Sunday Poster Session
Category: IBD
P1103 - Severe Fibrosis Predicted by Shear Wave Elastography of Crohn’s-Related Ileal Strictures Is Associated With Resistance to Medical Therapy
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall

Noa Krugliak Cleveland, MD (she/her/hers)
University of Chicago
Chicago, IL
Presenting Author(s)
Noa Krugliak Cleveland, MD1, Khushi S. Bhondwe, BS2, Charlotte M. Duty, BA2, Asher Shafrir, MD3, David T. Rubin, MD4
1University of Chicago, Chicago, IL; 2University of Chicago Medicine, Chicago, IL; 3University of Chicago Medicine, Inflammatory Bowel Disease Center, Chicago, IL; 4University of Chicago Medicine Inflammatory Bowel Disease Center, Chicago, IL, USA, Chicago, IL
Introduction: Patients (pts) with fibrostenotic Crohn’s disease (CD) are clinically challenging when trying to predict response to medical therapy. Shear wave elastography (SWE) is a feature of intestinal ultrasound (IUS) which detects intestinal fibrosis and has been proposed as a prediction tool for non-response to medical therapy. We assessed the clinical outcomes of pts with CD who have ileal strictures and SWE findings of severe fibrosis.
Methods: We reviewed index IUS exams of adult pts with CD from 10/5/2021-3/31/2025 and included those with a confirmed diagnosis of CD, findings of an ileal stricture on IUS (defined as bowel wall thickness (BWT) >3.0 mm, luminal narrowing, and with or without proximal dilation (Lu C. GUT. 2024)) and SWE Median (SWEM) values consistent with severe fibrosis (defined as >16.7 kPa (Chen Y. IBDJ. 2018)). Primary analysis was poor disease outcome defined as IBD medication change/escalation, prescription of corticosteroids, IBD-related hospitalization, and CD-related surgery. Steroid-free clinical remission (SFCR) was defined as HBI< 5 and no prescription of corticosteroids for IBD-related symptoms for ≥6 months. Resolution of stricture on follow-up IUS was defined as normalization of BWT, luminal narrowing, and proximal dilation.
Results: We included 35 pts (Table 1). Median values for stricture length was 10.0 cm (IQR 5.9-13.3) and maximal BWT was 4.95 (IQR 4-6.8) (Table 1). 28 (80%) had evidence of inflammation characterized by at least one parameter (hyperemia, loss of stratification, mesenteric fat proliferation). No significant correlation was found between IUS parameters and SWE on univariate analysis (Table 1).
22 pts (63%) had at least one follow up IUS exam over a median of 400 days (IQR 269-603). 30 (86%) had poor disease outcomes (21 (60%) therapy change/escalation, 22 (63%) course of steroids, 4 (11%) IBD-related hospitalization, 15 (43%) surgery). Of those who did not undergo surgery, 7 (35%) had resolution of stricture. A two-tailed Fisher’s exact test revealed that pts who underwent surgery were less likely to require therapy change/escalation (2 (13.3%) vs 14 (70%), p=0.0016) or have an increase from index IUS HBI score (1 (6.7%) vs 10 (50%), p=0.0095), and more likely to achieve SFCR (12 (80%) vs 9 (45%), p=0.0461) (Table 2).
Discussion: Elevated SWEM measures of >16.7 kPa on IUS is associated with medically refractory ileal CD, despite findings of inflammation by other IUS parameters. These findings should inform medical and surgical decisions in CD.
