Sunday Poster Session
Category: IBD
P1086 - Impact of IBD-Related Surgery on Dietary Practices and Perceptions in Patients With IBD
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall
- SW
Shawna E. Walsh, MD
Massachusetts General Hospital, Harvard Medical School
Boston, MA
Presenting Author(s)
Shawna E. Walsh, MD1, Seerat Chawla, BS, MSc2, Rachel Zhang, BS3, Kevin Casey, MPH1, Ashwin Ananthakrishnan, 4, Bharati Kochar, MD3, Emily Lopes, MD, MPH3
1Massachusetts General Hospital, Harvard Medical School, Boston, MA; 2Harvard Medical School, Boston, MA; 3Massachusetts General Hospital, Boston, MA; 4Division of Gastroenterology, Massachusetts General Hospital and Harvard Medical School, Boston, MA
Introduction: Evidence-based dietary recommendations for patients who have undergone surgery for IBD, such as diets for preventing recurrence or restrictions because of surgery, are limited. We aimed to compare dietary practices in those with and without a history of IBD-related surgery.
Methods: We administered a de-identified survey to IBD patients ≥18 years. We gathered demographics, medical and surgical history, dietary practices, and perceptions of dietary guidance. Participants self-confirmed diagnoses of Crohn’s disease (CD), ulcerative colitis (UC), or IBD-unclassified. The primary outcome was dietary modification due to IBD. Secondary outcomes included impact of IBD on appetite and enjoyment in eating, perception of diet as a trigger for flares, dietary supplement use, and comfort discussing diet with an IBD doctor. We used logistic regression to determine odds ratios (OR) and 95% CI for each outcome according to history of IBD-related surgery while adjusting for covariates.
Results: 648 respondents completed the survey (IBD-related surgery: yes=187, no=461). Those with a history of IBD-related surgery were younger at diagnosis (mean age 25 vs 33 years) and more likely to have CD (76.6 vs 42.2%); demographics were otherwise similar. Participants with IBD-related surgery were more likely to have modified their diet (aOR 1.78 (95%CI 1.03-3.06, p=0.04) when compared to those without surgery (Figure 1). In a subgroup analysis, those with a history of ileal pouch (n=42) were more likely to have modified their diet (aOR 4.08 (1.19-13.99), p=0.03) than those without, while those with a history of ostomy (n=28) were not (aOR 0.75 (0.28-1.98), p=0.56). Those with IBD-related surgery were also more likely to have appetite or enjoyment in eating affected by IBD, though this was not statistically significant (Table 1; p=0.06). More than 90% of respondents felt comfortable discussing diet with their IBD doctor, but less than 30% felt they received the “right amount” of dietary advice for their IBD.
Discussion: Patients with a history of IBD surgery, especially ileal pouches, were more likely to modify their diet and have appetite and enjoyment in eating impacted by their IBD. Though nearly all patients were comfortable discussing diet with their doctor, few felt they received adequate dietary guidance. Future studies and guidelines should better define dietary recommendations for those with IBD-related surgery, particularly ileal pouches.
