Sunday Poster Session
Category: IBD
P1051 - Breaking Down Barriers: Comparing Patient Challenges in Inflammatory Bowel Disease Care Across Healthcare Settings
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall

Aaron Tabibzadeh, MD
New York University Langone Health
New York, NY
Presenting Author(s)
Aaron Tabibzadeh, MD1, Sharon Klein, MD1, Shaili Babbar, MD, MBA1, Juan Cerezo, MD1, Antoinette Schoenthaler, PhD2, Lisa Malter, MD, FACG3, Jordan Axelrad, MD, MPH4
1New York University Langone Health, New York, NY; 2Department of Population Health, NYU Langone Health, New York, NY; 3Division of Gastroenterology, Department of Medicine, NYU Langone Health, New York, NY; 4Division of Gastroenterology, Department of Medicine, NYU Grossman School of Medicine, New York, NY
Introduction:
Inflammatory bowel disease (IBD) is a chronic condition resulting in substantial morbidity. Social determinants of health, including economic stability, education, and community resources, can create disparities in IBD outcomes. Our prior work identified disparities in IBD care between private and public hospital settings, driven in part by differences in patient demographics such as race and housing instability, as well as variation in advanced therapy use. This study aimed to identify barriers to chronic IBD care among patients treated at a private quaternary care hospital with a comprehensive IBD center versus an IBD center at large safety-net public hospital in New York City.
Methods:
We conducted qualitative focus groups of adult patients with Crohn’s disease or ulcerative colitis receiving care at a private or public hospital. Patients were contacted via MyChart, phone call, or in person after their appointments, and invited to join the study. Focus groups were conducted over WebEx using semi-structured interview guides. Interview notes were analyzed using a thematic coding approach with institutional ChatGPT-4, clustering findings into themes.
Results:
Ten focus groups were conducted with a total of 23 IBD patients (15 patients from the private hospital, 8 from the public hospital). Patients at both sites reported issues with: (1) insurance companies approving medications, (2) transportation logistics, (3) appointment wait times, and (4) difficulty contacting providers (Table). Patients also expressed concern about colonoscopies, specifically regarding the preparation and procedure. Patients at both sites described the mental and emotional toll of navigating insurance and payment assistance programs. Public hospital patients uniquely reported financial difficulties in maintaining nutritious diets and eliminating individual IBD symptom triggers. Private hospital patients reported frustration with medical record transfers between health systems and unclear billing processes.
