Sunday Poster Session
Category: IBD
P1090 - Bridging the Gap: Hospitalized IBD Transition of Care Platform
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall

Ernesto Robalino Gonzaga, MD (he/him/his)
AdventHealth
Philadelphia, PA
Presenting Author(s)
Ernesto Robalino Gonzaga, MD1, Aimen Farooq, MD2, Abdul Mohammed, MD2, Asfand Khan, MS1, Jennifer Seminerio, MD2, Ilan Aharoni, MD2
1AdventHealth, Orlando, FL; 2Department of Gastroenterology and Hepatology, AdventHealth Orlando, Orlando, FL
Introduction: Hospitalized patients with IBD are at significant risk of rehospitalization with one significant factor is a lapse in continuity of care. Post-hospitalization follow-up in the outpatient GI clinic is a protective factor against early readmission among IBD patients. However, achieving timely follow-up remains challenging due to fragmented communication systems, scheduling delays, and insufficient coordination between inpatient and outpatient services. Our study examines the impact of a centralized communication platform (CCP) designed to improve the transition of care for hospitalized IBD patients.
Methods: We conducted a retrospective analysis of patients admitted for IBD-related illnesses at a tertiary care center between July 2023 and July 2024. Patients were stratified based on the use or non-use of CCP for coordinating outpatient care following hospitalization. Details regarding demographics, IBD characteristics, hospitalization metrics, and post-discharge outcomes were collected and analyzed. Outcomes included follow-up rates, time to follow-up, new therapy initiation rates, and 30-day readmission rates.
Results: Among 91 patients (median age 40, 53% male), 69% were Caucasian, 24% Latin American, and the median BMI was 24. Ulcerative colitis accounted for 32% of cases, predominantly pancolitis (22%), while Crohn’s disease comprised 68%, with ileocolonic disease being the most common phenotype (39%). Most patients (62%) had prior treatment, and 44% were on active therapy during hospitalization.