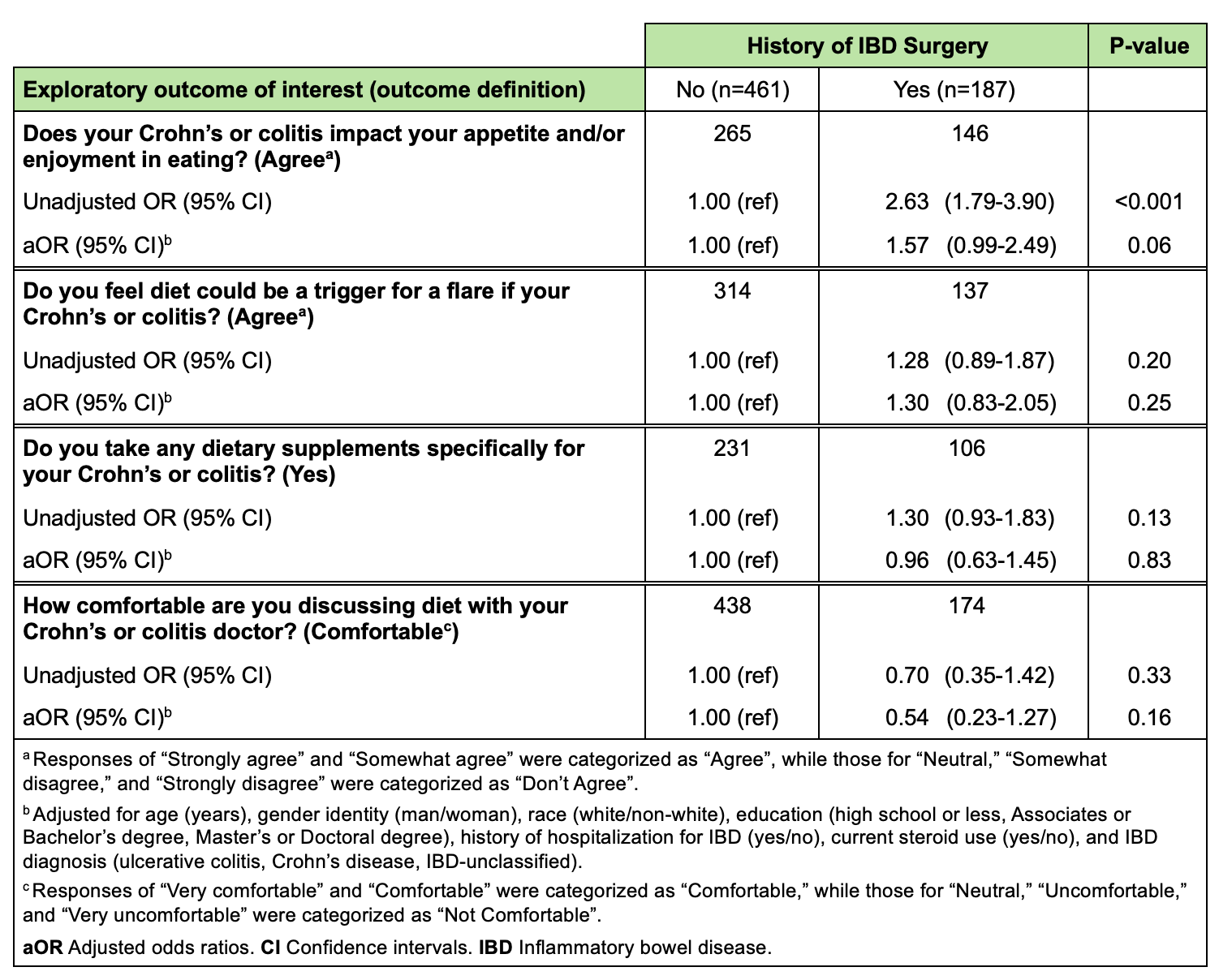
Figure: Figure 1. Adjusted odds ratios for having modified diet (primary outcome) according to history of IBD surgery (exposure of interest) and additional covariates. aOR Adjusted odds ratios. CI Confidence intervals. IBD Inflammatory bowel disease. IBD-U Inflammatory bowel disease unclassified.
