Sunday Poster Session
Category: Infections and Microbiome
P1320 - From Lips to Lumen: A Curious Case of Herpetic Esophagogastritis
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall

Joshika Agarwal, MD (she/her/hers)
Mercy Catholic Medical Center
Darby, PA
Presenting Author(s)
Joshika Agarwal, MD, Dhruvan Patel, MD
Mercy Catholic Medical Center, Darby, PA
Introduction: Herpes Simplex Virus (HSV-1), commonly recognized as a culprit for sexually transmitted infections, is an uncommon cause of peptic ulcer disease, particularly in immunocompetent people. It clinically presents as postprandial epigastric pain, nausea, vomiting, anemia, and hematochezia. This case report describes a HSV-1-related esophagogasritis in a patient with a vague presentation.
Case Description/
Methods: A 64-year-old male with a history of hypertension presented with diarrhea consisting of 2-3 daily episodes of loose watery, easy to flush stools over the past two months with associated weight loss and desquamative rash on palms, elbows, feet, knees, and face. No history of abdominal pain, nausea or vomiting, fever, chills, change in appetite, melena, or hematochezia was reported. The admission vitals, abdominal examination and CT imaging were unremarkable. Labs were notable for microcytic anemia with mild leukocytosis. Calculated stool gap of 36 was concerning for secretary diarrhea with a negative HIV test, Celiac panel and stool studies. Pancreatic elastase levels were low and the patient was initiated on oral pancreatic enzyme supplementation for suspected moderate pancreatic insufficiency. Later in the hospital course, the patient developed intermittent fever and mild icterus with a distended abdomen. Repeat CT abdomen confirmed hepatosplenomegaly with retroperitoneal lymph node enlargement. Given ongoing diarrhea, he underwent an upper gastrointestinal (GI) endoscopy with biopsy which showed necrotic debris with atypical cells containing herpetic-type inclusions involving gastric fundus and body as shown in Figure 1 and 2 respectively.
Discussion: Few studies in the past have shown association between HSV-1 and esophagitis or gastritis. HSV-1 esophagitis with concomitant duodenitis in a healthy individual is, however, rare as seen in our case. It is typically confirmed with endoscopic biopsy, histopathology and immnohistochemistry to rule out other etiology including Helicobacter pylori gastritis which was negative in our patient. Management is often conservative with repeat endoscopy to ensure complete healing. The patient was discharged on oral valacyclovir 1g twice daily prescribed for ten days with pantoprazole twice daily for four weeks and sucralfate 1g four times daily for two weeks. This case emphasizes the significance of considering HSV-1 infection as one of the differential diagnoses when approaching a patient with similar GI symptoms.
