Sunday Poster Session
Category: Infections and Microbiome
P1324 - Chronic Entamoeba Histolytica Infection Leading to Loeffler Endocarditis: A Rare Case
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall

Neal K. Bhachawat, DO
Houston Methodist Hospital
Houston, TX
Presenting Author(s)
Neal K. Bhachawat, DO, Muneeb Ajaz, MD, Miles Hill, MS, Henry Ellison, MD
Houston Methodist Hospital, Houston, TX
Introduction: Entamoeba histolytica is an invasive protozoan that typically causes amebic dysentery characterized by abdominal pain and bloody diarrhea. Chronic, untreated infection may trigger hypereosinophilic syndrome(HES), with cardiac involvement, known as Loeffler endocarditis, occurring in approximately 40–50% of HES cases. We present a rare case of symptomatic chronic E. histolytica infection resulting in Loeffler endocarditis.
Case Description/
Methods: A 70-year-old woman with a PMH of type 2 DM, HTN, and hypothyroidism presented with worsening exertional dyspnea and lower extremity edema for 3 weeks. Review of systems was notable for chronic, intermittent abdominal pain and diarrhea for several years. Physical examination revealed generalized abdominal tenderness and anasarca. Laboratory evaluation, including review of prior medical records, revealed intermittent eosinophilia with absolute eosinophil counts exceeding 1500 cells/μL, a pattern that had been present for two decades. Patient reported intermittent travel to Mexico. Stool studies and abdominal imaging identified E. histolytica infection and colitis of the ascending and transverse colon (image 1). Transthoracic echocardiography revealed a LVEF of 40–49%, subendocardial calcifications in the lateral and apical walls of the left ventricle (LV), and an enlarged right ventricle with severely depressed systolic function(image 2). Cardiac MRI showed prominent subendocardial late gadolinium enhancement of the lateral and apical LV wall, and an apical mural thrombus, findings consistent with Loeffler endocarditis. Patient was diagnosed with acute decompensated heart failure and started on guideline-directed medical therapy. She was treated for E. histolytica infection with systemic metronidazole and intraluminal nitazoxanide, resulting in resolution of eosinophilia and improvement in her chronic GI symptoms.
Discussion: E. histolytica’s chronic, non-bloody form is rare and often misdiagnosed. This case demonstrates a rare complication of chronic amebic infection—Loeffler endocarditis, a fibrotic and restrictive cardiomyopathy caused by eosinophilic infiltration of the endomyocardium, which carries a two-year mortality rate of 35–50%. Early diagnosis and treatment of the underlying etiology are critical to prevent irreversible cardiac damage. This case underscores the importance of maintaining a high index of suspicion for parasitic causes in patients with unexplained eosinophilia, chronic gastrointestinal symptoms, and a compatible travel history.
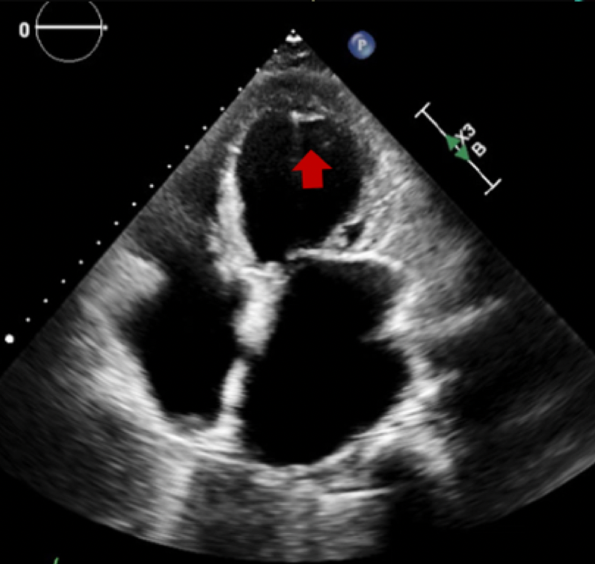
Figure: Image 1: Compute Tomography (CT) abdomen/pelvis with intravenous contrast showing mild ascending and proximal transverse colonic wall thickening (yellow arrow), suggestive of colitis.