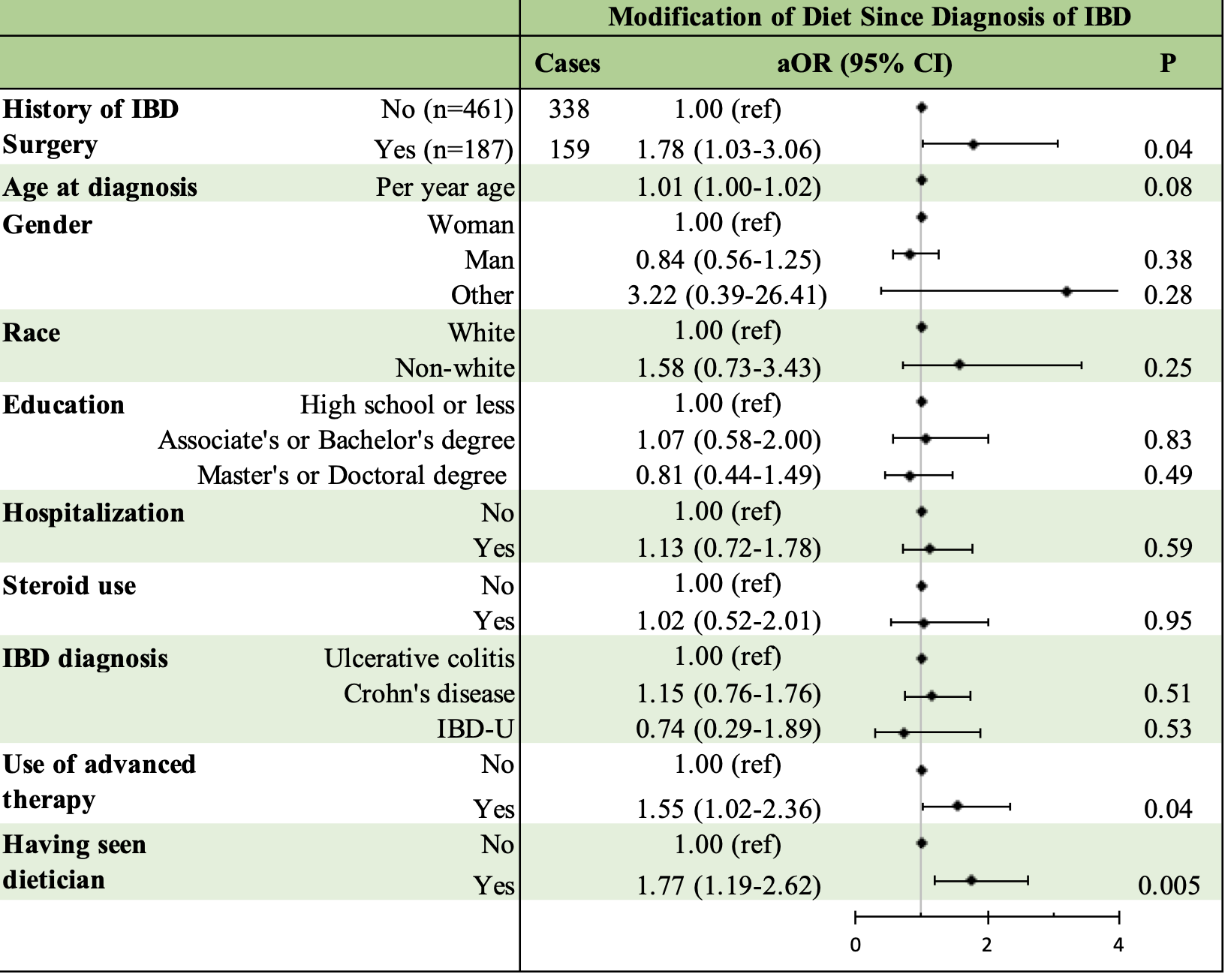
Figure: Table 1. Adjusted odds ratios for exploratory outcomes according to history of IBD surgery.
Disclosures:
Shawna Walsh indicated no relevant financial relationships.
Seerat Chawla indicated no relevant financial relationships.
Rachel Zhang indicated no relevant financial relationships.
Kevin Casey indicated no relevant financial relationships.
Ashwin Ananthakrishnan: Takeda – Grant/Research Support.
Bharati Kochar: Bristol Myers Squibb – Advisory Committee/Board Member. Pfizer, Inc – Advisory Committee/Board Member.
Emily Lopes indicated no relevant financial relationships.
