Sunday Poster Session
Category: Infections and Microbiome
P1323 - Black Fungus Ulcer: A Case of Severe Gastric Mucormycosis
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall

Angela Xue, MD (she/her/hers)
NYU Langone Health
New York, NY
Presenting Author(s)
Angela Xue, MD1, Ria Minawala, MD1, Henry Wu, MD2, Katherine Sun, MD2
1NYU Langone Health, New York, NY; 2New York University Langone Health, New York, NY
Introduction: Mucormycosis is a fungal infection affecting various organs; gastric mucormycosis is a rare, life-threatening disease with increasing incidence.1 Gastroenterologists should consider mucormycosis for patients with severe ulcerations and friable mucosa.
Case Description/
Methods: Mr. D is a 66y male with a past medical history of hypertension, hyperlipidemia, coronary artery disease status post stent placement, active smoker (2 packs/day), and alcohol use disorder who presented in January 2024 with abdominal pain and a 20-pound weight loss since 2023 with loss of appetite and left leg swelling. CT abdomen pelvis with oral and IV contrast showed diffuse enterocolitis with small bowel perforation, interloop abdominopelvic abscesses, pneumoperitoneum and small volume ascites, with concurrent findings of deep venous thrombosis in left external iliac vein and common femoral vein. He received extensive surgery involving small bowel resection, sigmoidectomy, small bowel anastomosis, and end colostomy. Several days after surgery, he developed melena and an acute hemoglobin drop from 7 to 6g/dL. Despite an initial upper endoscopy achieving hemostasis of a pigmented lesion with pulsatile flow near a gastric ulcer, he continued to have melena and hemoglobin drop requiring transfusions. Repeat EGD showed multiple non-obstructing, cratered gastric ulcers with adherent clot (Forrest Class IIb) in the cardia and fundus, with friable tissue oozing on contact with scope (Figure 1). Stomach ulcer biopsy with Grocott Methenamine Silver stain revealed mucor species with tissue invasion, ulceration, and granulomatous and giant cell reaction. He received 8 weeks of antifungal therapy and gradually improved.
Discussion: Gastric mucormycosis, associated with high mortality, usually presents with abdominal pain, distension, and gastrointestinal bleeding depending on the involved site.1 Tissue diagnosis via endoscopic biopsy is key to early recognition. Endoscopic findings include ulcers, thrombosis of adjacent vessels, and hemorrhagic, edematous mucosa. In this case, his low oral intake and significant weight loss likely contributed to his immunocompromised state. Treatment requires both antifungal therapy and surgical debulking; antifungal therapy alone is usually insufficient.1 Gastroenterologists should have a high degree of suspicion of mucormycosis among patients with similar presentations.
1. Yazan Addasi, et al. Gastrointestinal Mucormycosis: A Clinical Review. Gastroenterology Research, 2023, 16(5), 249–253.
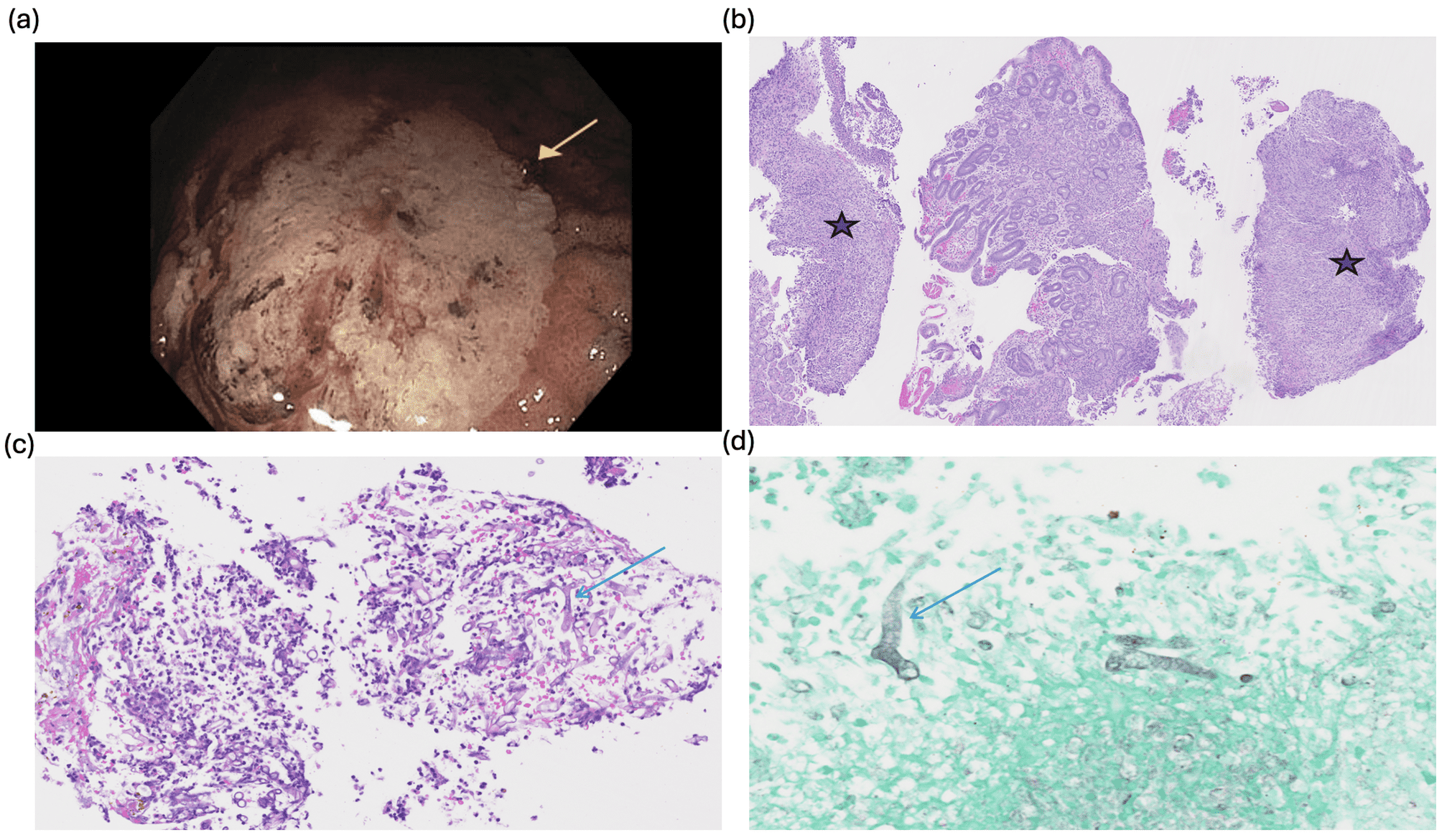
