Sunday Poster Session
Category: IBD
P1256 - Beyond the Colon: Acute Hemolysis Associated With Etrasimod
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall

Saud Khan, MD (he/him/his)
University of Central Florida, HCA Healthcare GME
Orlando, FL
Presenting Author(s)
Saud Khan, MD1, Eric Vargas, MD2, Jonathan Pinheiro, MD2, Sohaib Ahmed, MD2, Michael Delzoppo, DO1
1University of Central Florida, HCA Healthcare GME, Orlando, FL; 2Orlando VA Medical Center and UCF/HCA Greater Orlando, Orlando, FL
Introduction: Ulcerative colitis (UC) is a chronic inflammatory disease of the colon. It's management has evolved with the introduction of targeted immune modulators. Etrasimod is an oral sphingosine 1-phosphate (S1P) receptor modulator that was approved in 2023 for moderately to severely active UC in adults. We present the first reported case of acute hemolytic anemia associated with etrasimod therapy.
Case Description/
Methods: A 31-year-old man with a history of hypertension on amlodipine and controlled UC presented to the hospital after pre-endoscopy workup showed macrocytic anemia. His UC treatment changed from tofacitinib to etrasimod 2 months prior. He denied recent travel, alcohol use, other drugs or supplements, fever, night sweats, significant weight loss or recent UC flares. He had no family history of malignancy, hematologic or autoimmune disorder. He reported progressive fatigue for 1 month and one episode of diarrhea 2 weeks prior. Initial studies showed macrocytic anemia, reticulocyte count 22%. Labwork was unremarkable, except elevated D-dimer and high ferritin. Peripheral blood smear revealed schistocytes, polychromatophilia and teardrop cells. Viral serologies including hepatitis and HIV were negative. G6PD testing was negative. Immunoglobulins were normal, without monoclonal proteins. Cold agglutinin were absent. Direct antiglobulin test (DAT) was positive for IgG but negative for complement. Etrasimod was discontinued and he received two units of packed red cells. Serial testing demonstrated persistent hemolysis (Figure 1). Hematology recommended 100mg prednisone daily which was started on day 7, with recovery of hemoglobin. Follow up colonoscopy did not show active flare.
Discussion: Drug-induced immune hemolytic anemia is a rare (1/1-2mil)1 adverse event. Mechanisms include drug adsorption, immune complex mediated or autoantibody induction2-4. In our patient, the positive DAT for IgG suggests immune-mediation. Etrasimod is a selective S1P receptor modulator that causes partial sequestration of lymphocytes in lymphoid tissues. The most common adverse effects include headache, elevated liver enzymes, dizziness, arthralgia, nausea, and hypertension5-8. Specific cases of hemolytic anemia have not been previously reported. The exact mechanism that triggered hemolysis remains unclear. UC may rarely manifest as acute hemolysis associated with acute flares, however our patient was at baseline. This case aims to add to the literature and report a rare adverse advent of this new medication.
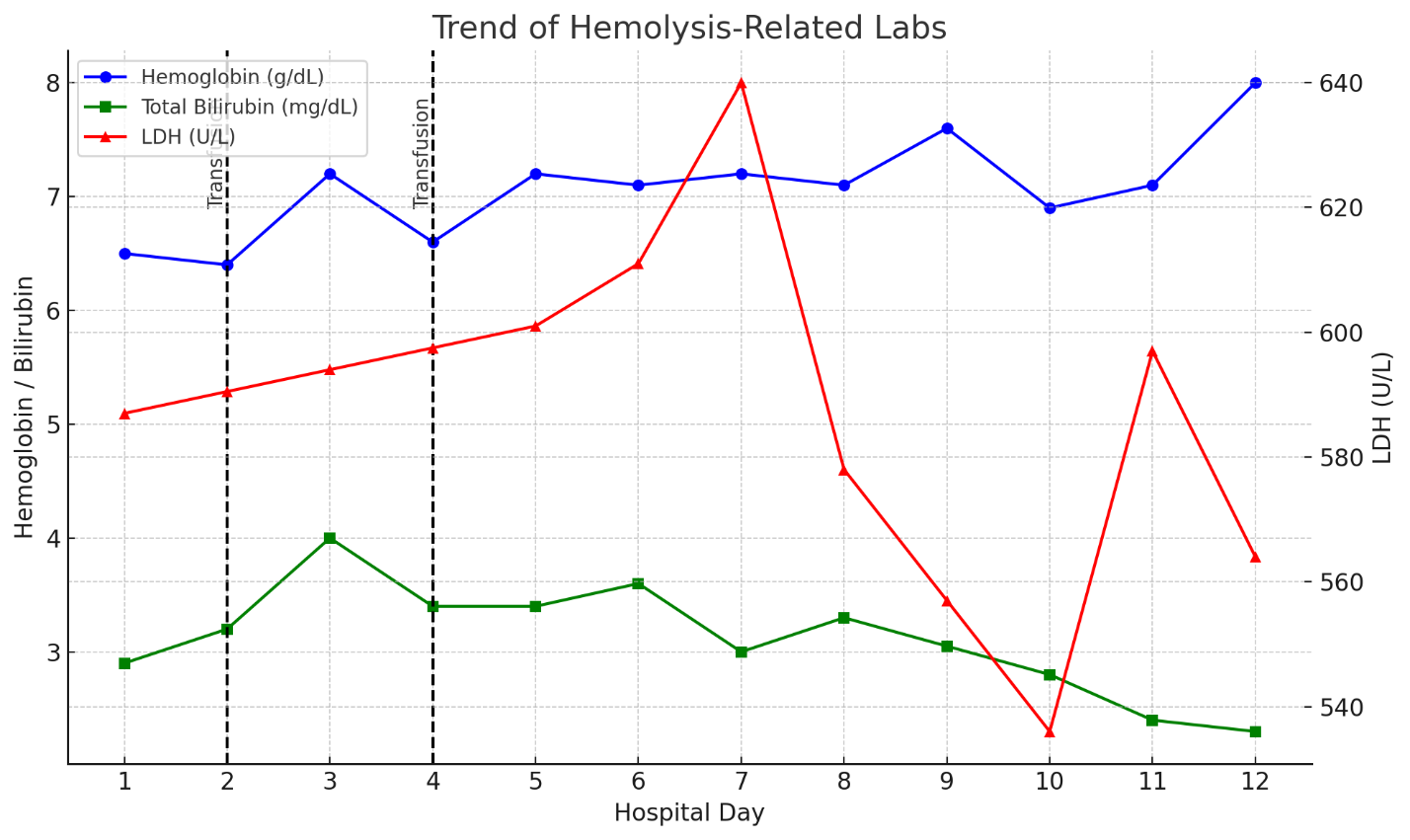
Figure: Figure 1: Trend of hemolysis related labs. (LDH: lactate dehydrogenase)
Disclosures:
Saud Khan indicated no relevant financial relationships.
Eric Vargas indicated no relevant financial relationships.
Jonathan Pinheiro indicated no relevant financial relationships.
Sohaib Ahmed indicated no relevant financial relationships.
Michael Delzoppo indicated no relevant financial relationships.
Saud Khan, MD1, Eric Vargas, MD2, Jonathan Pinheiro, MD2, Sohaib Ahmed, MD2, Michael Delzoppo, DO1. P1256 - Beyond the Colon: Acute Hemolysis Associated With Etrasimod, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1University of Central Florida, HCA Healthcare GME, Orlando, FL; 2Orlando VA Medical Center and UCF/HCA Greater Orlando, Orlando, FL
Introduction: Ulcerative colitis (UC) is a chronic inflammatory disease of the colon. It's management has evolved with the introduction of targeted immune modulators. Etrasimod is an oral sphingosine 1-phosphate (S1P) receptor modulator that was approved in 2023 for moderately to severely active UC in adults. We present the first reported case of acute hemolytic anemia associated with etrasimod therapy.
Case Description/
Methods: A 31-year-old man with a history of hypertension on amlodipine and controlled UC presented to the hospital after pre-endoscopy workup showed macrocytic anemia. His UC treatment changed from tofacitinib to etrasimod 2 months prior. He denied recent travel, alcohol use, other drugs or supplements, fever, night sweats, significant weight loss or recent UC flares. He had no family history of malignancy, hematologic or autoimmune disorder. He reported progressive fatigue for 1 month and one episode of diarrhea 2 weeks prior. Initial studies showed macrocytic anemia, reticulocyte count 22%. Labwork was unremarkable, except elevated D-dimer and high ferritin. Peripheral blood smear revealed schistocytes, polychromatophilia and teardrop cells. Viral serologies including hepatitis and HIV were negative. G6PD testing was negative. Immunoglobulins were normal, without monoclonal proteins. Cold agglutinin were absent. Direct antiglobulin test (DAT) was positive for IgG but negative for complement. Etrasimod was discontinued and he received two units of packed red cells. Serial testing demonstrated persistent hemolysis (Figure 1). Hematology recommended 100mg prednisone daily which was started on day 7, with recovery of hemoglobin. Follow up colonoscopy did not show active flare.
Discussion: Drug-induced immune hemolytic anemia is a rare (1/1-2mil)1 adverse event. Mechanisms include drug adsorption, immune complex mediated or autoantibody induction2-4. In our patient, the positive DAT for IgG suggests immune-mediation. Etrasimod is a selective S1P receptor modulator that causes partial sequestration of lymphocytes in lymphoid tissues. The most common adverse effects include headache, elevated liver enzymes, dizziness, arthralgia, nausea, and hypertension5-8. Specific cases of hemolytic anemia have not been previously reported. The exact mechanism that triggered hemolysis remains unclear. UC may rarely manifest as acute hemolysis associated with acute flares, however our patient was at baseline. This case aims to add to the literature and report a rare adverse advent of this new medication.