Shawna E. Walsh, MD1, Seerat Chawla, BS, MSc2, Rachel Zhang, BS3, Kevin Casey, MPH1, Ashwin Ananthakrishnan, 4, Bharati Kochar, MD3, Emily Lopes, MD, MPH3. P1086 - Impact of IBD-Related Surgery on Dietary Practices and Perceptions in Patients With IBD, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Massachusetts General Hospital, Harvard Medical School, Boston, MA; 2Harvard Medical School, Boston, MA; 3Massachusetts General Hospital, Boston, MA; 4Division of Gastroenterology, Massachusetts General Hospital and Harvard Medical School, Boston, MA
Introduction: Evidence-based dietary recommendations for patients who have undergone surgery for IBD, such as diets for preventing recurrence or restrictions because of surgery, are limited. We aimed to compare dietary practices in those with and without a history of IBD-related surgery.
Methods: We administered a de-identified survey to IBD patients ≥18 years. We gathered demographics, medical and surgical history, dietary practices, and perceptions of dietary guidance. Participants self-confirmed diagnoses of Crohn’s disease (CD), ulcerative colitis (UC), or IBD-unclassified. The primary outcome was dietary modification due to IBD. Secondary outcomes included impact of IBD on appetite and enjoyment in eating, perception of diet as a trigger for flares, dietary supplement use, and comfort discussing diet with an IBD doctor. We used logistic regression to determine odds ratios (OR) and 95% CI for each outcome according to history of IBD-related surgery while adjusting for covariates.
