Sunday Poster Session
Category: IBD
P1259 - An Untold Case of Crohn’s or a Post-Op Complication?
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall
- JT
Jeremiah Thyagaraj, MD
NewYork-Presbyterian/Queens
Williston Park, NY
Presenting Author(s)
Jeremiah Thyagaraj, MD1, Hannah Gaddam, BS2, Jonah A. Thyagaraj, DO3, Lenny Jacome Yshii, BS4, Louis Cohen, MD, MS5, Pratima Dibba, MD6
1NewYork-Presbyterian/Queens, Williston Park, NY; 2New York Institute of Technology, Flushing, NY; 3Mount Sinai South Nassau, Williston Park, NY; 4Medical Offices of Manhattan, New York, NY; 5Icahn School of Medicine at Mount Sinai, New York, NY; 6Medical Offices of Manhattan/NYU, New York, NY
Introduction: Fistulas are abnormal connections between areas of the digestive tract that can form as a result of inflammatory bowel disease or surgery. About 40% of patients with Crohn’s will develop at least one fistula throughout their disease course [1]. Although incidence is not clearly defined, there have been reports of fistula development secondary to surgery. Understanding the origin of an enterocolic fistula would direct therapy. We present an evolving case of an incidental fistula found during a colonoscopy in a patient with diarrhea after an appendectomy and partial colectomy.
Case Description/
Methods: A 53-year-old male with a reported history of a ruptured appendix status post appendectomy and partial colectomy in 1998 in Yugoslavia presented for a screening colonoscopy with an incidental history of postoperative diarrhea. He had 10 loose bowel movements daily, reduced with loperamide. The colonoscopy revealed two seemingly appearing “diverticula” in close proximity to one another connected by an ulcerated intraluminal tract. One diverticula contained a partially visible lesion, concerning for an abscess or fistula. A fecal calprotectin was elevated at 304. Post-procedural CT scan revealed a stable segment of active inflammation in the distal ileum with probable fistula to the adjacent proximal transverse colon. Pathology results revealed focal ulceration with nonspecific chronic and active inflammation and mild architectural changes.
Discussion: On review of prior records, the patient had a retrocecal abscess presumed to be secondary to appendicitis, for which he underwent surgery with creation of an ileotransverse anastomosis. The abscess may have been due to complicated appendicitis or undiagnosed Crohn’s disease. His current presentation of a “fistulous” tract in the colon may represent ongoing active Crohn’s, new Crohn’s involving the ileotransverse anastomosis or deterioration of the surgical anastomosis without Crohn's. Crohn's is suspected based on the pathology, and CT scan, but chronic ischemic ulceration due to a complication at the surgical anastomosis remains a possibility. There is likely some bile acid malabsorption. His symptoms resolved with cholestyramine. We will re-evaluate with a small bowel series and a repeat colonoscopy in 6 months to decide upon management.
1. McGregor CGC, Tandon R, Simmons A. Pathogenesis of Fistulating Crohn’s Disease: A Review. Cellular and Molecular Gastroenterology and Hepatology. 2023;15(1):1-11. doi:https://doi.org/10.1016/j.jcmgh.2022.09.011

Figure: Abdominal CT scan revealing stable segment of active inflammation in the distal ileum with probable fistula to the adjacent proximal transverse colon.
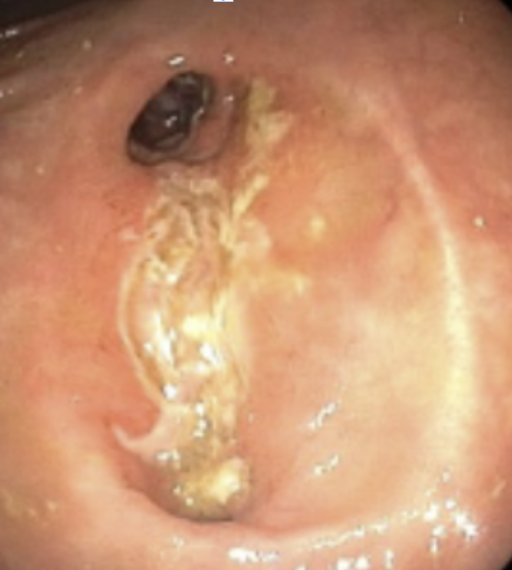
Figure: Two “diverticula” in close proximity connected by an ulcerated intraluminal tract.
Disclosures:
Jeremiah Thyagaraj indicated no relevant financial relationships.
Hannah Gaddam indicated no relevant financial relationships.
Jonah Thyagaraj indicated no relevant financial relationships.
Lenny Jacome Yshii indicated no relevant financial relationships.
Louis Cohen indicated no relevant financial relationships.
Pratima Dibba indicated no relevant financial relationships.