The CCP group showed a non-significant follow-up rate of 85% compared to 74% in the non-CCP group. The CCP group had a longer time to therapy initiation, with a median of 45 days (IQR: 25-62) compared to 26 days (IQR: 3-54) in the non-CCP group. This may be due to the higher rate of new therapy initiation in the CCP group (40% vs 32%), although it was not significant. The 30-day readmission (21% vs. 18%, p=0.72) and colectomy rates (4% vs. 5%, p=0.82) were similar in both groups.
Discussion: CCP was associated with improved follow-up rates and initiation of new therapies post-hospitalization for IBD patients. However, these findings were not statistically significant, likely due to the limited sample size. The existing EMR-based process, as the primary alternative to CCP, lacked transparency, with no clear understanding among stakeholders regarding its workflow or outcome. This inefficiency highlighted the need for CCP as a structured approach to improve care transitions.
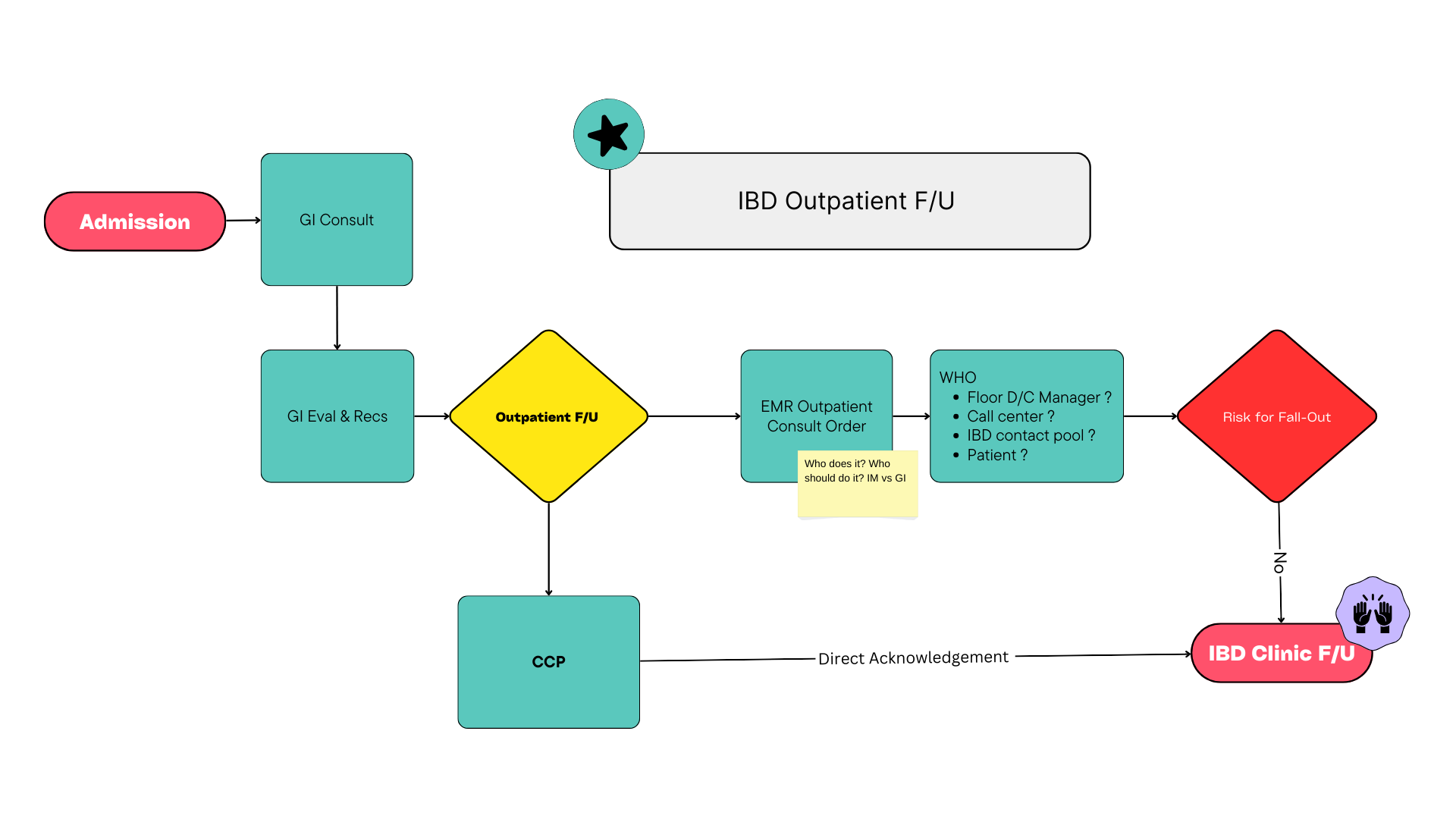
Figure: IBD Outpatient Follow-Up Workflow
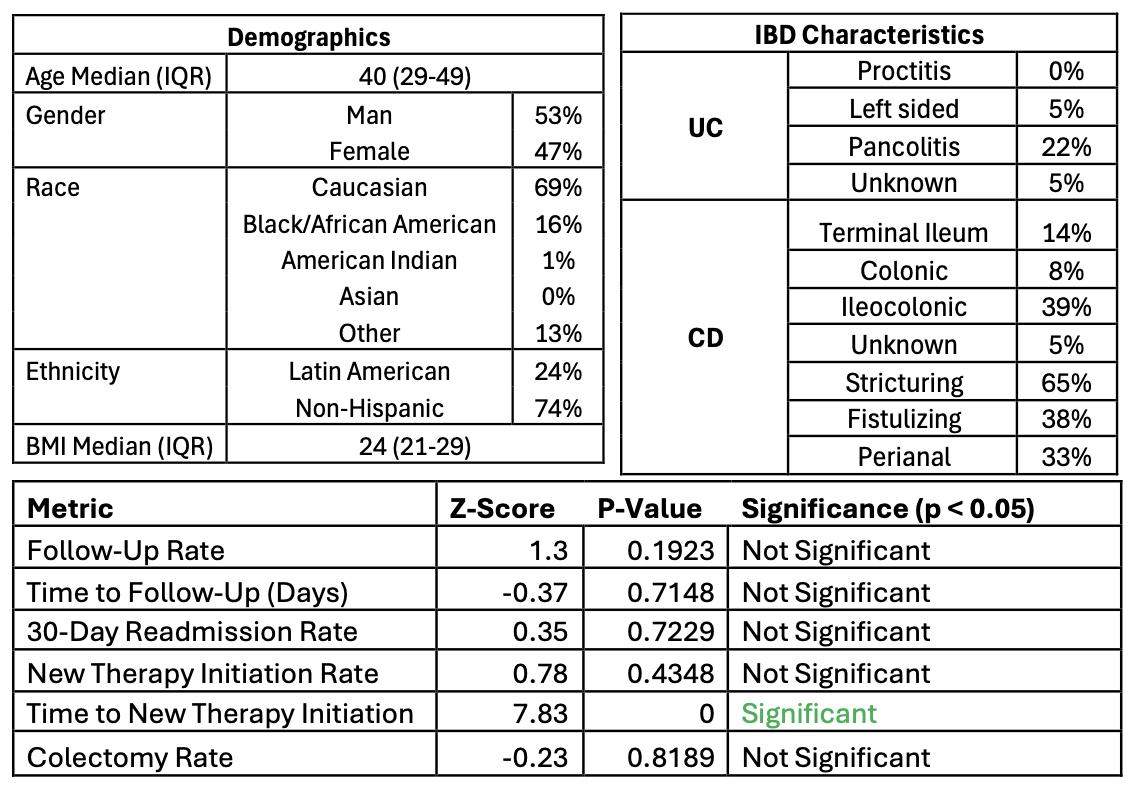
Figure: IBD Patient Characteristics
Disclosures:
Ernesto Robalino Gonzaga indicated no relevant financial relationships.
Aimen Farooq indicated no relevant financial relationships.
Abdul Mohammed indicated no relevant financial relationships.
Asfand Khan indicated no relevant financial relationships.
Jennifer Seminerio: Abbvie – Consultant. Johnson & Johnson – Consultant. Lilly – Consultant. Pfizer – Consultant. Sanofi – Consultant. Takeda – Consultant.
Ilan Aharoni indicated no relevant financial relationships.
Ernesto Robalino Gonzaga, MD1, Aimen Farooq, MD2, Abdul Mohammed, MD2, Asfand Khan, MS1, Jennifer Seminerio, MD2, Ilan Aharoni, MD2. P1090 - Bridging the Gap: Hospitalized IBD Transition of Care Platform, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1AdventHealth, Orlando, FL; 2Department of Gastroenterology and Hepatology, AdventHealth Orlando, Orlando, FL