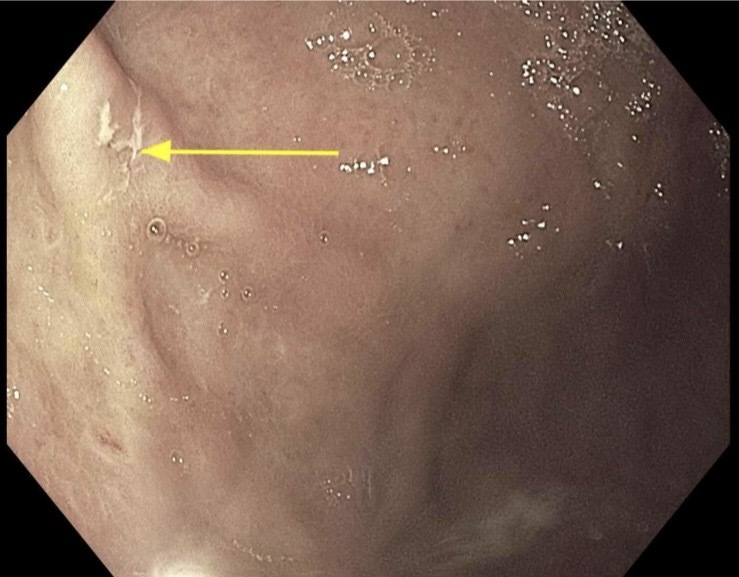
Figure: Endoscopic image of superficial non bleeding Gastric Body Ulcer measuring 4 mm in largest dimensions
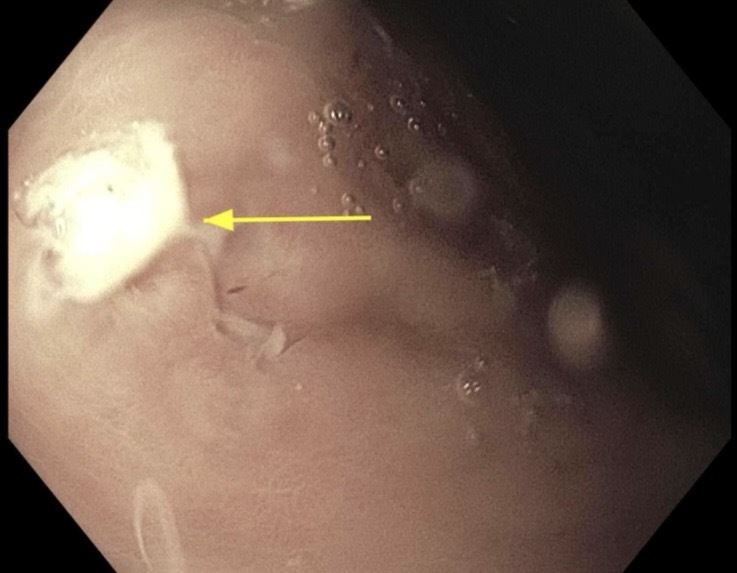
Figure: Endoscopic image of superficial non bleeding Gastric Fundus Ulcer measuring approximately 6 mm in largest dimensions
Disclosures:
Joshika Agarwal indicated no relevant financial relationships.
Dhruvan Patel indicated no relevant financial relationships.
Joshika Agarwal, MD, Dhruvan Patel, MD. P1320 - From Lips to Lumen: A Curious Case of Herpetic Esophagogastritis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
Mercy Catholic Medical Center, Darby, PA
Introduction: Herpes Simplex Virus (HSV-1), commonly recognized as a culprit for sexually transmitted infections, is an uncommon cause of peptic ulcer disease, particularly in immunocompetent people. It clinically presents as postprandial epigastric pain, nausea, vomiting, anemia, and hematochezia. This case report describes a HSV-1-related esophagogasritis in a patient with a vague presentation.
Case Description/
Methods: A 64-year-old male with a history of hypertension presented with diarrhea consisting of 2-3 daily episodes of loose watery, easy to flush stools over the past two months with associated weight loss and desquamative rash on palms, elbows, feet, knees, and face. No history of abdominal pain, nausea or vomiting, fever, chills, change in appetite, melena, or hematochezia was reported. The admission vitals, abdominal examination and CT imaging were unremarkable. Labs were notable for microcytic anemia with mild leukocytosis. Calculated stool gap of 36 was concerning for secretary diarrhea with a negative HIV test, Celiac panel and stool studies. Pancreatic elastase levels were low and the patient was initiated on oral pancreatic enzyme supplementation for suspected moderate pancreatic insufficiency. Later in the hospital course, the patient developed intermittent fever and mild icterus with a distended abdomen. Repeat CT abdomen confirmed hepatosplenomegaly with retroperitoneal lymph node enlargement. Given ongoing diarrhea, he underwent an upper gastrointestinal (GI) endoscopy with biopsy which showed necrotic debris with atypical cells containing herpetic-type inclusions involving gastric fundus and body as shown in Figure 1 and 2 respectively.