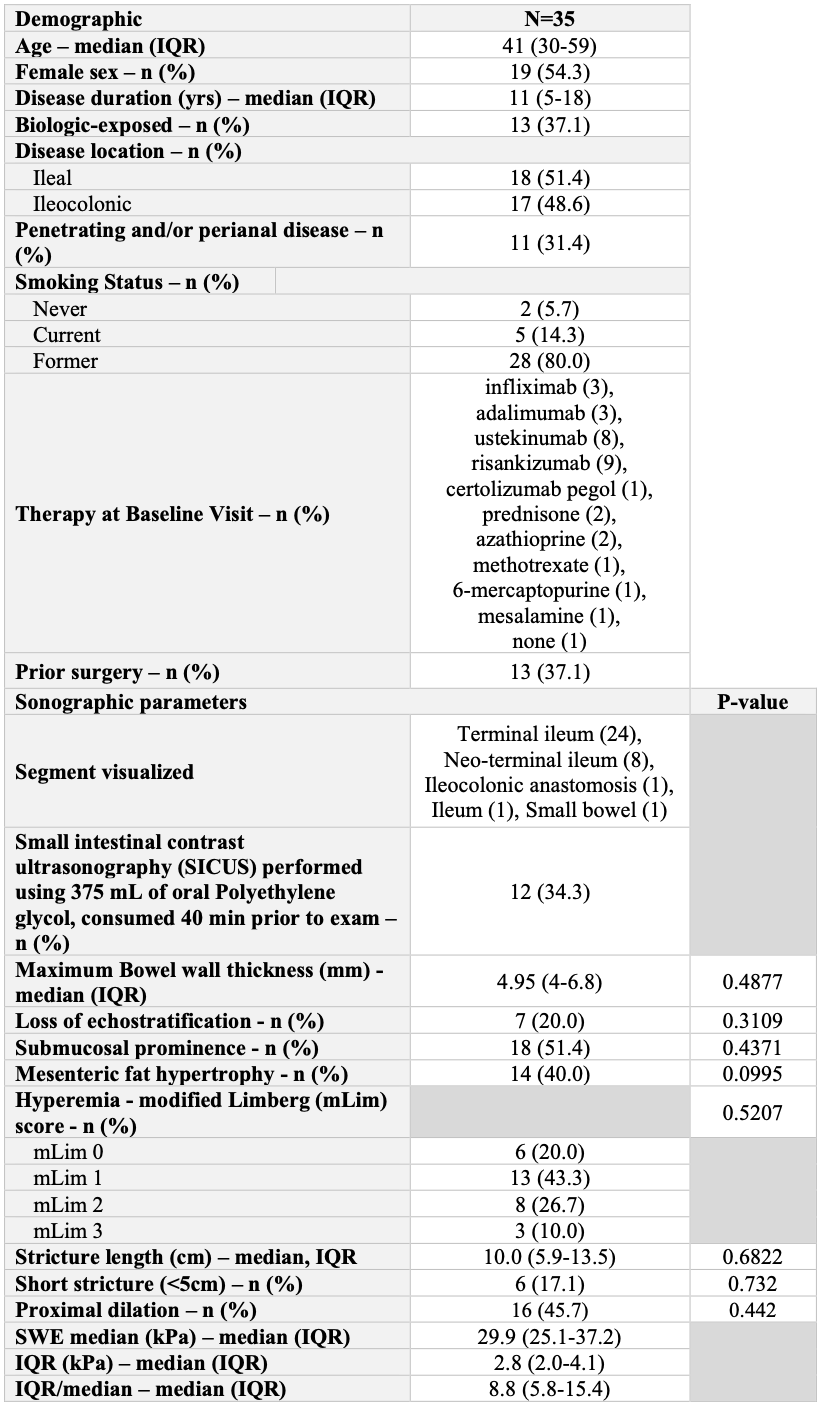
Figure: Table 1. Patient Demographics and Baseline Ultrasound Parameters
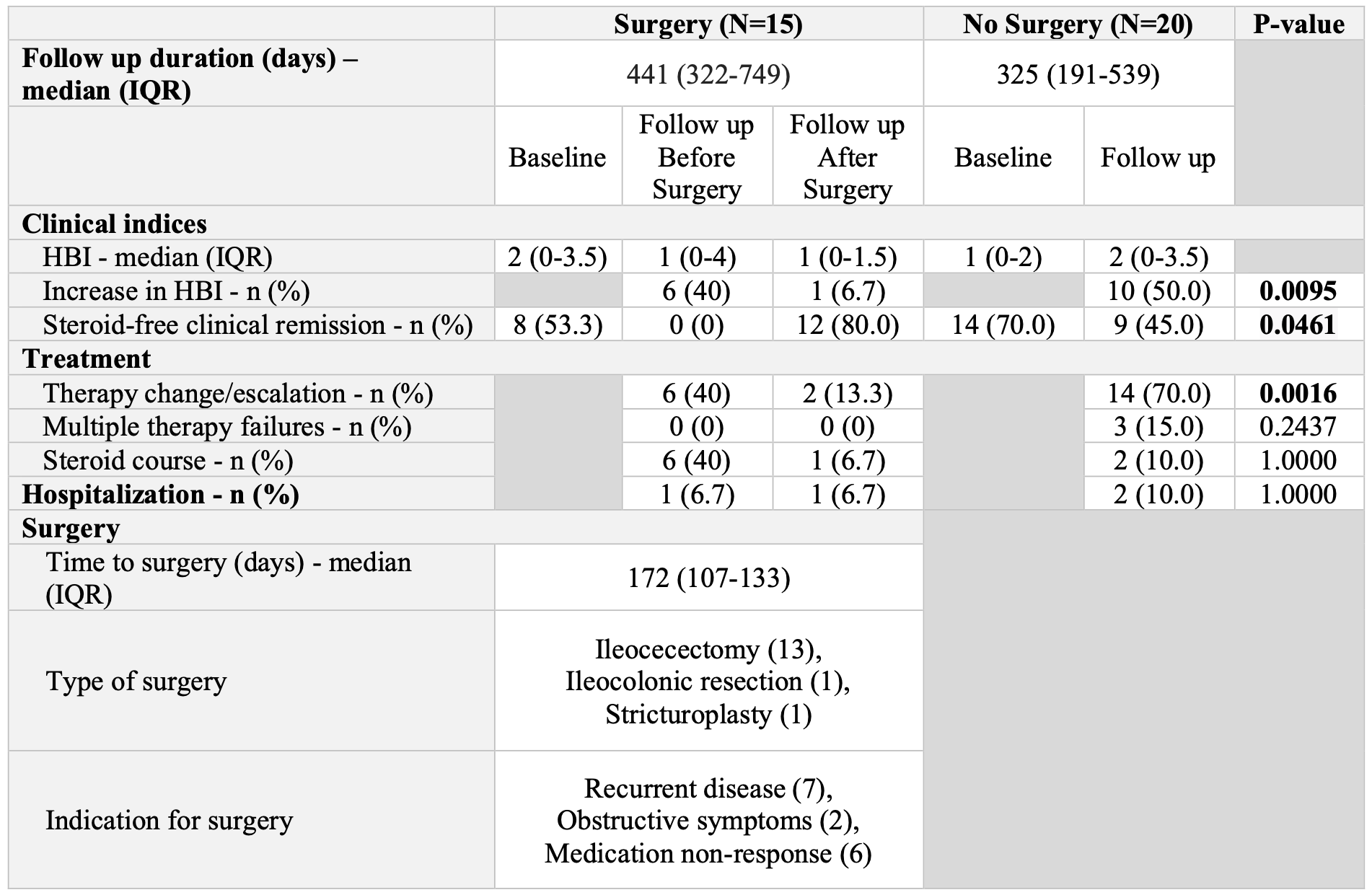
Figure: Table 2. Disease Progression and Outcomes
Disclosures:
Noa Krugliak Cleveland: Johnson & Johnson – Consultant. NueroLogica – Consultant.
Khushi Bhondwe indicated no relevant financial relationships.
Charlotte Duty indicated no relevant financial relationships.
Asher Shafrir indicated no relevant financial relationships.
David Rubin: AbbVie – Advisory Committee/Board Member, Consultant, Speaker fees. Abivax SA – Consultant. Altrubio – Advisory Committee/Board Member, Consultant, Speaker feees, Stock Options. Avalo – Advisory Committee/Board Member, Consultant, Speaker fees. Bausch Health – Consultant. Bristol Myers Squibb – Advisory Committee/Board Member, Consultant, Speaker fees. Buhlmann Diagnostics – Advisory Committee/Board Member, Consultant, Speaker fees. Celltrion – Consultant. ClostraBio – Consultant. Connect BioPharma – Consultant. Cornerstones Health, Inc – Board of Directors membership. Douglas Pharmaceuticals – Consultant. Eli Lilly & Co. – Consultant. Foresee, Genentech (Roche) Inc. – Consultant. Image Analysis Group – Consultant. InDex Pharmaceutical – Consultant. Intouch Group – Advisory Committee/Board Member, Consultant, Speaker fees. Iterative Health – Advisory Committee/Board Member, Consultant, Speaker fees. Iterative Health – Stock Options. Janssen Pharmaceuticals – Consultant. Lilly – Advisory Committee/Board Member, Consultant, Speaker fees. Odyssey Therapeutics – Consultant. Pfizer – Advisory Committee/Board Member, Consultant, Speaker fees. Sanofi – Consultant. Takeda – Advisory Committee/Board Member, Consultant, Grant/Research Support, Speaker fees. Throne – Consultant. Vedanta – Consultant.
