Sunday Poster Session
Category: Interventional Endoscopy
P1381 - Lumen-Apposing Metal Stents for Partial Reversal of Roux-en-Y Gastric Bypass: A Multicenter Study
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall
- AH
Azhar Hussain, MBBS
SUNY Upstate Medical University Hospital
Syracuse, NY
Presenting Author(s)
Azhar Hussain, MBBS1, Kambiz Khadkhodayan, MD2, Mohamad Khaled Almujarkesh, MD2, Saurabh Chandan, MD3, Sagar J.. Pathak, MD3, Abdullah Abassi, MD2, Artur Viana, MD2, Gustavo Bellovincentelli, MD2, Mustafa Arain, MD3, Natalie Cosgrove, MD3, Zubair Khan, MD4, Maham Hayat, MD3, Deepanshu Jain, MD3, Muhammad Usman Baig, MBBS5, Dushyant S. Dahiya, MD6, Dennis Yang, MD, FACG7, Mohammad Bilal, MD, FACG8, Reem Z.. Sharaiha, MD, MSc5, Muhammad Hasan, MD, FACG3, Shayan S. Irani, MD9
1SUNY Upstate Medical University Hospital, Syracuse, NY; 2AdventHealth, Orlando, FL; 3Center for Interventional Endoscopy, AdventHealth Orlando, Orlando, FL; 4Mercy Clinic East Communities, Festus, MO; 5Weill Cornell Medical College, New York, NY; 6University of Kansas School of Medicine, Kansas City, KS; 7Center for Interventional Endoscopic, AdventHealth Orlando, Orlando, FL; 8University of Colorado Anschutz Medical Campus, Denver, CO; 9Virginia Mason Medical Center, Seattle, WA
Introduction: Roux-en-Y gastric bypass (RYGB) is an effective treatment of obesity, however, some patients will develop debilitating nutritional and metabolic post-operative complications requiring surgical reversal that can be technically challenging and highly morbid (up to 50%). Partial re-direction of food into the native stomach via GG fistula by LAMS may result in improvement of nutritional status and may serve either as a bridge to surgery or as definitive therapy.
Methods: We report a prospective series of 16 patients with complications related to RYGB, from four tertiary care centers, who underwent EUS-guided LAMS placement and creation of a GG fistula due to either severe protein-calorie malnutrition, dumping syndrome, or postprandial hyperinsulinemic hypoglycemia.
Results: Technical and clinical success was achieved in 16 patients (100%) and 15 patients (93.75%) respectively. Mean body mass index increased significantly from the time of placement of LAMS to mean follow-up of 15.8 months (range 3-62), 21.2 kg/m² to 24.4 kg/m², (Mean Difference (MD): 3.19, P=0.005) (Table 1). In patients with benign disease, the mean change in % total body weight (TBW) was 13.4% at 3-6 month follow-up. Additionally, there was a significant increase in mean hemoglobin levels at follow-up, 10.4 g/dl to 11.6 g/dl, (MD: 1.22, P=0.02). The mean serum albumin increased from a mean of 2.61 g/dl to 3.51 g/dl (MD: 0.89, P< 0.001) at 3 months. LAMS-related complications occurred in 3 patients and included pain, tissue ingrowth, and stent migration and all managed endoscopically (Figure 1).
Discussion: Our study supports the safety, feasibility, and efficacy of EUS-guided LAMS placement for partial reversal of RYGB. For patients with severe protein-calorie malnutrition or nutrient deficiency, creation of GG fistula via LAMS between the gastric pouch and the excluded stomach resulted in improvement in weight and various nutritional parameters due to diversion of chyme into the excluded stomach and duodenum, increasing the absorption and bioavailability of macro and micronutrients.
In patients with dumping syndrome and post-prandial hypoglycemia, creation of a GG fistula via LAMS probably resulted in more controlled and lower-volume nutrient delivery into the afferent limb and thus significant clinical improvement in symptoms.
EUS-guided LAMS placement is a safe, efficacious, and minimally invasive strategy for partial reversal of RYGB as either a bridge to definitive surgical reversal or as destination therapy.