Introduction: Hospitalized patients with IBD are at significant risk of rehospitalization with one significant factor is a lapse in continuity of care. Post-hospitalization follow-up in the outpatient GI clinic is a protective factor against early readmission among IBD patients. However, achieving timely follow-up remains challenging due to fragmented communication systems, scheduling delays, and insufficient coordination between inpatient and outpatient services. Our study examines the impact of a centralized communication platform (CCP) designed to improve the transition of care for hospitalized IBD patients.
Methods: We conducted a retrospective analysis of patients admitted for IBD-related illnesses at a tertiary care center between July 2023 and July 2024. Patients were stratified based on the use or non-use of CCP for coordinating outpatient care following hospitalization. Details regarding demographics, IBD characteristics, hospitalization metrics, and post-discharge outcomes were collected and analyzed. Outcomes included follow-up rates, time to follow-up, new therapy initiation rates, and 30-day readmission rates.
Results: Among 91 patients (median age 40, 53% male), 69% were Caucasian, 24% Latin American, and the median BMI was 24. Ulcerative colitis accounted for 32% of cases, predominantly pancolitis (22%), while Crohn’s disease comprised 68%, with ileocolonic disease being the most common phenotype (39%). Most patients (62%) had prior treatment, and 44% were on active therapy during hospitalization.
The CCP group showed a non-significant follow-up rate of 85% compared to 74% in the non-CCP group. The CCP group had a longer time to therapy initiation, with a median of 45 days (IQR: 25-62) compared to 26 days (IQR: 3-54) in the non-CCP group. This may be due to the higher rate of new therapy initiation in the CCP group (40% vs 32%), although it was not significant. The 30-day readmission (21% vs. 18%, p=0.72) and colectomy rates (4% vs. 5%, p=0.82) were similar in both groups.
