Sunday Poster Session
Category: IBD
P1242 - Enterolith-Associated Enterocutaneous Fistula in Ulcerative Colitis: A Rare Complication
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall

Muskan Jain, MBBS (she/her/hers)
Kasturba Medical College, Manipal
Manipal, Karnataka, India
Presenting Author(s)
Siddharth Dwivedi, MBBS1, Muskan Jain, MBBS2, Vatsalya Choudhary, MBBS2, Balaji Musunuri, DNB (Gastro), MD, MBBS2, Ganesh C. Pai, DM (Gastro), MD, MBBS2
1Kasturba Medical College Manipal, Manipal, Karnataka, India; 2Kasturba Medical College, Manipal, Manipal, Karnataka, India
Introduction: Ulcerative colitis (UC) is a chronic inflammatory disorder usually confined to the colonic mucosa. Medically-refractory UC is managed with total proctocolectomy with ileal pouch-anal anastomosis. While most have good functional outcomes, rare complications like enterolith formation can lead to enterocutaneous fistula. Enteroliths are rock-like hard deposits in the lumen of the gastrointestinal tract, often caused by intestinal stasis, tumours, tuberculosis, and kinking due to adhesions, among various other causes. We report a rare case of chronic enterocutaneous fistula due to enteroliths in a patient with IBD-UC, twenty-two years after total colectomy with ileostomy.
Case Description/
Methods: A 55-year-old male with a history of UC status-post total colectomy with ileostomy presented with a four-day history of umbilical pain, intermittent stomal bleeding, and fecal discharge with greenish-yellow pus from an umbilical wound. Discharge aggravated with food intake from both sites. He also reported redness and itching around the wound, which was relieved by topical ointments. Physical examination revealed a stoma bag at the RIF end-ileostomy, and a fistulous opening at the umbilicus with fecal drainage; mild tenderness was also noted. Routine labs revealed high CRP. Abdominal CECT showed a 6.4×6.3mm enterocutaneous fistula, a 14mm circumferential irregular wall thickening of mid and distal ileal loops near the fistula, and a gallstone(Figures A, B). Enteroscopy revealed two linear ulcers and two black calculi at 22cm and 25cm, measuring 2x2 cm and 1x1 cm respectively(Figures Ca, Cb). Enteroliths were removed with Roth’s net. Biopsies confirmed ulcerated ileal mucosa with neutrophilic and lymphocytic infiltrates in the lamina propria with no evidence of granulomas.
Discussion: Enterolithiasis is rare, with a prevalence of 0.3% to 10%. Mortality is low in uncomplicated cases but can rise to 3% with delayed diagnosis or obstruction in debilitated patients. Crohn’s disease and intestinal tuberculosis are the most common causes; enteroliths are rare in ulcerative colitis (UC). Fistulas are also uncommon in UC and are typically perianal when present. This case is unusual, as a persistent enterolith led to a chronic enterocutaneous fistula in a UC patient—an atypical complication. Primary enteroliths remain a rare entity, mostly reported in isolated cases involving bowel obstruction. This case highlights an uncommon presentation that broadens the differential diagnosis for fistulizing disease in UC.