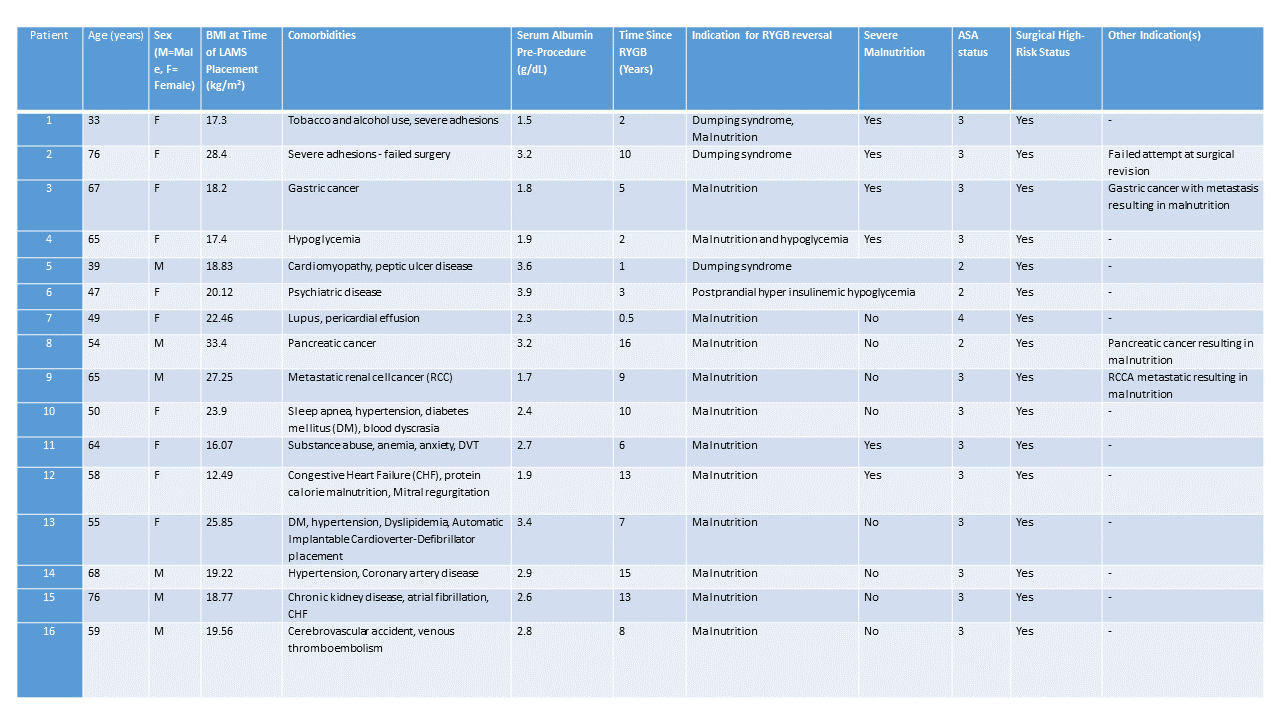
Figure: Table 1 – Patient Characteristics
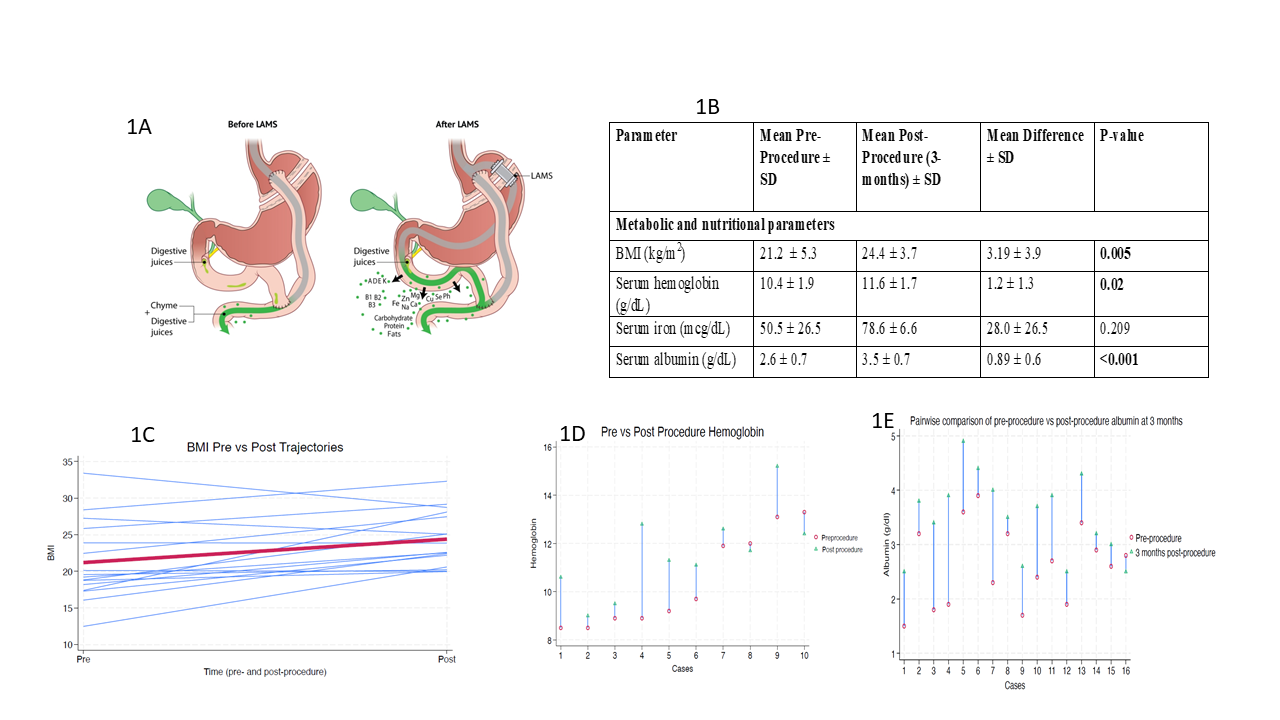
Figure: Figure 1: (A) Illustration demonstrating standard RYGB anatomy (left) and partial reversal of RYGB with the use of a gastro-gastric LAMS (right). Note that in the image on the right, the nutrient rich stream of chyme is partially shunted towards the excluded stomach, duodenum and biliopancreatic limb, where it mixes with digestive juices. (B) Summary of Metabolic and Nutritional Parameters Pre-Procedure and Post-Procedure at 3-Months. (C) Trends of pre- and post-procedure BMI. (D) Trends of Trends of pre- and post-procedure hemoglobin. (E) Trends of pre- and post-procedure albumin
Disclosures:
Azhar Hussain indicated no relevant financial relationships.
Kambiz Khadkhodayan indicated no relevant financial relationships.
Mohamad Khaled Almujarkesh indicated no relevant financial relationships.
Saurabh Chandan indicated no relevant financial relationships.
Sagar Pathak indicated no relevant financial relationships.
Abdullah Abassi indicated no relevant financial relationships.
Artur Viana indicated no relevant financial relationships.