Results: 648 respondents completed the survey (IBD-related surgery: yes=187, no=461). Those with a history of IBD-related surgery were younger at diagnosis (mean age 25 vs 33 years) and more likely to have CD (76.6 vs 42.2%); demographics were otherwise similar. Participants with IBD-related surgery were more likely to have modified their diet (aOR 1.78 (95%CI 1.03-3.06, p=0.04) when compared to those without surgery (Figure 1). In a subgroup analysis, those with a history of ileal pouch (n=42) were more likely to have modified their diet (aOR 4.08 (1.19-13.99), p=0.03) than those without, while those with a history of ostomy (n=28) were not (aOR 0.75 (0.28-1.98), p=0.56). Those with IBD-related surgery were also more likely to have appetite or enjoyment in eating affected by IBD, though this was not statistically significant (Table 1; p=0.06). More than 90% of respondents felt comfortable discussing diet with their IBD doctor, but less than 30% felt they received the “right amount” of dietary advice for their IBD.
Discussion: Patients with a history of IBD surgery, especially ileal pouches, were more likely to modify their diet and have appetite and enjoyment in eating impacted by their IBD. Though nearly all patients were comfortable discussing diet with their doctor, few felt they received adequate dietary guidance. Future studies and guidelines should better define dietary recommendations for those with IBD-related surgery, particularly ileal pouches.
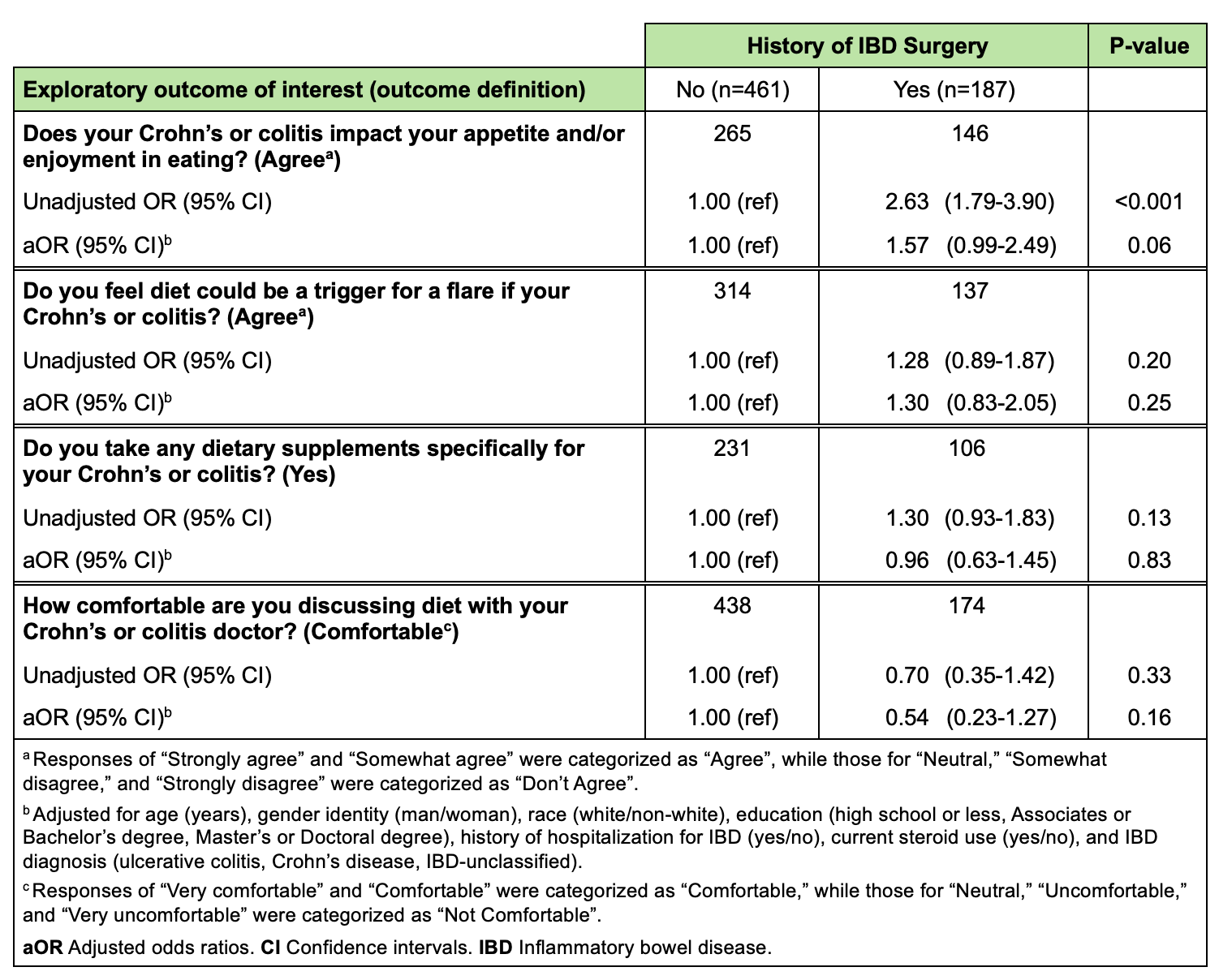
Figure: Figure 1. Adjusted odds ratios for having modified diet (primary outcome) according to history of IBD surgery (exposure of interest) and additional covariates. aOR Adjusted odds ratios. CI Confidence intervals. IBD Inflammatory bowel disease. IBD-U Inflammatory bowel disease unclassified.