Figure: Figure 1. Endoscopic Image and Tissue Biopsy of Gastric Ulcer. (a) Gastric Ulcer on EGD. (b) Hematoxylin and eosin stain (H&E), 40X: the tissue fragments with * show ulceration. (c) Hematoxylin and eosin stain, 200X: nonseptate widely branching hyphal elements infiltrating tissue. (d) Grocott methenamine silver stain (GMS) reveals mucor organisms as broad, irregular hyphae in tissue.
Disclosures:
Angela Xue indicated no relevant financial relationships.
Ria Minawala indicated no relevant financial relationships.
Henry Wu indicated no relevant financial relationships.
Katherine Sun indicated no relevant financial relationships.
Angela Xue, MD1, Ria Minawala, MD1, Henry Wu, MD2, Katherine Sun, MD2. P1323 - Black Fungus Ulcer: A Case of Severe Gastric Mucormycosis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1NYU Langone Health, New York, NY; 2New York University Langone Health, New York, NY
Introduction: Mucormycosis is a fungal infection affecting various organs; gastric mucormycosis is a rare, life-threatening disease with increasing incidence.1 Gastroenterologists should consider mucormycosis for patients with severe ulcerations and friable mucosa.
Case Description/
Methods: Mr. D is a 66y male with a past medical history of hypertension, hyperlipidemia, coronary artery disease status post stent placement, active smoker (2 packs/day), and alcohol use disorder who presented in January 2024 with abdominal pain and a 20-pound weight loss since 2023 with loss of appetite and left leg swelling. CT abdomen pelvis with oral and IV contrast showed diffuse enterocolitis with small bowel perforation, interloop abdominopelvic abscesses, pneumoperitoneum and small volume ascites, with concurrent findings of deep venous thrombosis in left external iliac vein and common femoral vein. He received extensive surgery involving small bowel resection, sigmoidectomy, small bowel anastomosis, and end colostomy. Several days after surgery, he developed melena and an acute hemoglobin drop from 7 to 6g/dL. Despite an initial upper endoscopy achieving hemostasis of a pigmented lesion with pulsatile flow near a gastric ulcer, he continued to have melena and hemoglobin drop requiring transfusions. Repeat EGD showed multiple non-obstructing, cratered gastric ulcers with adherent clot (Forrest Class IIb) in the cardia and fundus, with friable tissue oozing on contact with scope (Figure 1). Stomach ulcer biopsy with Grocott Methenamine Silver stain revealed mucor species with tissue invasion, ulceration, and granulomatous and giant cell reaction. He received 8 weeks of antifungal therapy and gradually improved.
Discussion: Gastric mucormycosis, associated with high mortality, usually presents with abdominal pain, distension, and gastrointestinal bleeding depending on the involved site.1 Tissue diagnosis via endoscopic biopsy is key to early recognition. Endoscopic findings include ulcers, thrombosis of adjacent vessels, and hemorrhagic, edematous mucosa. In this case, his low oral intake and significant weight loss likely contributed to his immunocompromised state. Treatment requires both antifungal therapy and surgical debulking; antifungal therapy alone is usually insufficient.1 Gastroenterologists should have a high degree of suspicion of mucormycosis among patients with similar presentations.