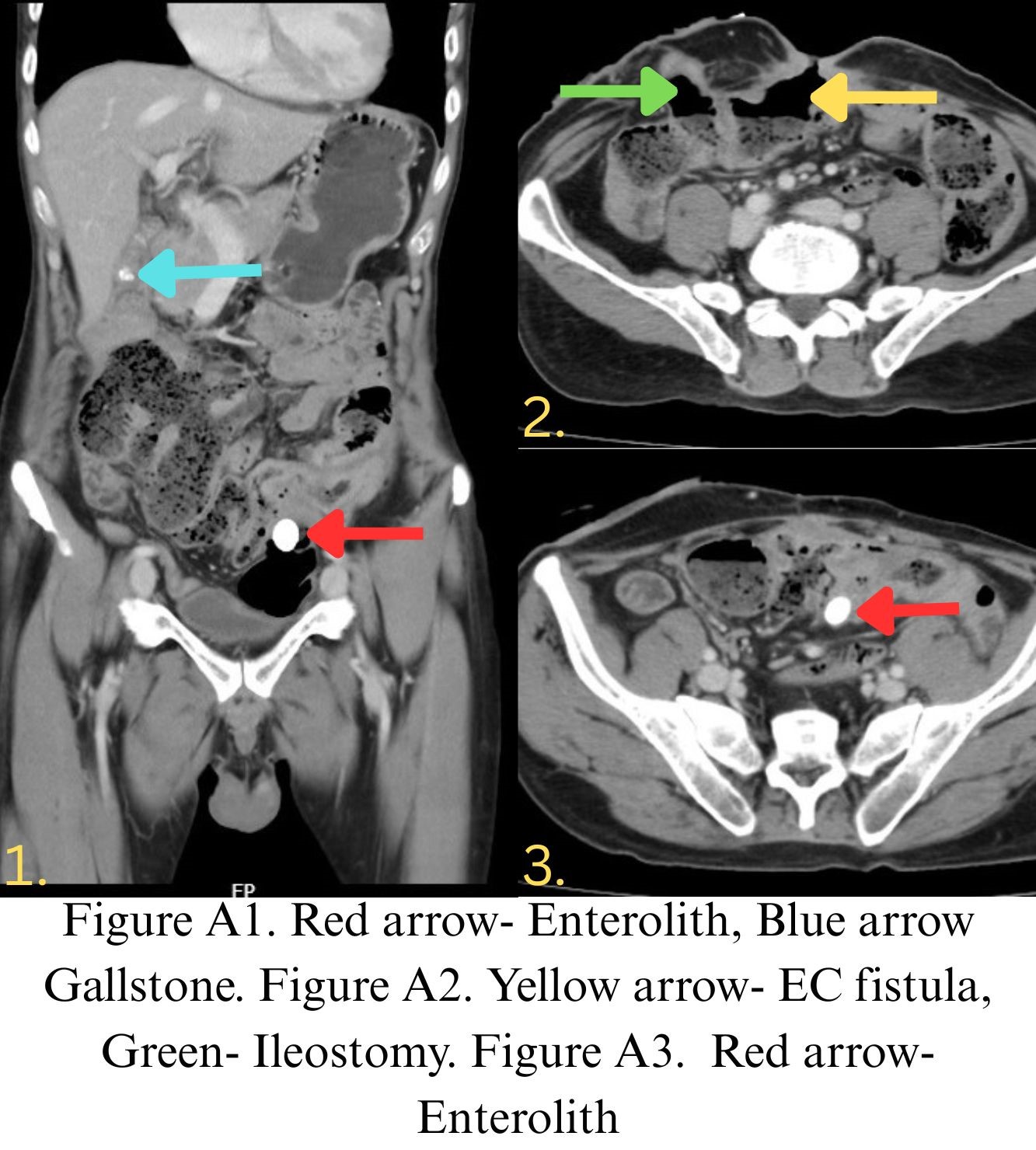
Figure: Figure A1. Red arrow- Enterolith, Blue arrow- Gallstone. Figure A2. Yellow arrow- EC fistula, Green arrow- Ileostomy. Figure A3. Red arrow- Enterolith
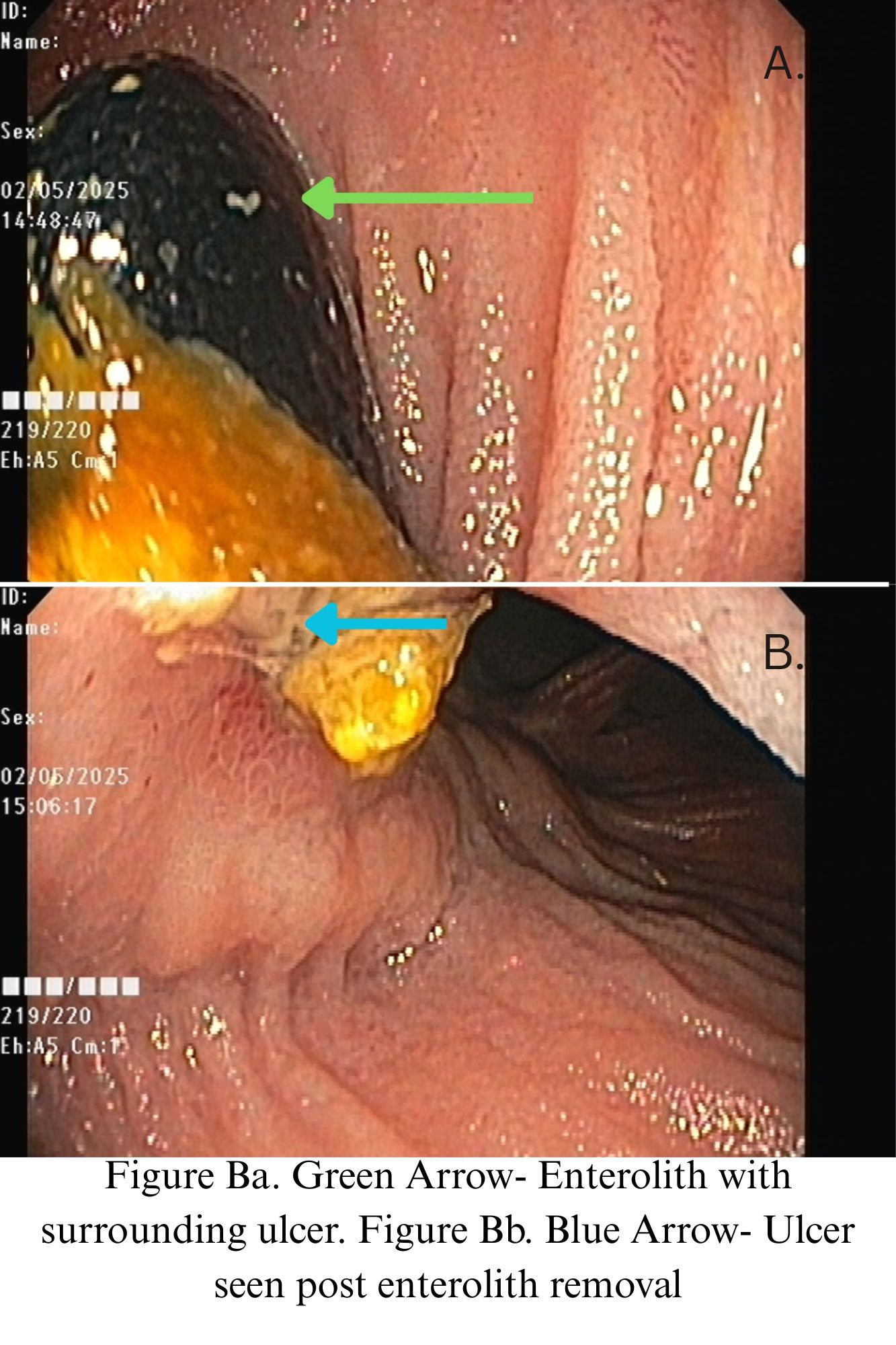
Figure: Figure Ba. Green Arrow- Enterolith with surrounding ulcer. Figure Bb. Blue Arrow- Ulcer seen post enterolith removal
Disclosures:
Siddharth Dwivedi indicated no relevant financial relationships.
Muskan Jain indicated no relevant financial relationships.
Vatsalya Choudhary indicated no relevant financial relationships.
Balaji Musunuri indicated no relevant financial relationships.
Ganesh Pai indicated no relevant financial relationships.