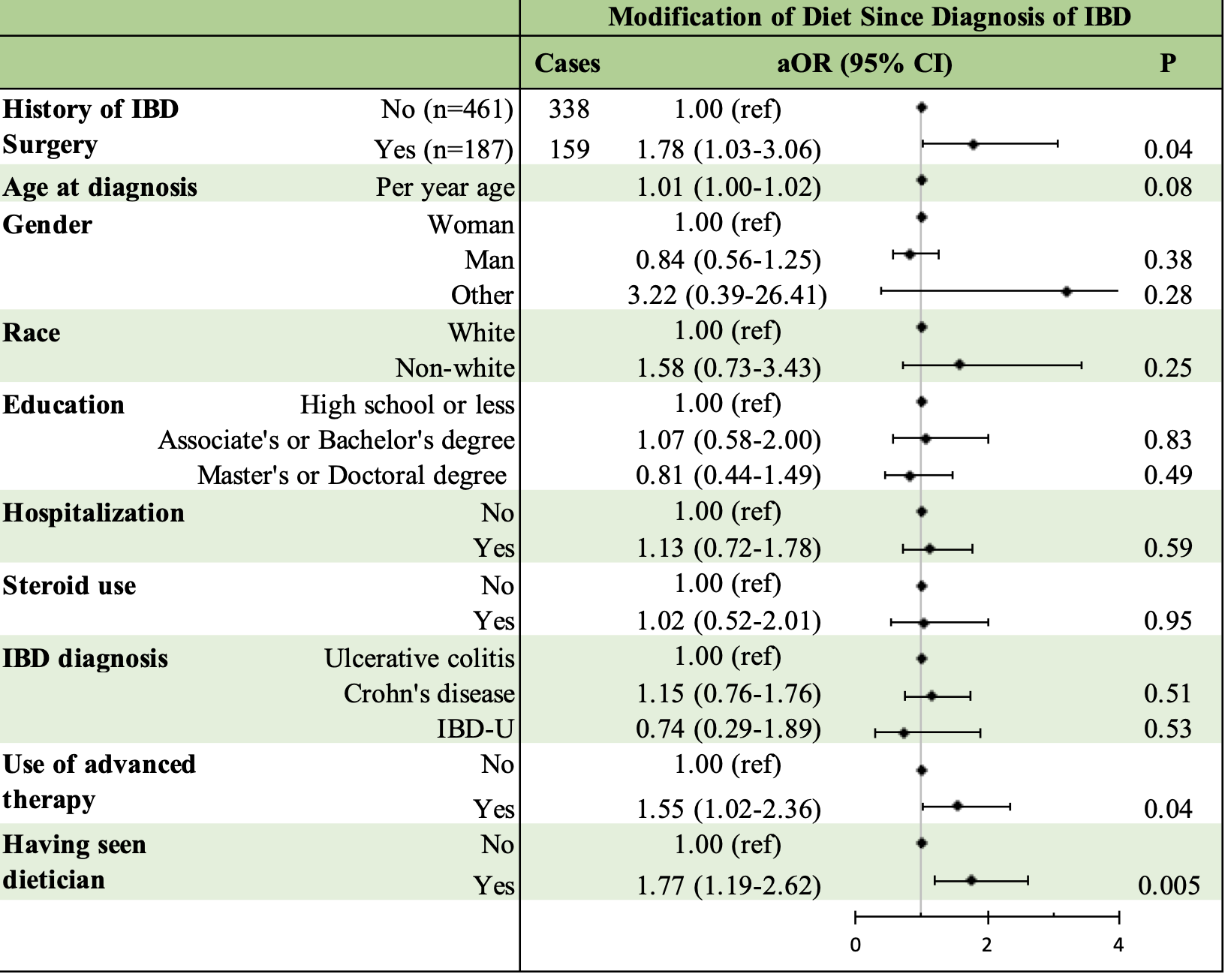
Figure: Table 1. Adjusted odds ratios for exploratory outcomes according to history of IBD surgery.
Disclosures:
Shawna Walsh indicated no relevant financial relationships.
Seerat Chawla indicated no relevant financial relationships.
Rachel Zhang indicated no relevant financial relationships.
Kevin Casey indicated no relevant financial relationships.
Ashwin Ananthakrishnan: Takeda – Grant/Research Support.
Bharati Kochar: Bristol Myers Squibb – Advisory Committee/Board Member. Pfizer, Inc – Advisory Committee/Board Member.
Emily Lopes indicated no relevant financial relationships.
Shawna E. Walsh, MD1, Seerat Chawla, BS, MSc2, Rachel Zhang, BS3, Kevin Casey, MPH1, Ashwin Ananthakrishnan, 4, Bharati Kochar, MD3, Emily Lopes, MD, MPH3. P1086 - Impact of IBD-Related Surgery on Dietary Practices and Perceptions in Patients With IBD, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.