Discussion: Few studies in the past have shown association between HSV-1 and esophagitis or gastritis. HSV-1 esophagitis with concomitant duodenitis in a healthy individual is, however, rare as seen in our case. It is typically confirmed with endoscopic biopsy, histopathology and immnohistochemistry to rule out other etiology including Helicobacter pylori gastritis which was negative in our patient. Management is often conservative with repeat endoscopy to ensure complete healing. The patient was discharged on oral valacyclovir 1g twice daily prescribed for ten days with pantoprazole twice daily for four weeks and sucralfate 1g four times daily for two weeks. This case emphasizes the significance of considering HSV-1 infection as one of the differential diagnoses when approaching a patient with similar GI symptoms.
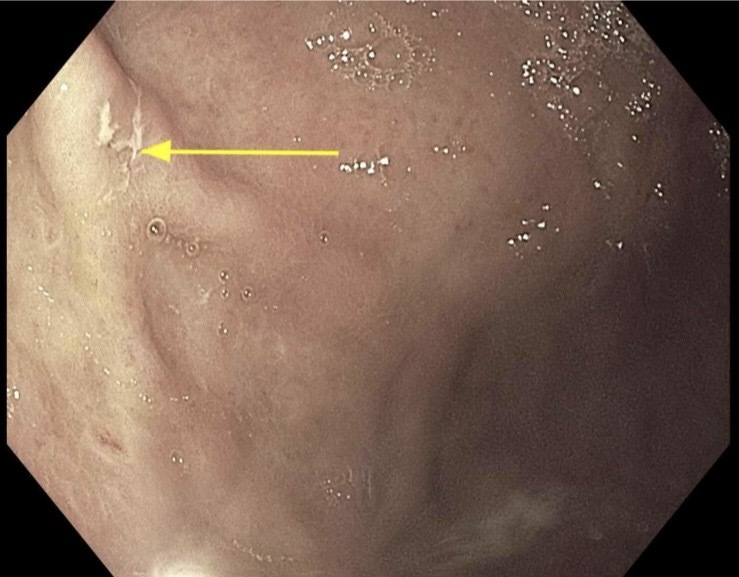
Figure: Endoscopic image of superficial non bleeding Gastric Body Ulcer measuring 4 mm in largest dimensions
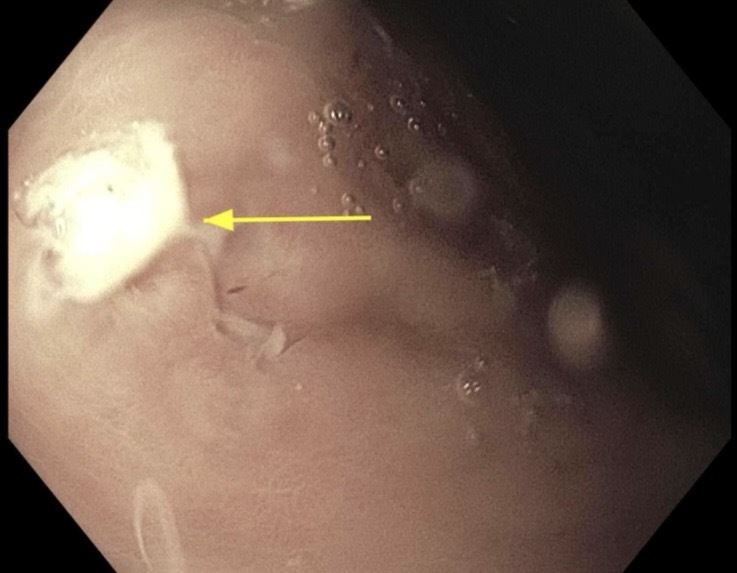
Figure: Endoscopic image of superficial non bleeding Gastric Fundus Ulcer measuring approximately 6 mm in largest dimensions
Disclosures:
Joshika Agarwal indicated no relevant financial relationships.
Dhruvan Patel indicated no relevant financial relationships.
Joshika Agarwal, MD, Dhruvan Patel, MD. P1320 - From Lips to Lumen: A Curious Case of Herpetic Esophagogastritis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
