Sunday Poster Session
Category: Interventional Endoscopy
P1393 - Submucosal Injection versus Non-Injection Technique in Endoscopic Papillectomy: A Systematic Review and Meta-Analysis of Efficacy and Safety Outcomes
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall
Rami Musallam, MD
Carilion Clinic, VA
Presenting Author(s)
Rami Musallam, MD1, Abbinaya Elangovan, MD1, Mohammad Aldiabat, MD2, Jay Bapaye, MD1, Subhash Garikipati, MD1, William Abel, MD3, Andrew Canakis, DO4, Mohannad Abousaleh, MD5, Paul Yeaton, MD3, Patrick Okolo, MD3, Klaus Monkemuller, MD3, Vivek Kesar, MD3, Varun Kesar, MD6
1Carilion Clinic, Roanoke, VA; 2Washington University School of Medicine in St. Louis, St. Louis, MO; 3CARILION CLINIC, Roanoke, VA; 4Unc chapel hill, Bishopville, MD; 5Huron Gastro Ann Arbor, Ypsilanti, MI; 6Virginia Tech Carilion School of Medicine, Roanoke, VA
Introduction: The utility of submucosal injection (SI) in endoscopic papillectomy (EP) remains debated. This meta-analysis compares outcomes between SI and non-injection (NI) techniques.
Methods: A systematic search of PubMed, Scopus, and Web of Science (through May 2025) identified studies comparing SI and NI in EP. Primary outcomes included technical success, en bloc resection, and complete (R0) resection. Secondary outcomes were recurrence/residual disease and adverse events (AEs). A random-effects model was used; heterogeneity was assessed via the I² statistic.SI: submucosal injection. NI: non-injection
Results: Forty-six studies (3 RCTs, 5 prospective, 38 retrospective) comprising 461 SI and 1,868 NI patients were included. The mean age was 61.6 years; 48.7% were female. Lesion size averaged 17.3 mm (SI) vs. 18.8 mm (NI), with mean follow-up of 30.2 months. Technical success was 93.5% (95% CI: 87.5–96.7; I² = 58.1) in SI vs. 97.4% (95.6–98.5; I² = 63.8) in NI. En bloc resection was 84.7% (72.0–92.3; I² = 83.4) in SI and 88.5% (84.9–91.2; I² = 54.8) in NI; RCTs showed 91.7% (83.0–96.1; I² = 0) for NI. Complete (R0) resection was higher in SI (89.0%; 73.2–96.0; I² = 81.5) vs. NI (72.2%; 64.4–79.0; I² = 87.4); in RCTs, NI had 83.0% (72.4–90.1; I² = 0). Recurrence/residual tumor rates were similar: 15.7% (10.8–22.4; I² = 45.5) in SI vs. 15.4% (11.9–19.7; I² = 73.2) in NI. Mean time to recurrence was ~14.2 months. Overall AEs were 32.2% (22.3–43.9; I² = 70.2) in SI vs. 29.9% (23.0–37.9; I² = 87.3) in NI. Pancreatitis occurred in 10.5% (5.6–18.7; I² = 71.7) of SI cases, reduced to 7.8% (4.1–14.2; I² = 0) with stenting. In NI, pancreatitis was 12.3% (9.9–15.2; I² = 58.2), reduced to 10.9% (6.2–18.7; I² = 69.5) with stenting. Bleeding was higher in SI (22.7%; 14.5–33.8; I² = 78.1) vs. NI (14.2%; 10.4–19.1; I² = 83.6). Perforation was 5.1% (3.3–7.7; I² = 0) in SI and 2.6% (1.9–3.6; I² = 0) in NI (Table1).
Discussion: While SI improves R0 resection rates, it does not significantly enhance en bloc resection, technical success, or recurrence rates. Moreover, SI is associated with increased bleeding and perforation risk. Pancreatitis rates are similar and can be reduced with prophylactic stenting. The NI technique offers comparable efficacy with a more favorable safety profile in selected patients. Further high-quality RCTs are warranted to confirm these findings and inform procedural strategy.