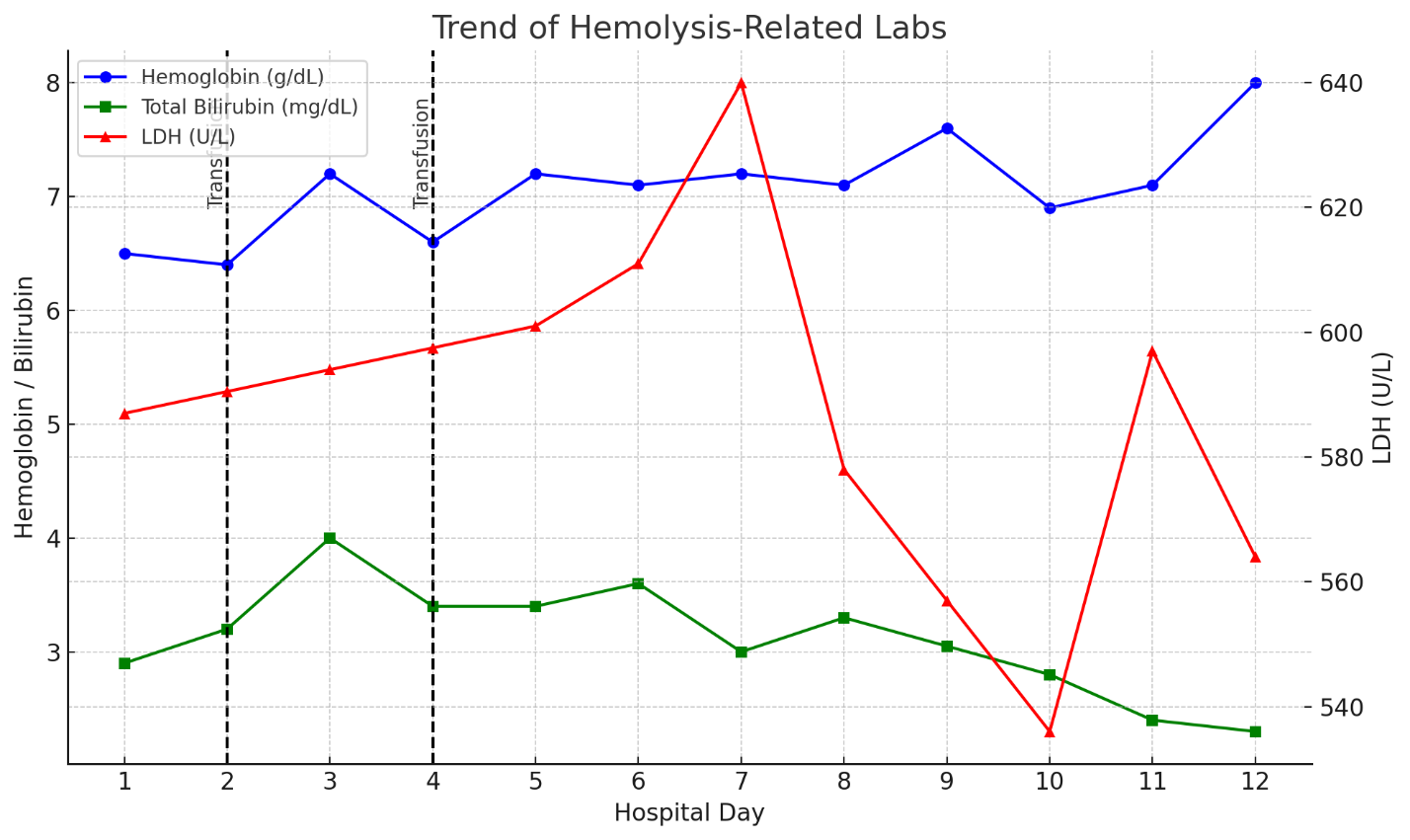
Figure: Figure 1: Trend of hemolysis related labs. (LDH: lactate dehydrogenase)
Disclosures:
Saud Khan indicated no relevant financial relationships.
Eric Vargas indicated no relevant financial relationships.
Jonathan Pinheiro indicated no relevant financial relationships.
Sohaib Ahmed indicated no relevant financial relationships.
Michael Delzoppo indicated no relevant financial relationships.
Saud Khan, MD1, Eric Vargas, MD2, Jonathan Pinheiro, MD2, Sohaib Ahmed, MD2, Michael Delzoppo, DO1. P1256 - Beyond the Colon: Acute Hemolysis Associated With Etrasimod, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