Figure: Image 2: Transthoracic echocardiogram apical 4 chamber view showing irregular linear echo-dense mass along subendocardial left ventricular myocardium involving the distal inferolateral wall and the apex (red arrows).
Disclosures:
Neal Bhachawat indicated no relevant financial relationships.
Muneeb Ajaz indicated no relevant financial relationships.
Miles Hill indicated no relevant financial relationships.
Henry Ellison indicated no relevant financial relationships.
Neal K. Bhachawat, DO, Muneeb Ajaz, MD, Miles Hill, MS, Henry Ellison, MD. P1324 - Chronic Entamoeba Histolytica Infection Leading to Loeffler Endocarditis: A Rare Case, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
Houston Methodist Hospital, Houston, TX
Introduction: Entamoeba histolytica is an invasive protozoan that typically causes amebic dysentery characterized by abdominal pain and bloody diarrhea. Chronic, untreated infection may trigger hypereosinophilic syndrome(HES), with cardiac involvement, known as Loeffler endocarditis, occurring in approximately 40–50% of HES cases. We present a rare case of symptomatic chronic E. histolytica infection resulting in Loeffler endocarditis.
Case Description/
Methods: A 70-year-old woman with a PMH of type 2 DM, HTN, and hypothyroidism presented with worsening exertional dyspnea and lower extremity edema for 3 weeks. Review of systems was notable for chronic, intermittent abdominal pain and diarrhea for several years. Physical examination revealed generalized abdominal tenderness and anasarca. Laboratory evaluation, including review of prior medical records, revealed intermittent eosinophilia with absolute eosinophil counts exceeding 1500 cells/μL, a pattern that had been present for two decades. Patient reported intermittent travel to Mexico. Stool studies and abdominal imaging identified E. histolytica infection and colitis of the ascending and transverse colon (image 1). Transthoracic echocardiography revealed a LVEF of 40–49%, subendocardial calcifications in the lateral and apical walls of the left ventricle (LV), and an enlarged right ventricle with severely depressed systolic function(image 2). Cardiac MRI showed prominent subendocardial late gadolinium enhancement of the lateral and apical LV wall, and an apical mural thrombus, findings consistent with Loeffler endocarditis. Patient was diagnosed with acute decompensated heart failure and started on guideline-directed medical therapy. She was treated for E. histolytica infection with systemic metronidazole and intraluminal nitazoxanide, resulting in resolution of eosinophilia and improvement in her chronic GI symptoms.
Discussion: E. histolytica’s chronic, non-bloody form is rare and often misdiagnosed. This case demonstrates a rare complication of chronic amebic infection—Loeffler endocarditis, a fibrotic and restrictive cardiomyopathy caused by eosinophilic infiltration of the endomyocardium, which carries a two-year mortality rate of 35–50%. Early diagnosis and treatment of the underlying etiology are critical to prevent irreversible cardiac damage. This case underscores the importance of maintaining a high index of suspicion for parasitic causes in patients with unexplained eosinophilia, chronic gastrointestinal symptoms, and a compatible travel history.
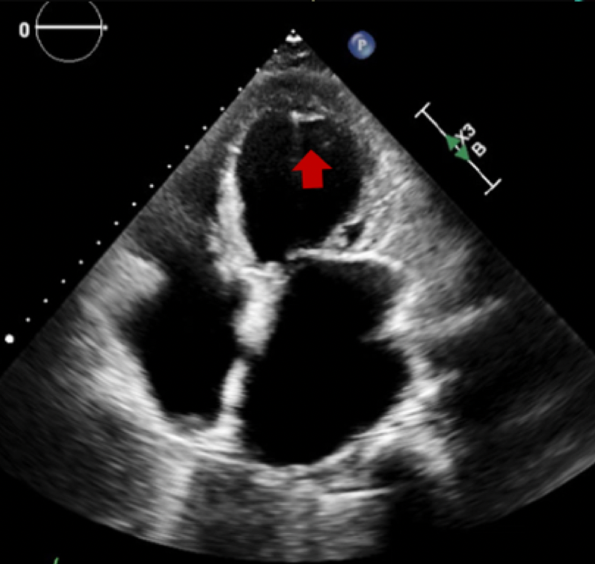
Figure: Image 1: Compute Tomography (CT) abdomen/pelvis with intravenous contrast showing mild ascending and proximal transverse colonic wall thickening (yellow arrow), suggestive of colitis.

Figure: Image 2: Transthoracic echocardiogram apical 4 chamber view showing irregular linear echo-dense mass along subendocardial left ventricular myocardium involving the distal inferolateral wall and the apex (red arrows).
Disclosures:
Neal Bhachawat indicated no relevant financial relationships.
Muneeb Ajaz indicated no relevant financial relationships.
Miles Hill indicated no relevant financial relationships.
Henry Ellison indicated no relevant financial relationships.
Neal K. Bhachawat, DO, Muneeb Ajaz, MD, Miles Hill, MS, Henry Ellison, MD. P1324 - Chronic Entamoeba Histolytica Infection Leading to Loeffler Endocarditis: A Rare Case, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