Siddharth Dwivedi, MBBS1, Muskan Jain, MBBS2, Vatsalya Choudhary, MBBS2, Balaji Musunuri, DNB (Gastro), MD, MBBS2, Ganesh C. Pai, DM (Gastro), MD, MBBS2. P1242 - Enterolith-Associated Enterocutaneous Fistula in Ulcerative Colitis: A Rare Complication, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Kasturba Medical College Manipal, Manipal, Karnataka, India; 2Kasturba Medical College, Manipal, Manipal, Karnataka, India
Introduction: Ulcerative colitis (UC) is a chronic inflammatory disorder usually confined to the colonic mucosa. Medically-refractory UC is managed with total proctocolectomy with ileal pouch-anal anastomosis. While most have good functional outcomes, rare complications like enterolith formation can lead to enterocutaneous fistula. Enteroliths are rock-like hard deposits in the lumen of the gastrointestinal tract, often caused by intestinal stasis, tumours, tuberculosis, and kinking due to adhesions, among various other causes. We report a rare case of chronic enterocutaneous fistula due to enteroliths in a patient with IBD-UC, twenty-two years after total colectomy with ileostomy.
Case Description/
Methods: A 55-year-old male with a history of UC status-post total colectomy with ileostomy presented with a four-day history of umbilical pain, intermittent stomal bleeding, and fecal discharge with greenish-yellow pus from an umbilical wound. Discharge aggravated with food intake from both sites. He also reported redness and itching around the wound, which was relieved by topical ointments. Physical examination revealed a stoma bag at the RIF end-ileostomy, and a fistulous opening at the umbilicus with fecal drainage; mild tenderness was also noted. Routine labs revealed high CRP. Abdominal CECT showed a 6.4×6.3mm enterocutaneous fistula, a 14mm circumferential irregular wall thickening of mid and distal ileal loops near the fistula, and a gallstone(Figures A, B). Enteroscopy revealed two linear ulcers and two black calculi at 22cm and 25cm, measuring 2x2 cm and 1x1 cm respectively(Figures Ca, Cb). Enteroliths were removed with Roth’s net. Biopsies confirmed ulcerated ileal mucosa with neutrophilic and lymphocytic infiltrates in the lamina propria with no evidence of granulomas.
Discussion: Enterolithiasis is rare, with a prevalence of 0.3% to 10%. Mortality is low in uncomplicated cases but can rise to 3% with delayed diagnosis or obstruction in debilitated patients. Crohn’s disease and intestinal tuberculosis are the most common causes; enteroliths are rare in ulcerative colitis (UC). Fistulas are also uncommon in UC and are typically perianal when present. This case is unusual, as a persistent enterolith led to a chronic enterocutaneous fistula in a UC patient—an atypical complication. Primary enteroliths remain a rare entity, mostly reported in isolated cases involving bowel obstruction. This case highlights an uncommon presentation that broadens the differential diagnosis for fistulizing disease in UC.