Jeremiah Thyagaraj, MD1, Hannah Gaddam, BS2, Jonah A. Thyagaraj, DO3, Lenny Jacome Yshii, BS4, Louis Cohen, MD, MS5, Pratima Dibba, MD6. P1259 - An Untold Case of Crohn’s or a Post-Op Complication?, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1NewYork-Presbyterian/Queens, Williston Park, NY; 2New York Institute of Technology, Flushing, NY; 3Mount Sinai South Nassau, Williston Park, NY; 4Medical Offices of Manhattan, New York, NY; 5Icahn School of Medicine at Mount Sinai, New York, NY; 6Medical Offices of Manhattan/NYU, New York, NY
Introduction: Fistulas are abnormal connections between areas of the digestive tract that can form as a result of inflammatory bowel disease or surgery. About 40% of patients with Crohn’s will develop at least one fistula throughout their disease course [1]. Although incidence is not clearly defined, there have been reports of fistula development secondary to surgery. Understanding the origin of an enterocolic fistula would direct therapy. We present an evolving case of an incidental fistula found during a colonoscopy in a patient with diarrhea after an appendectomy and partial colectomy.
Case Description/
Methods: A 53-year-old male with a reported history of a ruptured appendix status post appendectomy and partial colectomy in 1998 in Yugoslavia presented for a screening colonoscopy with an incidental history of postoperative diarrhea. He had 10 loose bowel movements daily, reduced with loperamide. The colonoscopy revealed two seemingly appearing “diverticula” in close proximity to one another connected by an ulcerated intraluminal tract. One diverticula contained a partially visible lesion, concerning for an abscess or fistula. A fecal calprotectin was elevated at 304. Post-procedural CT scan revealed a stable segment of active inflammation in the distal ileum with probable fistula to the adjacent proximal transverse colon. Pathology results revealed focal ulceration with nonspecific chronic and active inflammation and mild architectural changes.
Discussion: On review of prior records, the patient had a retrocecal abscess presumed to be secondary to appendicitis, for which he underwent surgery with creation of an ileotransverse anastomosis. The abscess may have been due to complicated appendicitis or undiagnosed Crohn’s disease. His current presentation of a “fistulous” tract in the colon may represent ongoing active Crohn’s, new Crohn’s involving the ileotransverse anastomosis or deterioration of the surgical anastomosis without Crohn's. Crohn's is suspected based on the pathology, and CT scan, but chronic ischemic ulceration due to a complication at the surgical anastomosis remains a possibility. There is likely some bile acid malabsorption. His symptoms resolved with cholestyramine. We will re-evaluate with a small bowel series and a repeat colonoscopy in 6 months to decide upon management.
1. McGregor CGC, Tandon R, Simmons A. Pathogenesis of Fistulating Crohn’s Disease: A Review. Cellular and Molecular Gastroenterology and Hepatology. 2023;15(1):1-11. doi:https://doi.org/10.1016/j.jcmgh.2022.09.011

Figure: Abdominal CT scan revealing stable segment of active inflammation in the distal ileum with probable fistula to the adjacent proximal transverse colon.
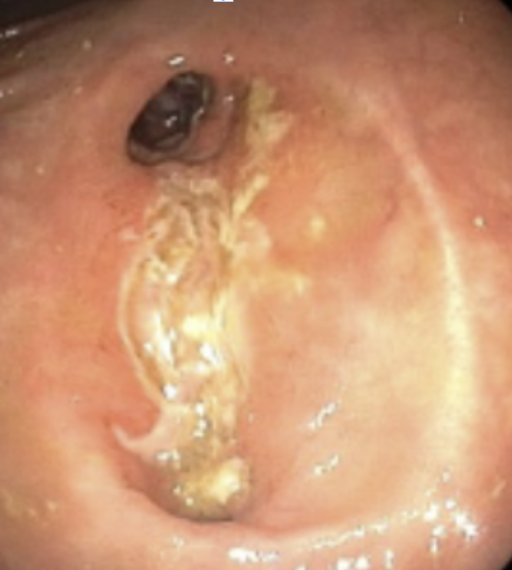
Figure: Two “diverticula” in close proximity connected by an ulcerated intraluminal tract.
Disclosures:
Jeremiah Thyagaraj indicated no relevant financial relationships.
Hannah Gaddam indicated no relevant financial relationships.
Jonah Thyagaraj indicated no relevant financial relationships.
Lenny Jacome Yshii indicated no relevant financial relationships.
Louis Cohen indicated no relevant financial relationships.
Pratima Dibba indicated no relevant financial relationships.
Jeremiah Thyagaraj, MD1, Hannah Gaddam, BS2, Jonah A. Thyagaraj, DO3, Lenny Jacome Yshii, BS4, Louis Cohen, MD, MS5, Pratima Dibba, MD6. P1259 - An Untold Case of Crohn’s or a Post-Op Complication?, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