Gustavo Bellovincentelli indicated no relevant financial relationships.
Mustafa Arain: Boston Scientific – Consultant. Cook Endoscopy – Consultant. Olympus – Consultant.
Natalie Cosgrove indicated no relevant financial relationships.
Zubair Khan indicated no relevant financial relationships.
Maham Hayat indicated no relevant financial relationships.
Deepanshu Jain indicated no relevant financial relationships.
Muhammad Usman Baig indicated no relevant financial relationships.
Dushyant Dahiya indicated no relevant financial relationships.
Dennis Yang: 3D-Matrix – Consultant. Apollo Endosurgery – Consultant. ERBE – Consultant. Fujifilm – Consultant. Medtronic – Consultant. MicroTech – Consultant. Olympus – Consultant.
Mohammad Bilal: Boston Scientific – Consultant. Cook endoscopy – Paid speaker. Steris Endoscopy – Consultant.
Reem Sharaiha: Boston Scientific – Consultant. Cook Medical – Consultant. Olympus – Consultant. Surgical Intuitive – Consultant.
Muhammad Hasan: Boston Scientific – Consultant. MicroTech Endoscopy – Consultant. Olympus America – Consultant.
Shayan Irani: Boston Scientific – Consultant. ConMed – Consultant. W.L. Gore – Consultant.