Discussion:
This qualitative study using focus groups revealed shared and site-specific differences in patients’ experiences with IBD care. Both groups of patients emphasized the financial and logistical barriers to care, which often negatively impacted physical and mental health. Disparities in access to affordable foods and symptom trigger management in the safety-net patient population highlight the need for continued community and patient-centered interventions to help improve IBD care for these patients.
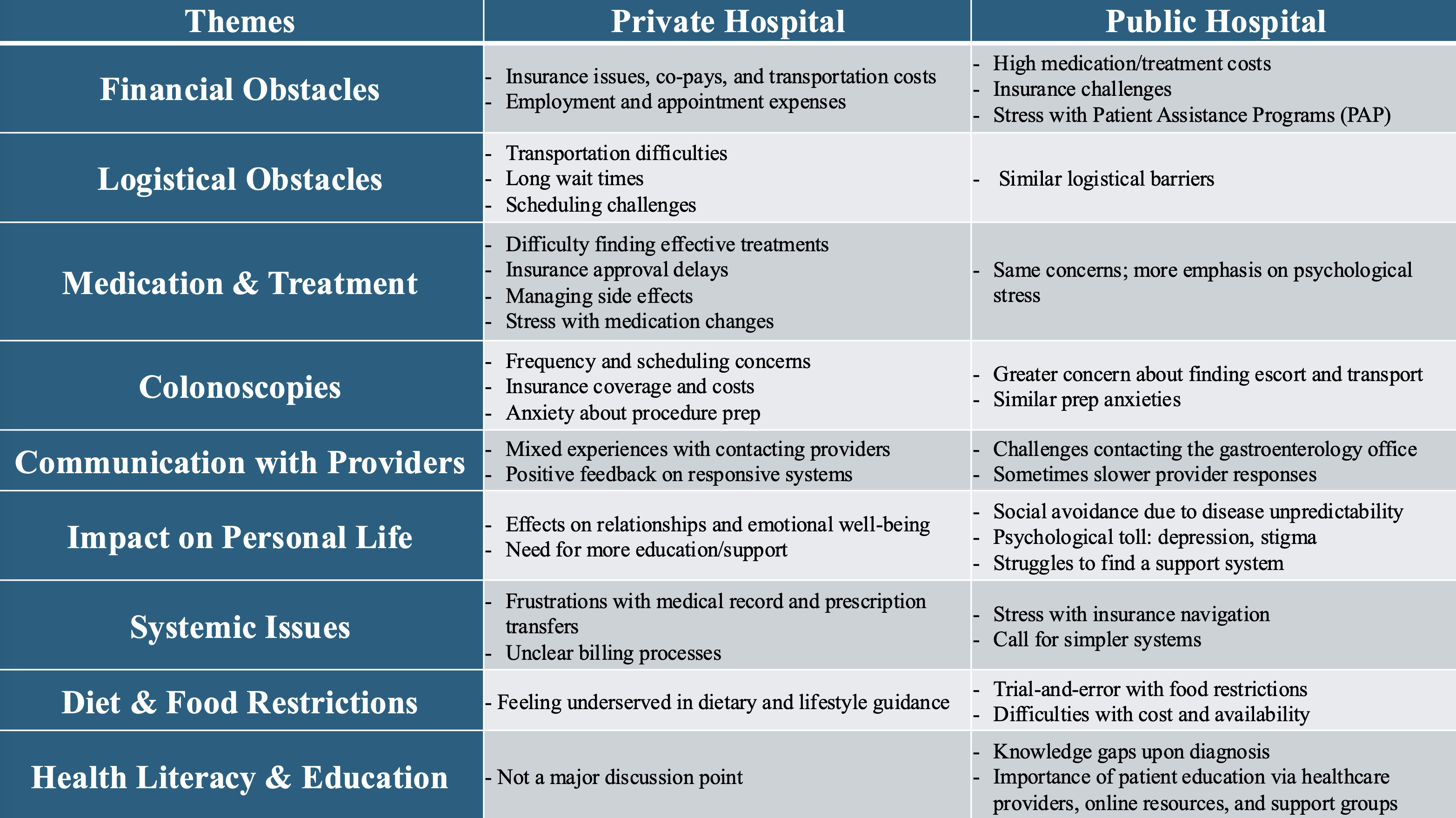
Figure: Table. Comparison of themes elucidated from private vs public hospital focus groups.
Disclosures:
Aaron Tabibzadeh indicated no relevant financial relationships.
Sharon Klein indicated no relevant financial relationships.
Shaili Babbar indicated no relevant financial relationships.
Juan Cerezo indicated no relevant financial relationships.
Antoinette Schoenthaler indicated no relevant financial relationships.
Lisa Malter: AbbVie – Grant/Research Support. Bristol Myers Squibb – Advisory Committee/Board Member. Celltrion – Advisory Committee/Board Member. Janssen – Grant/Research Support. Pfizer – Advisory Committee/Board Member, Consultant, Grant/Research Support. Pharmacosmos – Consultant.
Jordan Axelrad: Abbvie – Advisory Committee/Board Member, Consultant, Honorarium. Abivax – Advisory Committee/Board Member, Consultant, Honorarium. Adiso – Advisory Committee/Board Member, Consultant, Honorarium. BioFire Diagnostics – Grant/Research Support. Biomerieux – Advisory Committee/Board Member, Consultant, Honorarium. Bristol-Myers Squibb – Advisory Committee/Board Member, Consultant, Honorarium. Celltrion – Advisory Committee/Board Member, Consultant, Honorarium. Ferring – Advisory Committee/Board Member, Consultant, Honorarium. Fresenius – Advisory Committee/Board Member, Consultant, Honorarium. Genentech – Grant/Research Support. Janssen – Advisory Committee/Board Member, Consultant. Janssen – Grant/Research Support. Janssen – Honorarium. Johnson & Johnson – Advisory Committee/Board Member, Consultant. Merck – Advisory Committee/Board Member, Consultant, Honorarium. NIH NIDDK Diseases K23DK124570 – Grant/Research Support. Pfizer – Advisory Committee/Board Member, Consultant, Honorarium. Sanofi – Advisory Committee/Board Member, Consultant, Honorarium. The Crohn's and Colitis Foundation (#878246) – Grant/Research Support. The Judith & Stewart Colton Center for Autoimmunity – Grant/Research Support. Vedanta – Advisory Committee/Board Member, Consultant, Honorarium.