1. Yazan Addasi, et al. Gastrointestinal Mucormycosis: A Clinical Review. Gastroenterology Research, 2023, 16(5), 249–253.
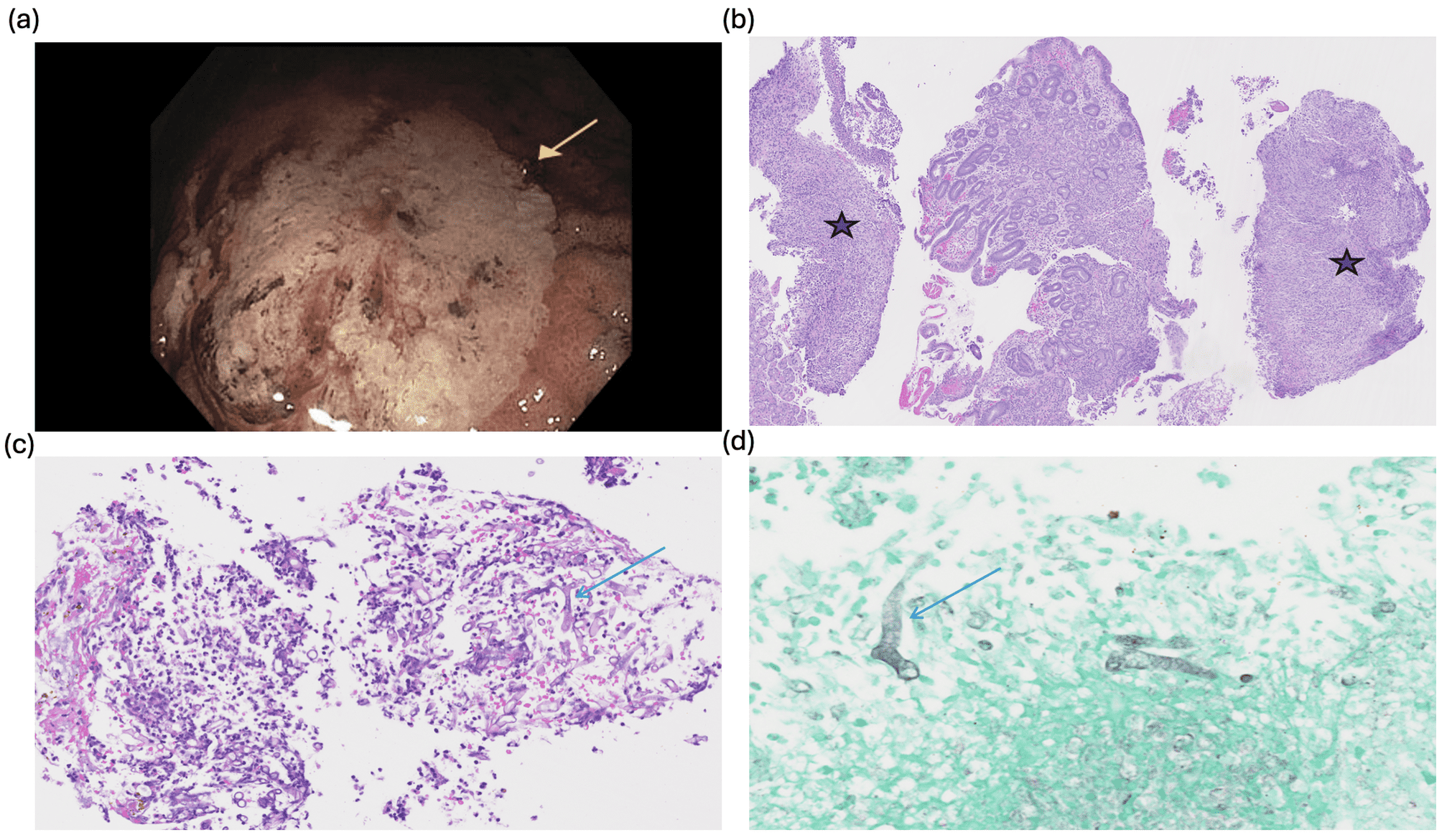
Figure: Figure 1. Endoscopic Image and Tissue Biopsy of Gastric Ulcer. (a) Gastric Ulcer on EGD. (b) Hematoxylin and eosin stain (H&E), 40X: the tissue fragments with * show ulceration. (c) Hematoxylin and eosin stain, 200X: nonseptate widely branching hyphal elements infiltrating tissue. (d) Grocott methenamine silver stain (GMS) reveals mucor organisms as broad, irregular hyphae in tissue.
Disclosures:
Angela Xue indicated no relevant financial relationships.
Ria Minawala indicated no relevant financial relationships.
Henry Wu indicated no relevant financial relationships.
Katherine Sun indicated no relevant financial relationships.
Angela Xue, MD1, Ria Minawala, MD1, Henry Wu, MD2, Katherine Sun, MD2. P1323 - Black Fungus Ulcer: A Case of Severe Gastric Mucormycosis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