Azhar Hussain, MBBS1, Kambiz Khadkhodayan, MD2, Mohamad Khaled Almujarkesh, MD2, Saurabh Chandan, MD3, Sagar J.. Pathak, MD3, Abdullah Abassi, MD2, Artur Viana, MD2, Gustavo Bellovincentelli, MD2, Mustafa Arain, MD3, Natalie Cosgrove, MD3, Zubair Khan, MD4, Maham Hayat, MD3, Deepanshu Jain, MD3, Muhammad Usman Baig, MBBS5, Dushyant S. Dahiya, MD6, Dennis Yang, MD, FACG7, Mohammad Bilal, MD, FACG8, Reem Z.. Sharaiha, MD, MSc5, Muhammad Hasan, MD, FACG3, Shayan S. Irani, MD9. P1381 - Lumen-Apposing Metal Stents for Partial Reversal of Roux-en-Y Gastric Bypass: A Multicenter Study, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1SUNY Upstate Medical University Hospital, Syracuse, NY; 2AdventHealth, Orlando, FL; 3Center for Interventional Endoscopy, AdventHealth Orlando, Orlando, FL; 4Mercy Clinic East Communities, Festus, MO; 5Weill Cornell Medical College, New York, NY; 6University of Kansas School of Medicine, Kansas City, KS; 7Center for Interventional Endoscopic, AdventHealth Orlando, Orlando, FL; 8University of Colorado Anschutz Medical Campus, Denver, CO; 9Virginia Mason Medical Center, Seattle, WA
Introduction: Roux-en-Y gastric bypass (RYGB) is an effective treatment of obesity, however, some patients will develop debilitating nutritional and metabolic post-operative complications requiring surgical reversal that can be technically challenging and highly morbid (up to 50%). Partial re-direction of food into the native stomach via GG fistula by LAMS may result in improvement of nutritional status and may serve either as a bridge to surgery or as definitive therapy.
Methods: We report a prospective series of 16 patients with complications related to RYGB, from four tertiary care centers, who underwent EUS-guided LAMS placement and creation of a GG fistula due to either severe protein-calorie malnutrition, dumping syndrome, or postprandial hyperinsulinemic hypoglycemia.
Results: Technical and clinical success was achieved in 16 patients (100%) and 15 patients (93.75%) respectively. Mean body mass index increased significantly from the time of placement of LAMS to mean follow-up of 15.8 months (range 3-62), 21.2 kg/m² to 24.4 kg/m², (Mean Difference (MD): 3.19, P=0.005) (Table 1). In patients with benign disease, the mean change in % total body weight (TBW) was 13.4% at 3-6 month follow-up. Additionally, there was a significant increase in mean hemoglobin levels at follow-up, 10.4 g/dl to 11.6 g/dl, (MD: 1.22, P=0.02). The mean serum albumin increased from a mean of 2.61 g/dl to 3.51 g/dl (MD: 0.89, P< 0.001) at 3 months. LAMS-related complications occurred in 3 patients and included pain, tissue ingrowth, and stent migration and all managed endoscopically (Figure 1).
Discussion: Our study supports the safety, feasibility, and efficacy of EUS-guided LAMS placement for partial reversal of RYGB. For patients with severe protein-calorie malnutrition or nutrient deficiency, creation of GG fistula via LAMS between the gastric pouch and the excluded stomach resulted in improvement in weight and various nutritional parameters due to diversion of chyme into the excluded stomach and duodenum, increasing the absorption and bioavailability of macro and micronutrients.
In patients with dumping syndrome and post-prandial hypoglycemia, creation of a GG fistula via LAMS probably resulted in more controlled and lower-volume nutrient delivery into the afferent limb and thus significant clinical improvement in symptoms.
EUS-guided LAMS placement is a safe, efficacious, and minimally invasive strategy for partial reversal of RYGB as either a bridge to definitive surgical reversal or as destination therapy.