Aaron Tabibzadeh, MD1, Sharon Klein, MD1, Shaili Babbar, MD, MBA1, Juan Cerezo, MD1, Antoinette Schoenthaler, PhD2, Lisa Malter, MD, FACG3, Jordan Axelrad, MD, MPH4. P1051 - Breaking Down Barriers: Comparing Patient Challenges in Inflammatory Bowel Disease Care Across Healthcare Settings, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1New York University Langone Health, New York, NY; 2Department of Population Health, NYU Langone Health, New York, NY; 3Division of Gastroenterology, Department of Medicine, NYU Langone Health, New York, NY; 4Division of Gastroenterology, Department of Medicine, NYU Grossman School of Medicine, New York, NY
Introduction:
Inflammatory bowel disease (IBD) is a chronic condition resulting in substantial morbidity. Social determinants of health, including economic stability, education, and community resources, can create disparities in IBD outcomes. Our prior work identified disparities in IBD care between private and public hospital settings, driven in part by differences in patient demographics such as race and housing instability, as well as variation in advanced therapy use. This study aimed to identify barriers to chronic IBD care among patients treated at a private quaternary care hospital with a comprehensive IBD center versus an IBD center at large safety-net public hospital in New York City.
Methods:
We conducted qualitative focus groups of adult patients with Crohn’s disease or ulcerative colitis receiving care at a private or public hospital. Patients were contacted via MyChart, phone call, or in person after their appointments, and invited to join the study. Focus groups were conducted over WebEx using semi-structured interview guides. Interview notes were analyzed using a thematic coding approach with institutional ChatGPT-4, clustering findings into themes.
Results:
Ten focus groups were conducted with a total of 23 IBD patients (15 patients from the private hospital, 8 from the public hospital). Patients at both sites reported issues with: (1) insurance companies approving medications, (2) transportation logistics, (3) appointment wait times, and (4) difficulty contacting providers (Table). Patients also expressed concern about colonoscopies, specifically regarding the preparation and procedure. Patients at both sites described the mental and emotional toll of navigating insurance and payment assistance programs. Public hospital patients uniquely reported financial difficulties in maintaining nutritious diets and eliminating individual IBD symptom triggers. Private hospital patients reported frustration with medical record transfers between health systems and unclear billing processes.
Discussion:
This qualitative study using focus groups revealed shared and site-specific differences in patients’ experiences with IBD care. Both groups of patients emphasized the financial and logistical barriers to care, which often negatively impacted physical and mental health. Disparities in access to affordable foods and symptom trigger management in the safety-net patient population highlight the need for continued community and patient-centered interventions to help improve IBD care for these patients.
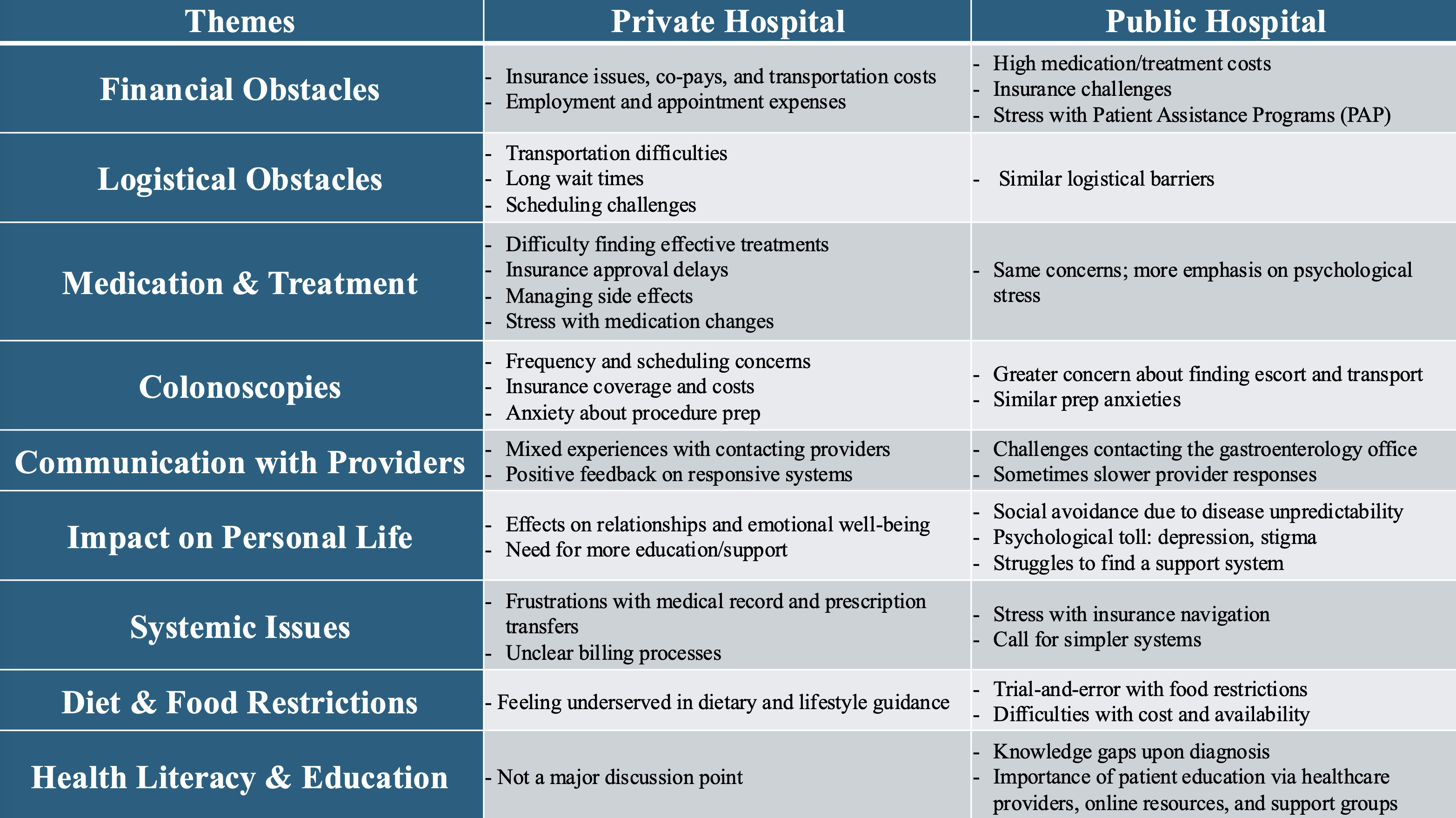
Figure: Table. Comparison of themes elucidated from private vs public hospital focus groups.
Disclosures:
Aaron Tabibzadeh indicated no relevant financial relationships.
Sharon Klein indicated no relevant financial relationships.
Shaili Babbar indicated no relevant financial relationships.
Juan Cerezo indicated no relevant financial relationships.
Antoinette Schoenthaler indicated no relevant financial relationships.
Lisa Malter: AbbVie – Grant/Research Support. Bristol Myers Squibb – Advisory Committee/Board Member. Celltrion – Advisory Committee/Board Member. Janssen – Grant/Research Support. Pfizer – Advisory Committee/Board Member, Consultant, Grant/Research Support. Pharmacosmos – Consultant.
Jordan Axelrad: Abbvie – Advisory Committee/Board Member, Consultant, Honorarium. Abivax – Advisory Committee/Board Member, Consultant, Honorarium. Adiso – Advisory Committee/Board Member, Consultant, Honorarium. BioFire Diagnostics – Grant/Research Support. Biomerieux – Advisory Committee/Board Member, Consultant, Honorarium. Bristol-Myers Squibb – Advisory Committee/Board Member, Consultant, Honorarium. Celltrion – Advisory Committee/Board Member, Consultant, Honorarium. Ferring – Advisory Committee/Board Member, Consultant, Honorarium. Fresenius – Advisory Committee/Board Member, Consultant, Honorarium. Genentech – Grant/Research Support. Janssen – Advisory Committee/Board Member, Consultant. Janssen – Grant/Research Support. Janssen – Honorarium. Johnson & Johnson – Advisory Committee/Board Member, Consultant. Merck – Advisory Committee/Board Member, Consultant, Honorarium. NIH NIDDK Diseases K23DK124570 – Grant/Research Support. Pfizer – Advisory Committee/Board Member, Consultant, Honorarium. Sanofi – Advisory Committee/Board Member, Consultant, Honorarium. The Crohn's and Colitis Foundation (#878246) – Grant/Research Support. The Judith & Stewart Colton Center for Autoimmunity – Grant/Research Support. Vedanta – Advisory Committee/Board Member, Consultant, Honorarium.
Aaron Tabibzadeh, MD1, Sharon Klein, MD1, Shaili Babbar, MD, MBA1, Juan Cerezo, MD1, Antoinette Schoenthaler, PhD2, Lisa Malter, MD, FACG3, Jordan Axelrad, MD, MPH4. P1051 - Breaking Down Barriers: Comparing Patient Challenges in Inflammatory Bowel Disease Care Across Healthcare Settings, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