Discussion: CCP was associated with improved follow-up rates and initiation of new therapies post-hospitalization for IBD patients. However, these findings were not statistically significant, likely due to the limited sample size. The existing EMR-based process, as the primary alternative to CCP, lacked transparency, with no clear understanding among stakeholders regarding its workflow or outcome. This inefficiency highlighted the need for CCP as a structured approach to improve care transitions.
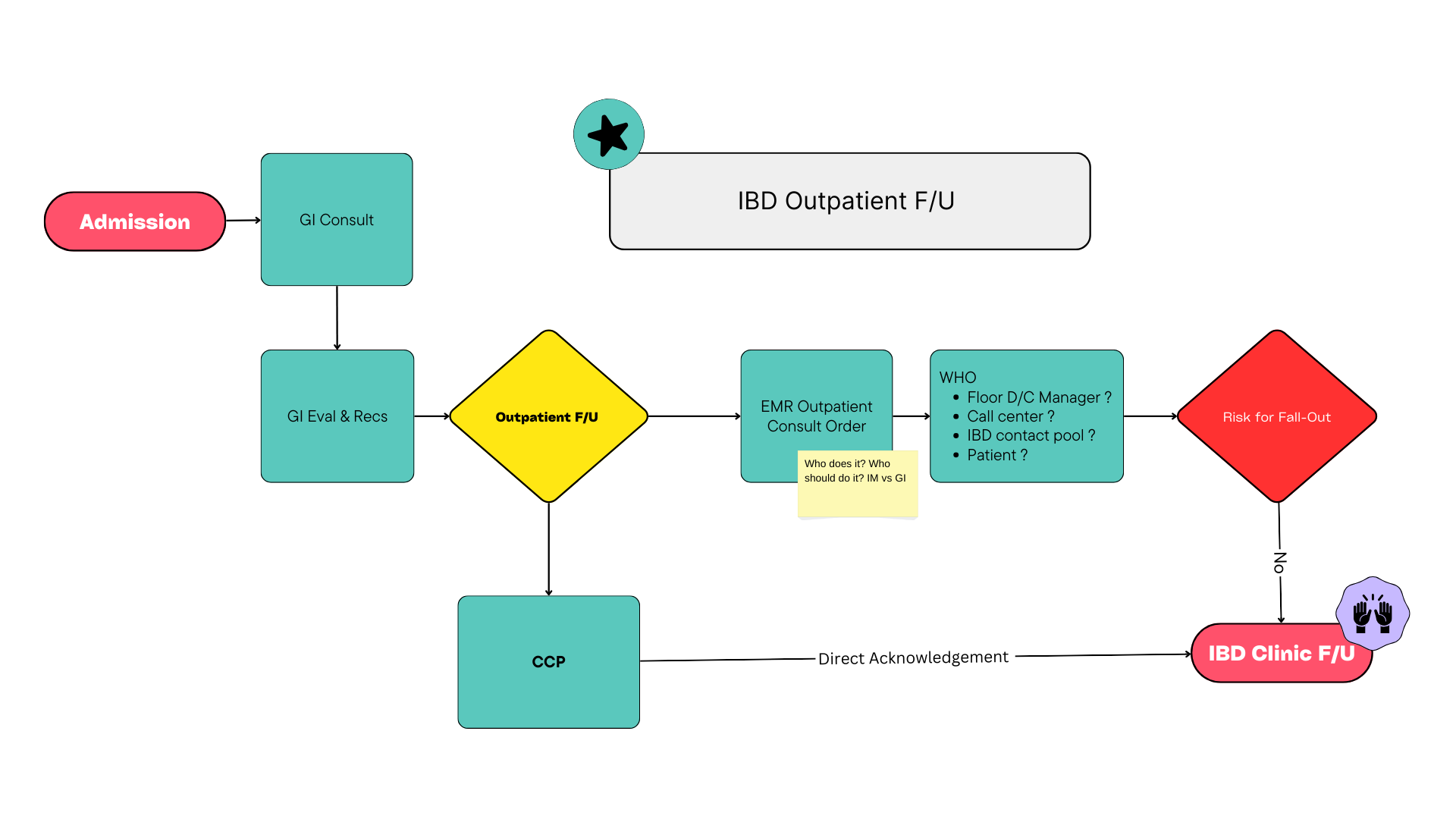
Figure: IBD Outpatient Follow-Up Workflow
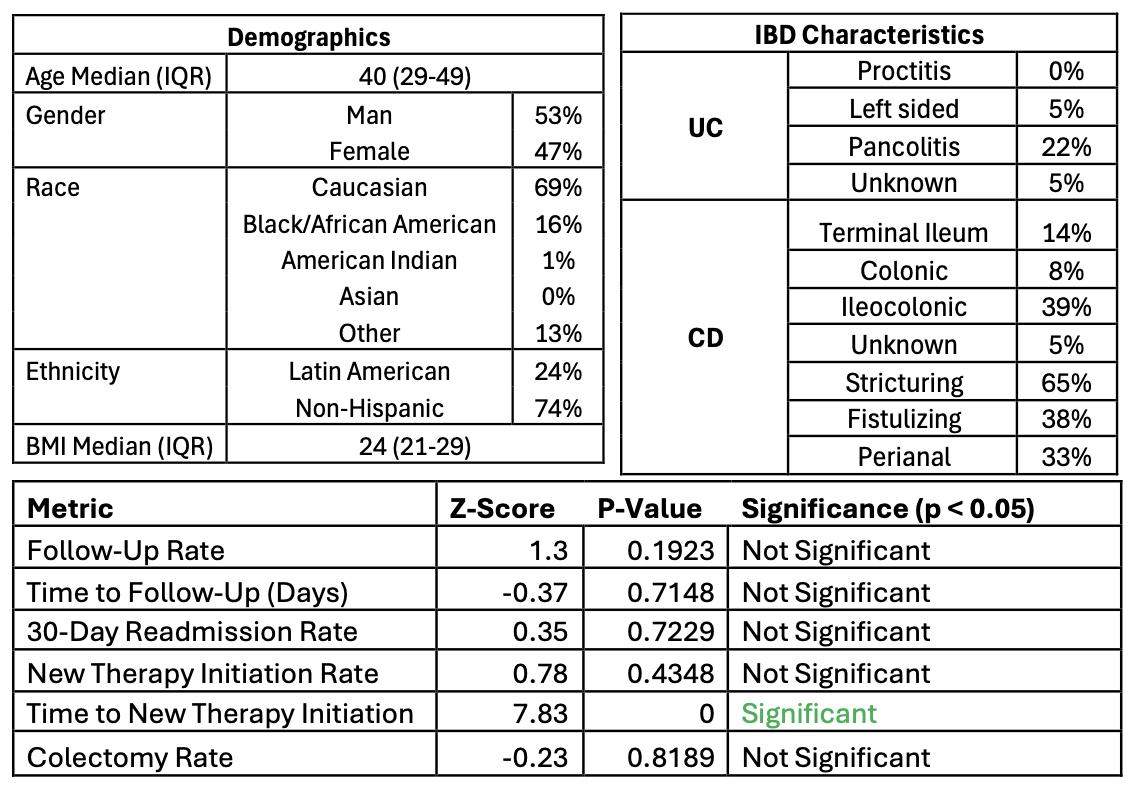
Figure: IBD Patient Characteristics
Disclosures:
Ernesto Robalino Gonzaga indicated no relevant financial relationships.
Aimen Farooq indicated no relevant financial relationships.
Abdul Mohammed indicated no relevant financial relationships.
Asfand Khan indicated no relevant financial relationships.
Jennifer Seminerio: Abbvie – Consultant. Johnson & Johnson – Consultant. Lilly – Consultant. Pfizer – Consultant. Sanofi – Consultant. Takeda – Consultant.
Ilan Aharoni indicated no relevant financial relationships.
Ernesto Robalino Gonzaga, MD1, Aimen Farooq, MD2, Abdul Mohammed, MD2, Asfand Khan, MS1, Jennifer Seminerio, MD2, Ilan Aharoni, MD2. P1090 - Bridging the Gap: Hospitalized IBD Transition of Care Platform, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