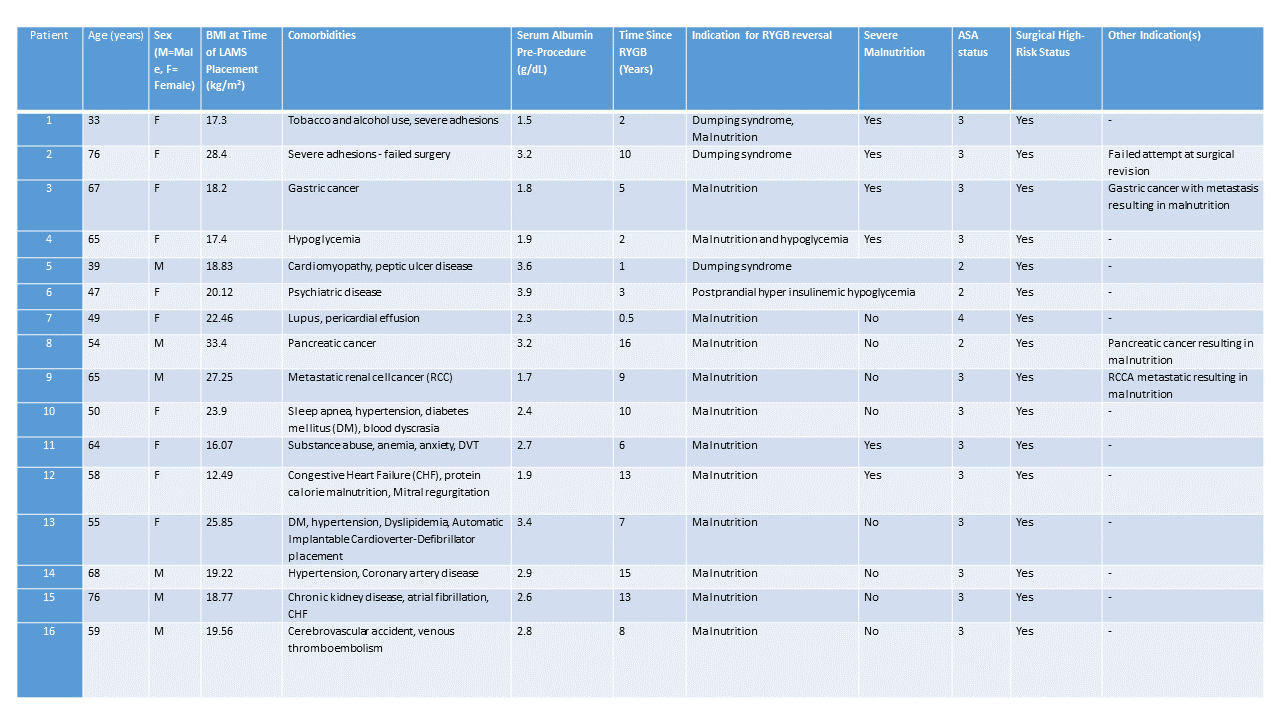
Figure: Table 1 – Patient Characteristics
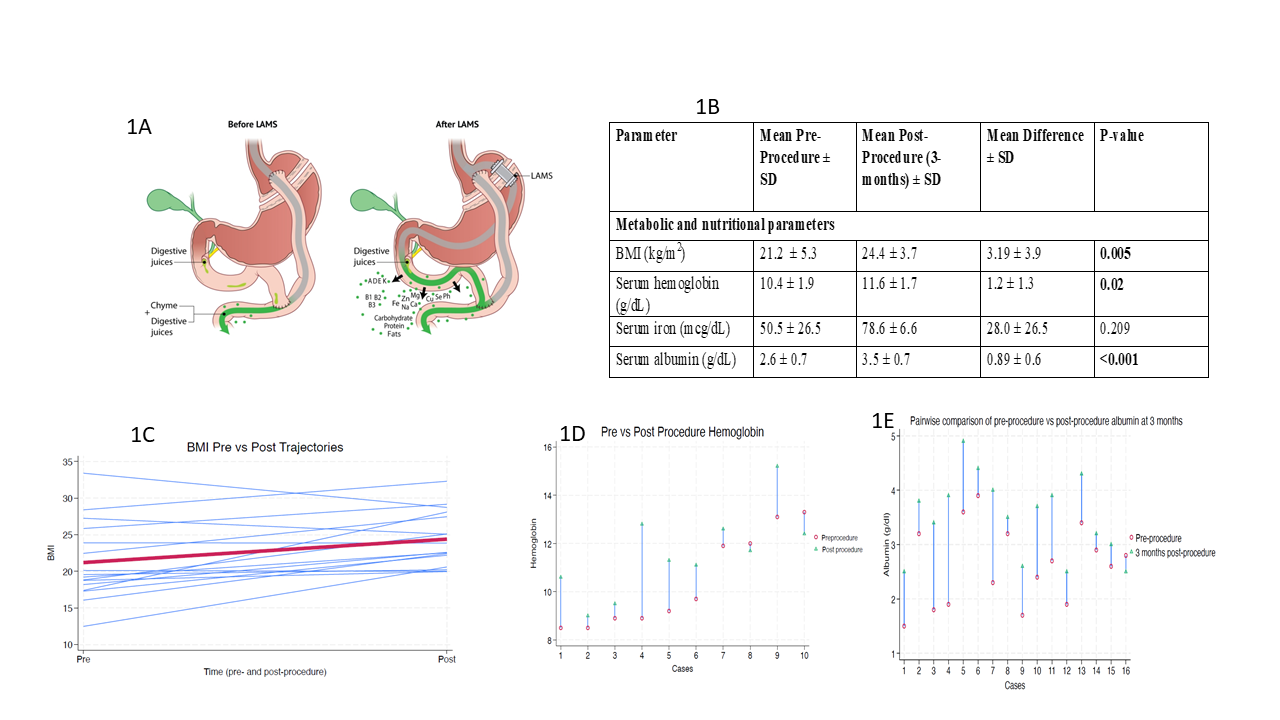
Figure: Figure 1: (A) Illustration demonstrating standard RYGB anatomy (left) and partial reversal of RYGB with the use of a gastro-gastric LAMS (right). Note that in the image on the right, the nutrient rich stream of chyme is partially shunted towards the excluded stomach, duodenum and biliopancreatic limb, where it mixes with digestive juices. (B) Summary of Metabolic and Nutritional Parameters Pre-Procedure and Post-Procedure at 3-Months. (C) Trends of pre- and post-procedure BMI. (D) Trends of Trends of pre- and post-procedure hemoglobin. (E) Trends of pre- and post-procedure albumin
Disclosures:
Azhar Hussain indicated no relevant financial relationships.
Kambiz Khadkhodayan indicated no relevant financial relationships.
Mohamad Khaled Almujarkesh indicated no relevant financial relationships.
Saurabh Chandan indicated no relevant financial relationships.
Sagar Pathak indicated no relevant financial relationships.
Abdullah Abassi indicated no relevant financial relationships.
Artur Viana indicated no relevant financial relationships.
Gustavo Bellovincentelli indicated no relevant financial relationships.
Mustafa Arain: Boston Scientific – Consultant. Cook Endoscopy – Consultant. Olympus – Consultant.
Natalie Cosgrove indicated no relevant financial relationships.
Zubair Khan indicated no relevant financial relationships.
