinine 0.79. MELD was 15. EGD showed no esophageal or gastric luminal stigmata of liver disease. An actively bleeding lesion was found in the second part of the duodenum: 4 mm submucosal bulge with central umbilication and clot (fig 1a), initially suspected to be a Dieulafoy’s lesion. Epinephrine injection worsened bleeding despite multiple aliquots. Two metallic hemoclips were ineffective; three additional clips (fig 1b,c) were placed, achieving partial hemostasis, and complete hemostasis was then achieved after Hemostatic powder was applied (fig 1d). Post-procedure CT A/P showed cirrhosis and a small non-bleeding duodenal varix with inflow from a duodenal branch of the SMV and outflow to the IVC near the right gonadal vein (fig 2a,b). She recovered with durable hemostasis, was extubated, and discharged in stable condition.
Discussion: This case underscores challenges in managing ectopic duodenal variceal bleeding. Duodenal varices can mimic Dieulafoy’s lesions, leading to misdiagnosis and inadequate interventions. In this case, misclassification of the lesion as a Dieulafoy’s prompted standard hemostatic techniques epinephrine injection and hemoclips which not only failed but exacerbated the bleeding.
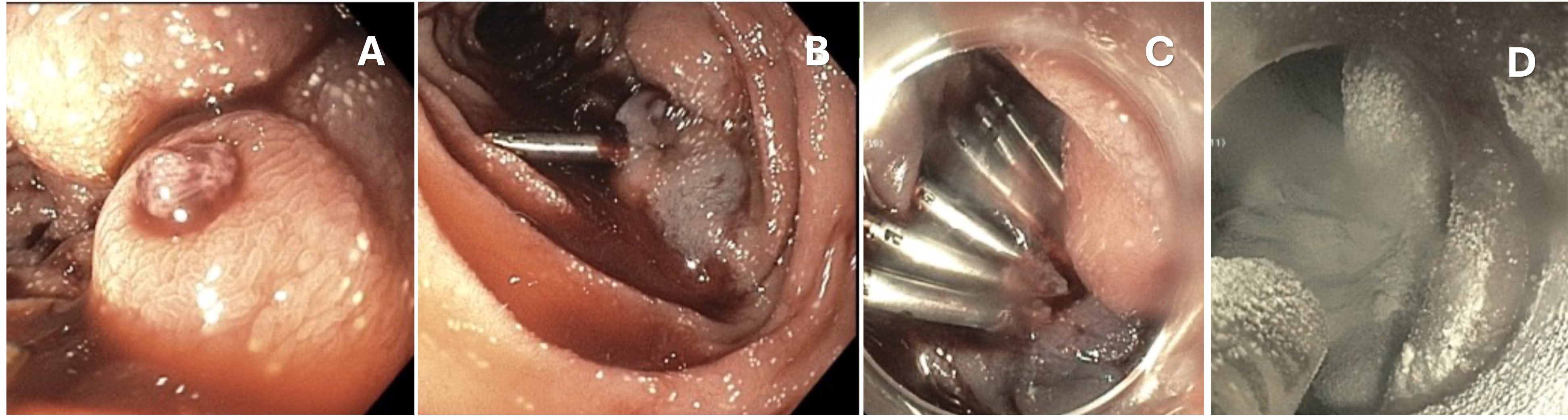
Figure: Figure 1: 1A Focal 4 mm sub-mucosal bulge with a central umbilication with an embedded clot. 1B Incomplete
hemostasis with epinephrine injection and singular hemostatic clip placement. Hemostasis achieved with multiple
clips (1C) placement and hemospray (1D)
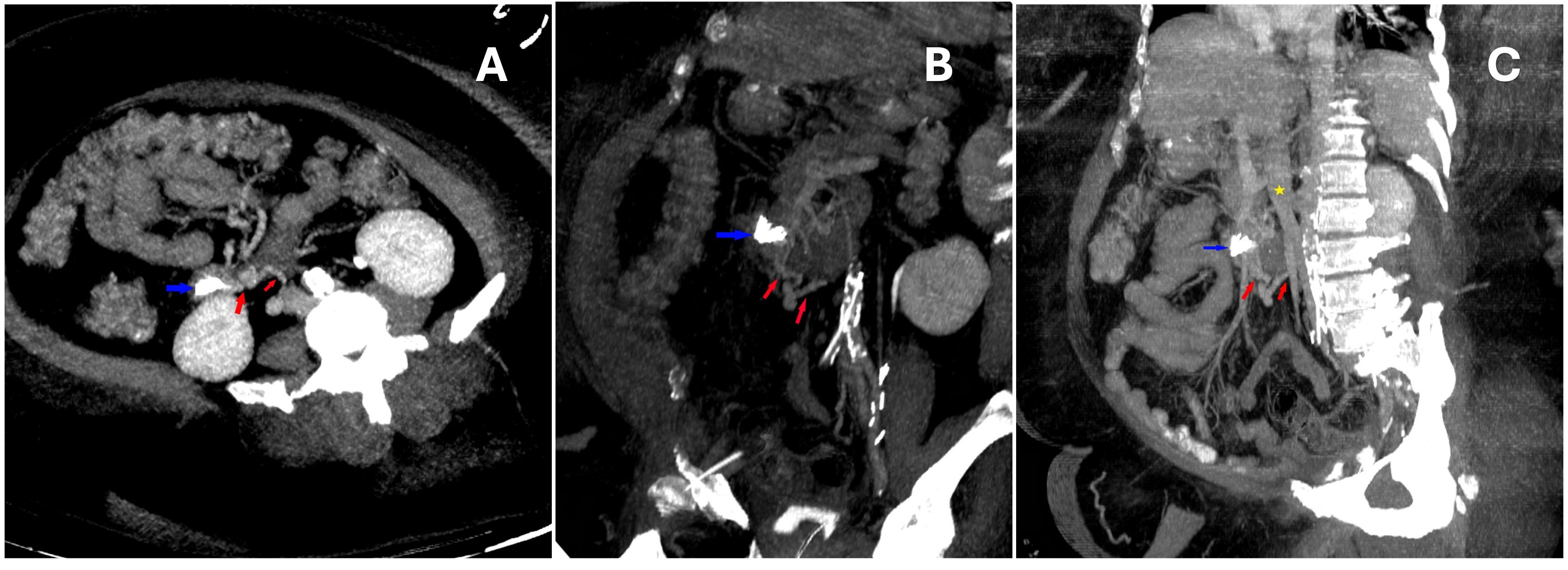
Figure: Figure 2: 2A&B Axial and Coronal CT demonstrating endoscopic clips in the wall of the duodenum(blue arrow) with varix complex and draining outflow vein (red arrows). 2C Maximum intensity oblique coronal CT image demonstrating endoscopic clips in the wall of the duodenum(blue arrow) with varix complex and draining outflow vein (red arrows). Inferior vena cava (yellow star).
Disclosures:
Medora Rodrigues indicated no relevant financial relationships.
Mena Saad indicated no relevant financial relationships.
Jonathan Scott indicated no relevant financial relationships.
Wichit Srikureja indicated no relevant financial relationships.
Khalid Mumtaz indicated no relevant financial relationships.
Medora Doris. Rodrigues, MD, MPH1, Mena Saad, DO2, Jonathan Scott, MD3, Wichit Srikureja, MD4, Khalid Mumtaz, MBBS, MSc1. P0967 - The Bleeding Duodenal Varix Dilemma: An Atypical Endoscopic Presentation of Duodenal Variceal Bleed, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