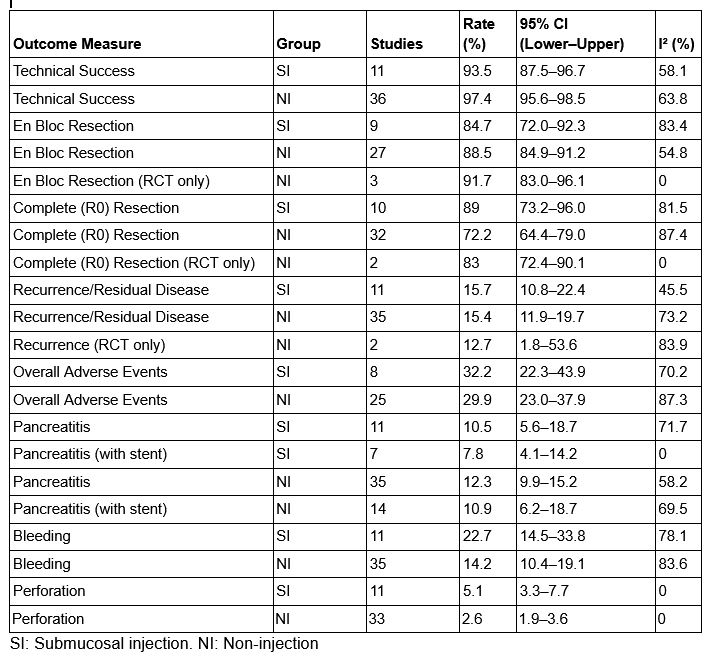
Figure: Table 1: summary of pooled rates
Disclosures:
Rami Musallam indicated no relevant financial relationships.
Abbinaya Elangovan indicated no relevant financial relationships.
Mohammad Aldiabat indicated no relevant financial relationships.
Jay Bapaye indicated no relevant financial relationships.
Subhash Garikipati indicated no relevant financial relationships.
William Abel indicated no relevant financial relationships.
Andrew Canakis indicated no relevant financial relationships.
Mohannad Abousaleh indicated no relevant financial relationships.
Paul Yeaton indicated no relevant financial relationships.
Patrick Okolo indicated no relevant financial relationships.
Klaus Monkemuller indicated no relevant financial relationships.
Vivek Kesar indicated no relevant financial relationships.
Varun Kesar indicated no relevant financial relationships.
Rami Musallam, MD1, Abbinaya Elangovan, MD1, Mohammad Aldiabat, MD2, Jay Bapaye, MD1, Subhash Garikipati, MD1, William Abel, MD3, Andrew Canakis, DO4, Mohannad Abousaleh, MD5, Paul Yeaton, MD3, Patrick Okolo, MD3, Klaus Monkemuller, MD3, Vivek Kesar, MD3, Varun Kesar, MD6. P1393 - Submucosal Injection versus Non-Injection Technique in Endoscopic Papillectomy: A Systematic Review and Meta-Analysis of Efficacy and Safety Outcomes, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Carilion Clinic, Roanoke, VA; 2Washington University School of Medicine in St. Louis, St. Louis, MO; 3CARILION CLINIC, Roanoke, VA; 4Unc chapel hill, Bishopville, MD; 5Huron Gastro Ann Arbor, Ypsilanti, MI; 6Virginia Tech Carilion School of Medicine, Roanoke, VA
Introduction: The utility of submucosal injection (SI) in endoscopic papillectomy (EP) remains debated. This meta-analysis compares outcomes between SI and non-injection (NI) techniques.
Methods: A systematic search of PubMed, Scopus, and Web of Science (through May 2025) identified studies comparing SI and NI in EP. Primary outcomes included technical success, en bloc resection, and complete (R0) resection. Secondary outcomes were recurrence/residual disease and adverse events (AEs). A random-effects model was used; heterogeneity was assessed via the I² statistic.SI: submucosal injection. NI: non-injection
Results: Forty-six studies (3 RCTs, 5 prospective, 38 retrospective) comprising 461 SI and 1,868 NI patients were included. The mean age was 61.6 years; 48.7% were female. Lesion size averaged 17.3 mm (SI) vs. 18.8 mm (NI), with mean follow-up of 30.2 months. Technical success was 93.5% (95% CI: 87.5–96.7; I² = 58.1) in SI vs. 97.4% (95.6–98.5; I² = 63.8) in NI. En bloc resection was 84.7% (72.0–92.3; I² = 83.4) in SI and 88.5% (84.9–91.2; I² = 54.8) in NI; RCTs showed 91.7% (83.0–96.1; I² = 0) for NI. Complete (R0) resection was higher in SI (89.0%; 73.2–96.0; I² = 81.5) vs. NI (72.2%; 64.4–79.0; I² = 87.4); in RCTs, NI had 83.0% (72.4–90.1; I² = 0). Recurrence/residual tumor rates were similar: 15.7% (10.8–22.4; I² = 45.5) in SI vs. 15.4% (11.9–19.7; I² = 73.2) in NI. Mean time to recurrence was ~14.2 months. Overall AEs were 32.2% (22.3–43.9; I² = 70.2) in SI vs. 29.9% (23.0–37.9; I² = 87.3) in NI. Pancreatitis occurred in 10.5% (5.6–18.7; I² = 71.7) of SI cases, reduced to 7.8% (4.1–14.2; I² = 0) with stenting. In NI, pancreatitis was 12.3% (9.9–15.2; I² = 58.2), reduced to 10.9% (6.2–18.7; I² = 69.5) with stenting. Bleeding was higher in SI (22.7%; 14.5–33.8; I² = 78.1) vs. NI (14.2%; 10.4–19.1; I² = 83.6). Perforation was 5.1% (3.3–7.7; I² = 0) in SI and 2.6% (1.9–3.6; I² = 0) in NI (Table1).