Maham Hayat indicated no relevant financial relationships.
Deepanshu Jain indicated no relevant financial relationships.
Muhammad Usman Baig indicated no relevant financial relationships.
Dushyant Dahiya indicated no relevant financial relationships.
Dennis Yang: 3D-Matrix – Consultant. Apollo Endosurgery – Consultant. ERBE – Consultant. Fujifilm – Consultant. Medtronic – Consultant. MicroTech – Consultant. Olympus – Consultant.
Mohammad Bilal: Boston Scientific – Consultant. Cook endoscopy – Paid speaker. Steris Endoscopy – Consultant.
Reem Sharaiha: Boston Scientific – Consultant. Cook Medical – Consultant. Olympus – Consultant. Surgical Intuitive – Consultant.
Muhammad Hasan: Boston Scientific – Consultant. MicroTech Endoscopy – Consultant. Olympus America – Consultant.
Shayan Irani: Boston Scientific – Consultant. ConMed – Consultant. W.L. Gore – Consultant.
Azhar Hussain, MBBS1, Kambiz Khadkhodayan, MD2, Mohamad Khaled Almujarkesh, MD2, Saurabh Chandan, MD3, Sagar J.. Pathak, MD3, Abdullah Abassi, MD2, Artur Viana, MD2, Gustavo Bellovincentelli, MD2, Mustafa Arain, MD3, Natalie Cosgrove, MD3, Zubair Khan, MD4, Maham Hayat, MD3, Deepanshu Jain, MD3, Muhammad Usman Baig, MBBS5, Dushyant S. Dahiya, MD6, Dennis Yang, MD, FACG7, Mohammad Bilal, MD, FACG8, Reem Z.. Sharaiha, MD, MSc5, Muhammad Hasan, MD, FACG3, Shayan S. Irani, MD9. P1381 - Lumen-Apposing Metal Stents for Partial Reversal of Roux-en-Y Gastric Bypass: A Multicenter Study, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