Noa Krugliak Cleveland, MD1, Khushi S. Bhondwe, BS2, Charlotte M. Duty, BA2, Asher Shafrir, MD3, David T. Rubin, MD4. P1103 - Severe Fibrosis Predicted by Shear Wave Elastography of Crohn’s-Related Ileal Strictures Is Associated With Resistance to Medical Therapy, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1University of Chicago, Chicago, IL; 2University of Chicago Medicine, Chicago, IL; 3University of Chicago Medicine, Inflammatory Bowel Disease Center, Chicago, IL; 4University of Chicago Medicine Inflammatory Bowel Disease Center, Chicago, IL, USA, Chicago, IL
Introduction: Patients (pts) with fibrostenotic Crohn’s disease (CD) are clinically challenging when trying to predict response to medical therapy. Shear wave elastography (SWE) is a feature of intestinal ultrasound (IUS) which detects intestinal fibrosis and has been proposed as a prediction tool for non-response to medical therapy. We assessed the clinical outcomes of pts with CD who have ileal strictures and SWE findings of severe fibrosis.
Methods: We reviewed index IUS exams of adult pts with CD from 10/5/2021-3/31/2025 and included those with a confirmed diagnosis of CD, findings of an ileal stricture on IUS (defined as bowel wall thickness (BWT) >3.0 mm, luminal narrowing, and with or without proximal dilation (Lu C. GUT. 2024)) and SWE Median (SWEM) values consistent with severe fibrosis (defined as >16.7 kPa (Chen Y. IBDJ. 2018)). Primary analysis was poor disease outcome defined as IBD medication change/escalation, prescription of corticosteroids, IBD-related hospitalization, and CD-related surgery. Steroid-free clinical remission (SFCR) was defined as HBI< 5 and no prescription of corticosteroids for IBD-related symptoms for ≥6 months. Resolution of stricture on follow-up IUS was defined as normalization of BWT, luminal narrowing, and proximal dilation.
Results: We included 35 pts (Table 1). Median values for stricture length was 10.0 cm (IQR 5.9-13.3) and maximal BWT was 4.95 (IQR 4-6.8) (Table 1). 28 (80%) had evidence of inflammation characterized by at least one parameter (hyperemia, loss of stratification, mesenteric fat proliferation). No significant correlation was found between IUS parameters and SWE on univariate analysis (Table 1).
22 pts (63%) had at least one follow up IUS exam over a median of 400 days (IQR 269-603). 30 (86%) had poor disease outcomes (21 (60%) therapy change/escalation, 22 (63%) course of steroids, 4 (11%) IBD-related hospitalization, 15 (43%) surgery). Of those who did not undergo surgery, 7 (35%) had resolution of stricture. A two-tailed Fisher’s exact test revealed that pts who underwent surgery were less likely to require therapy change/escalation (2 (13.3%) vs 14 (70%), p=0.0016) or have an increase from index IUS HBI score (1 (6.7%) vs 10 (50%), p=0.0095), and more likely to achieve SFCR (12 (80%) vs 9 (45%), p=0.0461) (Table 2).
Discussion: Elevated SWEM measures of >16.7 kPa on IUS is associated with medically refractory ileal CD, despite findings of inflammation by other IUS parameters. These findings should inform medical and surgical decisions in CD.