Discussion: While SI improves R0 resection rates, it does not significantly enhance en bloc resection, technical success, or recurrence rates. Moreover, SI is associated with increased bleeding and perforation risk. Pancreatitis rates are similar and can be reduced with prophylactic stenting. The NI technique offers comparable efficacy with a more favorable safety profile in selected patients. Further high-quality RCTs are warranted to confirm these findings and inform procedural strategy.
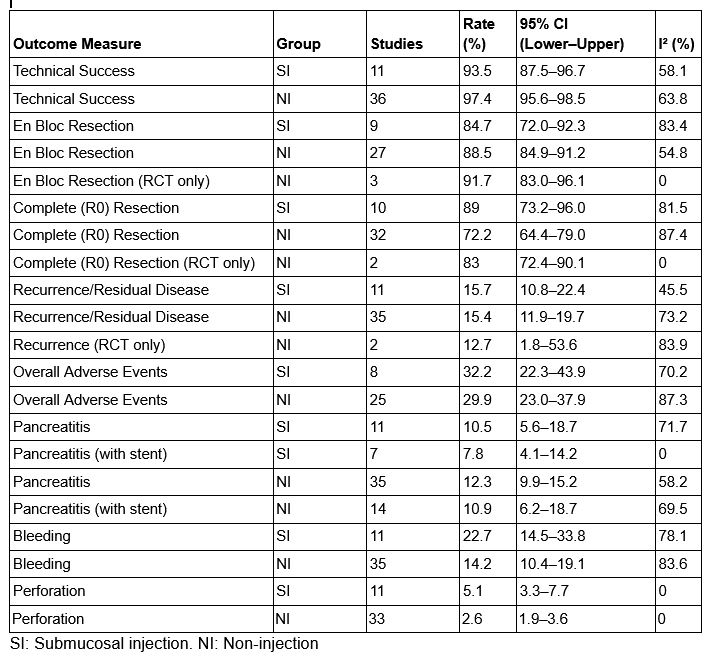
Figure: Table 1: summary of pooled rates
Disclosures:
Rami Musallam indicated no relevant financial relationships.
Abbinaya Elangovan indicated no relevant financial relationships.
Mohammad Aldiabat indicated no relevant financial relationships.
Jay Bapaye indicated no relevant financial relationships.
Subhash Garikipati indicated no relevant financial relationships.
William Abel indicated no relevant financial relationships.
Andrew Canakis indicated no relevant financial relationships.
Mohannad Abousaleh indicated no relevant financial relationships.
Paul Yeaton indicated no relevant financial relationships.
Patrick Okolo indicated no relevant financial relationships.
Klaus Monkemuller indicated no relevant financial relationships.
Vivek Kesar indicated no relevant financial relationships.
Varun Kesar indicated no relevant financial relationships.
Rami Musallam, MD1, Abbinaya Elangovan, MD1, Mohammad Aldiabat, MD2, Jay Bapaye, MD1, Subhash Garikipati, MD1, William Abel, MD3, Andrew Canakis, DO4, Mohannad Abousaleh, MD5, Paul Yeaton, MD3, Patrick Okolo, MD3, Klaus Monkemuller, MD3, Vivek Kesar, MD3, Varun Kesar, MD6. P1393 - Submucosal Injection versus Non-Injection Technique in Endoscopic Papillectomy: A Systematic Review and Meta-Analysis of Efficacy and Safety Outcomes, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