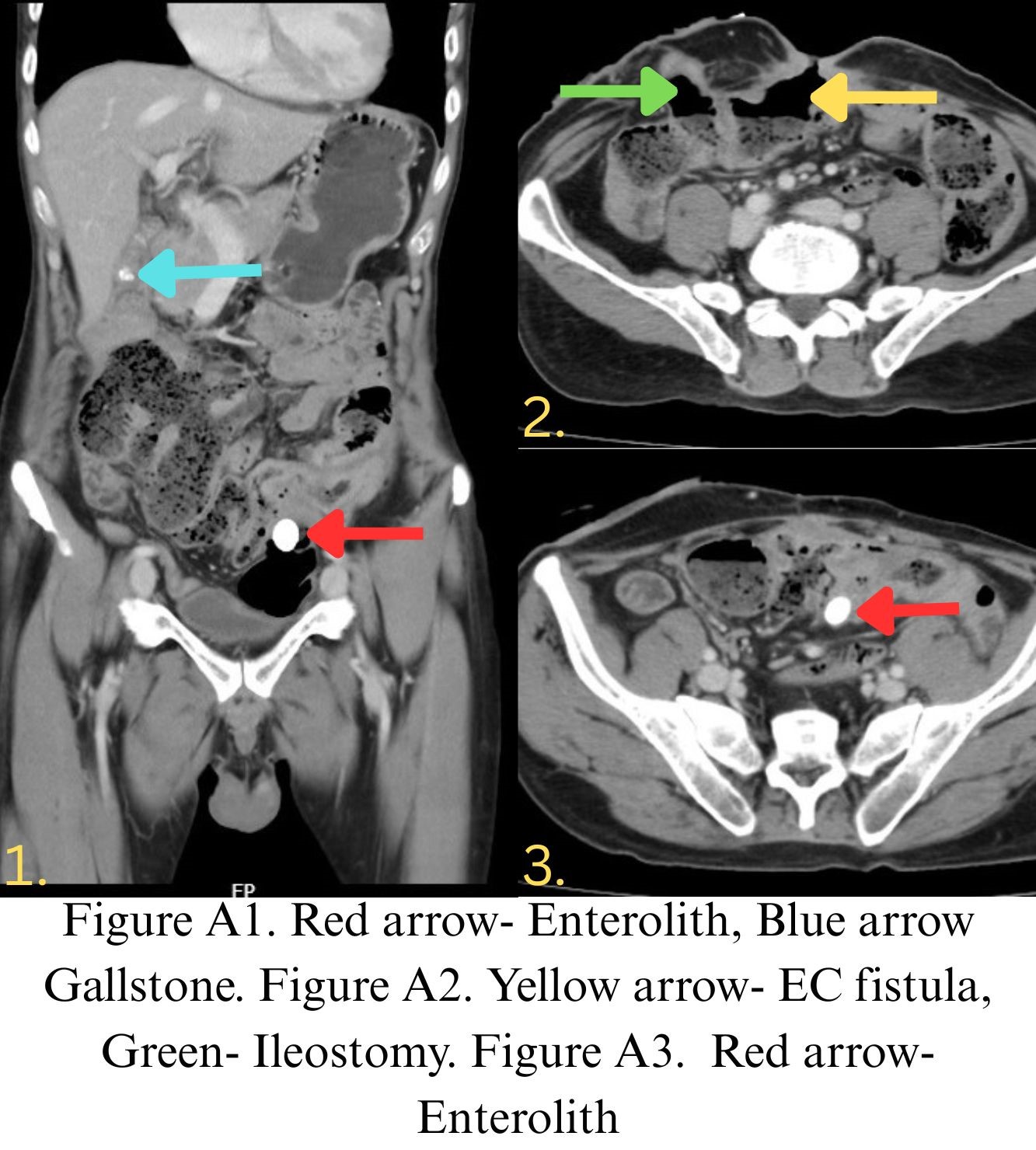
Figure: Figure A1. Red arrow- Enterolith, Blue arrow- Gallstone. Figure A2. Yellow arrow- EC fistula, Green arrow- Ileostomy. Figure A3. Red arrow- Enterolith
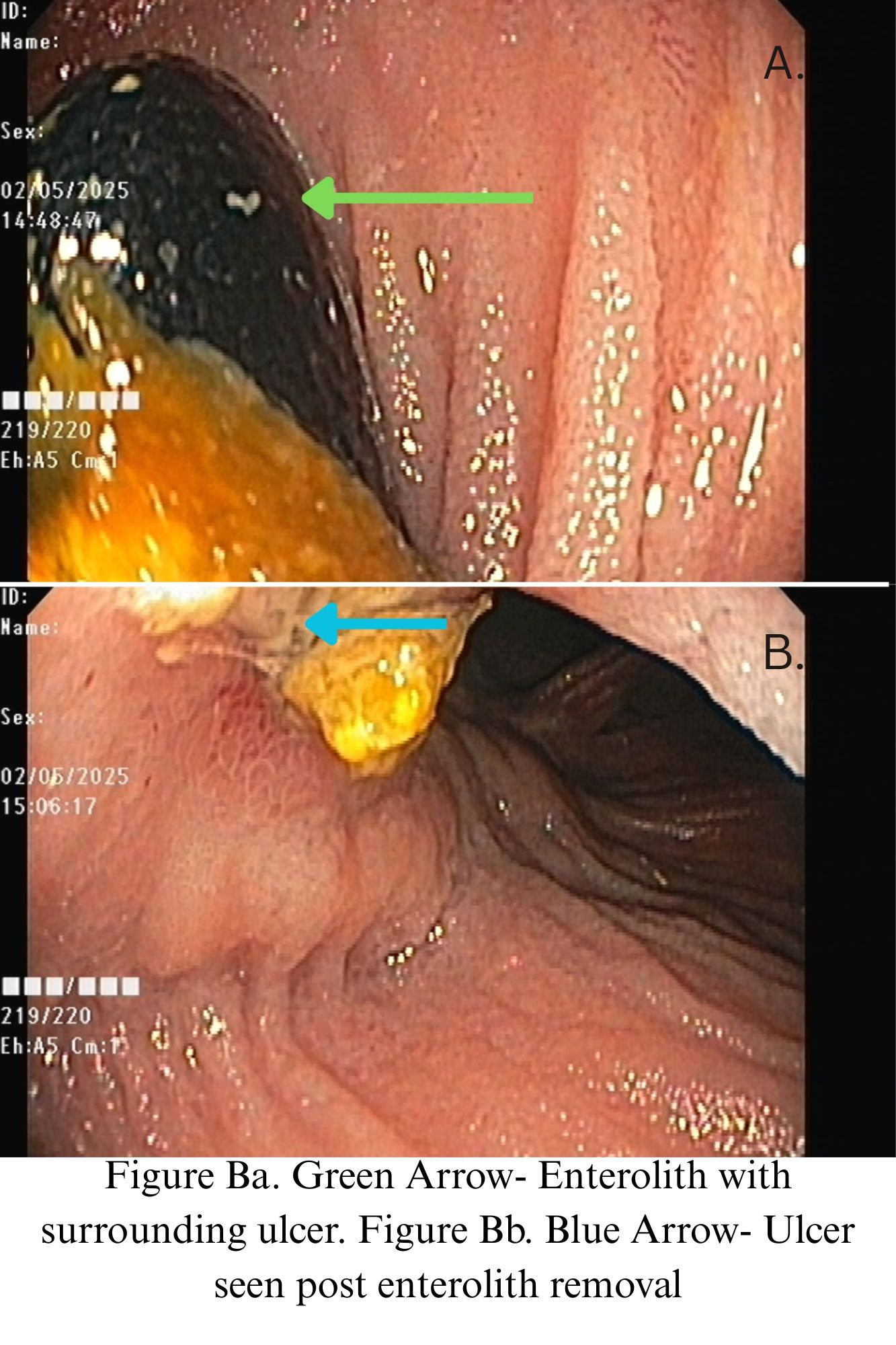
Figure: Figure Ba. Green Arrow- Enterolith with surrounding ulcer. Figure Bb. Blue Arrow- Ulcer seen post enterolith removal
Disclosures:
Siddharth Dwivedi indicated no relevant financial relationships.
Muskan Jain indicated no relevant financial relationships.
Vatsalya Choudhary indicated no relevant financial relationships.
Balaji Musunuri indicated no relevant financial relationships.
Ganesh Pai indicated no relevant financial relationships.
Siddharth Dwivedi, MBBS1, Muskan Jain, MBBS2, Vatsalya Choudhary, MBBS2, Balaji Musunuri, DNB (Gastro), MD, MBBS2, Ganesh C. Pai, DM (Gastro), MD, MBBS2. P1242 - Enterolith-Associated Enterocutaneous Fistula in Ulcerative Colitis: A Rare Complication, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