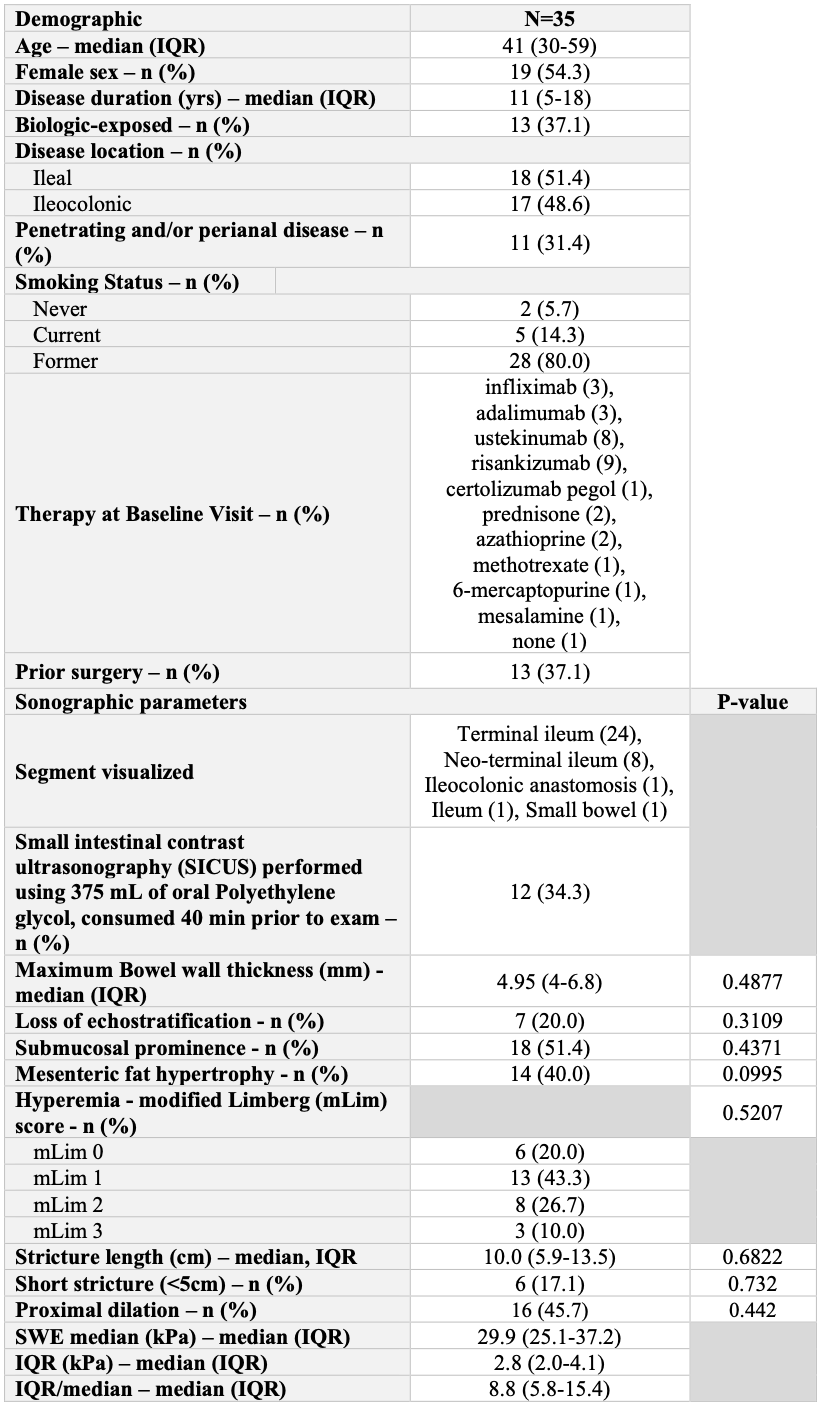
Figure: Table 1. Patient Demographics and Baseline Ultrasound Parameters
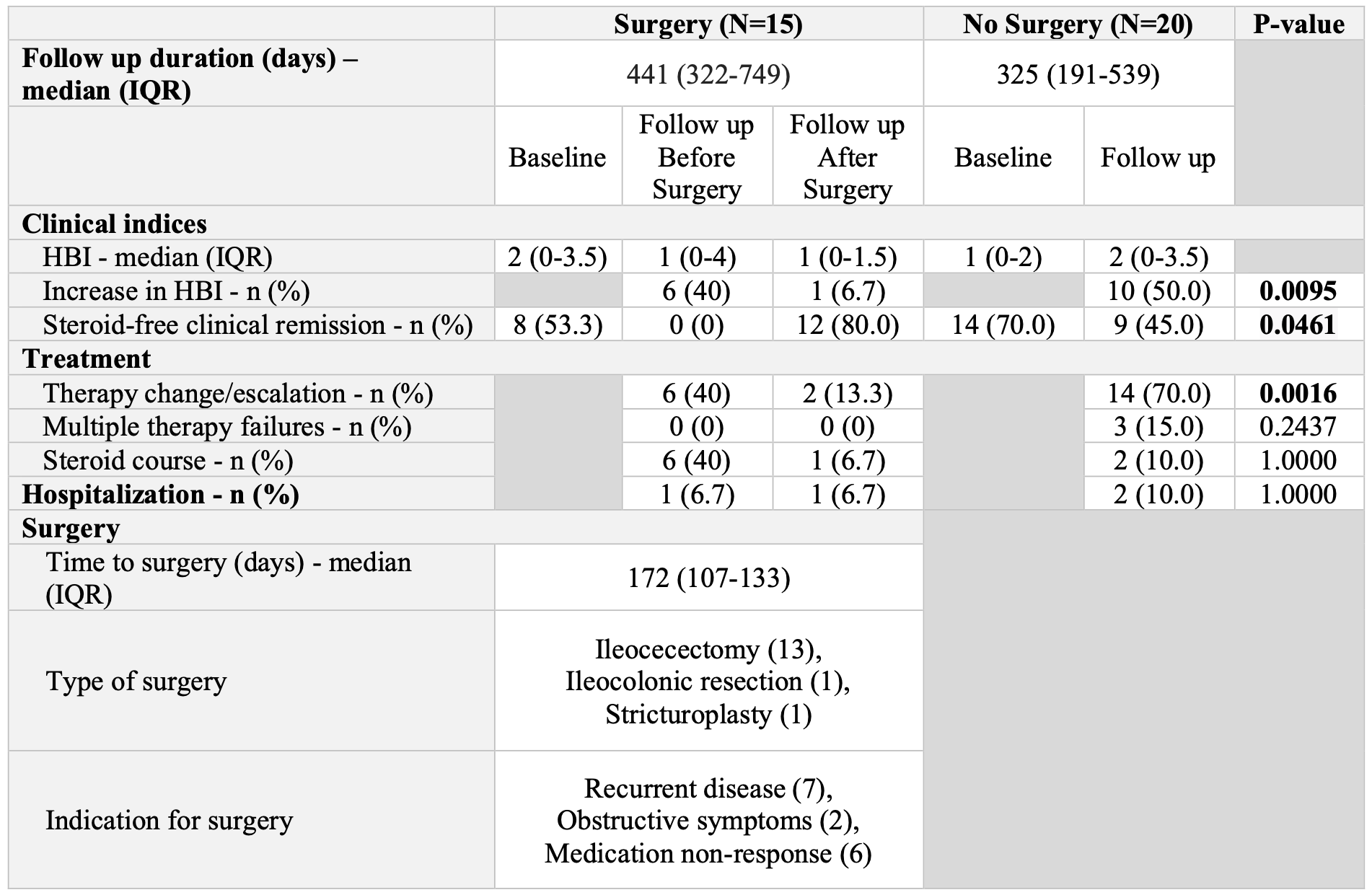
Figure: Table 2. Disease Progression and Outcomes
Disclosures:
Noa Krugliak Cleveland: Johnson & Johnson – Consultant. NueroLogica – Consultant.
Khushi Bhondwe indicated no relevant financial relationships.
Charlotte Duty indicated no relevant financial relationships.
Asher Shafrir indicated no relevant financial relationships.
David Rubin: AbbVie – Advisory Committee/Board Member, Consultant, Speaker fees. Abivax SA – Consultant. Altrubio – Advisory Committee/Board Member, Consultant, Speaker feees, Stock Options. Avalo – Advisory Committee/Board Member, Consultant, Speaker fees. Bausch Health – Consultant. Bristol Myers Squibb – Advisory Committee/Board Member, Consultant, Speaker fees. Buhlmann Diagnostics – Advisory Committee/Board Member, Consultant, Speaker fees. Celltrion – Consultant. ClostraBio – Consultant. Connect BioPharma – Consultant. Cornerstones Health, Inc – Board of Directors membership. Douglas Pharmaceuticals – Consultant. Eli Lilly & Co. – Consultant. Foresee, Genentech (Roche) Inc. – Consultant. Image Analysis Group – Consultant. InDex Pharmaceutical – Consultant. Intouch Group – Advisory Committee/Board Member, Consultant, Speaker fees. Iterative Health – Advisory Committee/Board Member, Consultant, Speaker fees. Iterative Health – Stock Options. Janssen Pharmaceuticals – Consultant. Lilly – Advisory Committee/Board Member, Consultant, Speaker fees. Odyssey Therapeutics – Consultant. Pfizer – Advisory Committee/Board Member, Consultant, Speaker fees. Sanofi – Consultant. Takeda – Advisory Committee/Board Member, Consultant, Grant/Research Support, Speaker fees. Throne – Consultant. Vedanta – Consultant.
Noa Krugliak Cleveland, MD1, Khushi S. Bhondwe, BS2, Charlotte M. Duty, BA2, Asher Shafrir, MD3, David T. Rubin, MD4. P1103 - Severe Fibrosis Predicted by Shear Wave Elastography of Crohn’s-Related Ileal Strictures Is Associated With Resistance to Medical Therapy, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
