Sunday Poster Session
Category: Interventional Endoscopy
P1466 - Endoscopic Mucosal Defect Closure for Management of High Risk Gastric Perforation
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall

Melanie De Shadarevian, DO (she/her/hers)
Valley Hospital Medical Center
Las Vegas, NV
Presenting Author(s)
Melanie De Shadarevian, DO1, Joy-Marie Hermes, MD2, Matthew Skinner, MD3
1Valley Hospital Medical Center, Las Vegas, NV; 2Scripps Green Hospital, San Diego, CA; 3Scripps Green Hospital, La Jolla, CA
Introduction: The management of gastrointestinal (GI) tract perforations typically includes surgical repair or observation and supportive care for small low-risk perforations. Endoscopic suturing is an advanced endoscopic technique which has been implemented for achieving tissue defect closure. It has been used in fistula repairs, anastomotic leaks, peroral endoscopic myotomy, and primary sleeve gastroplasty; its use in gastrointestinal perforations has thus far been limited.
Case Description/
Methods: A 44-year old female with a history of decompensated alcoholic cirrhosis complicated by portal hypertension, variceal hemorrhage, portal vein thrombosis and deep-vein thrombosis with inferior vena cava filter presented with hematemesis and melena of one day duration. She was initially hypotensive and tachycardic with a hemoglobin of 4.0. CT of the abdomen & pelvis revealed moderate pneumoperitoneum and multiple intra-abdominal fluid collections. She was intubated, admitted to the ICU and treated supportively including placement of multiple IR drains for abscess management. Esophagogastroduodenoscopy (EGD) revealed a large antral ulcer with full-thickness perforation. Attempts were made to clip the perforation without success. She was deemed a high-risk surgical candidate and recommended palliative care as she remained critically ill. She was transferred to our facility for advanced endoscopic evaluation. Repeat endoscopy demonstrated a 5cm x 3cm near circumferential antral ulcer with perforation and purulence suggestive of peritonitis. Complete defect closure was not achieved on initial endoscopy due to the fibrotic surrounding tissue. Using a combination of endoscopic suturing and fully covered esophageal stent placement across the antrum, the defect was successfully closed after serial endoscopic treatments. Ultimately, CT confirmed defect closure without any contrast extravasation. Oral diet was gradually advanced and the patient was discharged home in stable condition. Two month follow-up EGD demonstrated normal appearing gastric mucosa with no evidence of ongoing perforation nor fistulization at which time the stent was removed.
Discussion: Management of GI tract perforations has classically been supportive/non-operative or surgical. This case demonstrates the utility of minimally invasive endoscopic techniques for management of complex luminal perforations in an appropriate candidate.
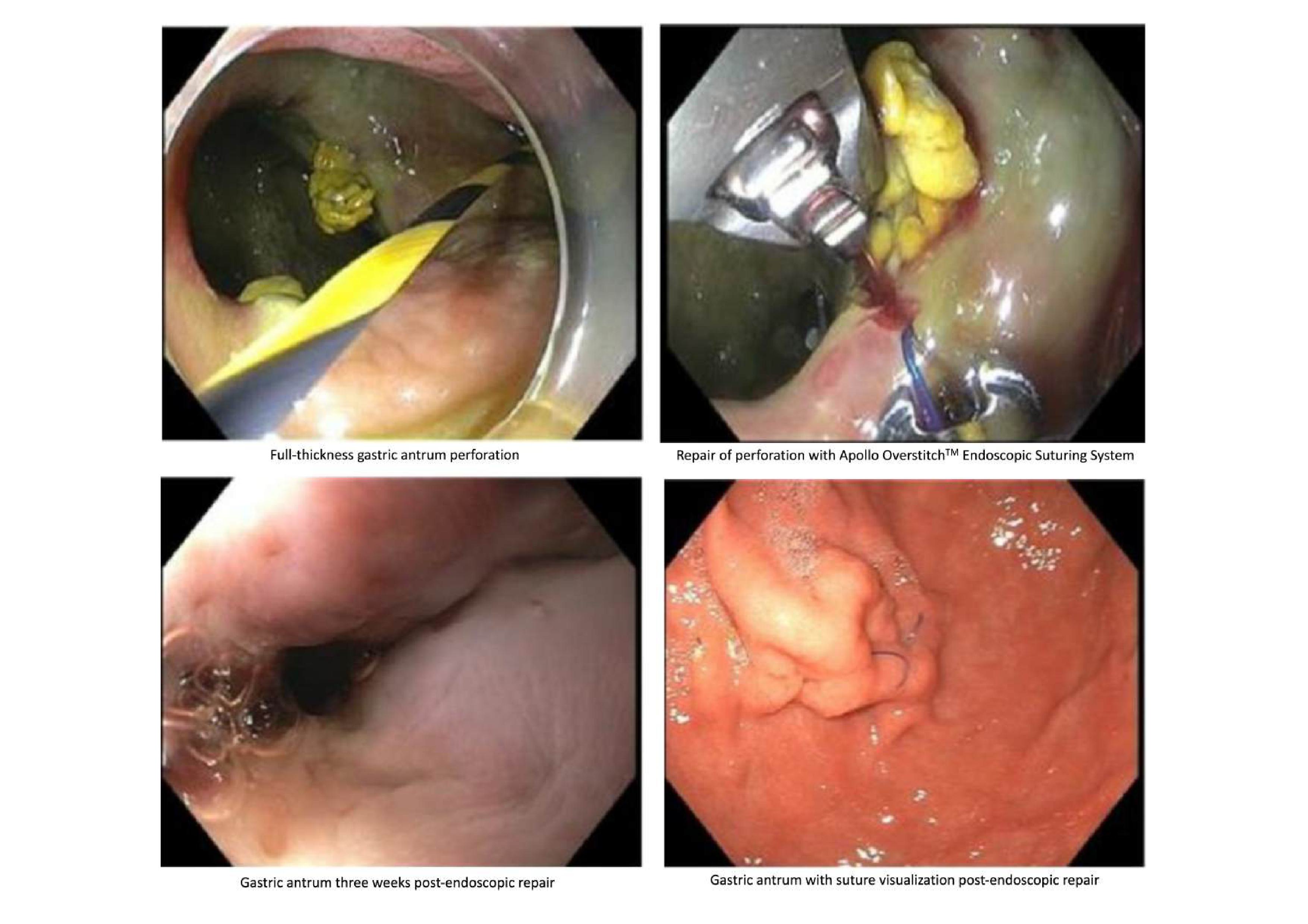
Figure: Figure 1. Esophagogastroduodenoscopy findings at time of initial endoscopic suture and post-endoscopic repair
Disclosures:
Melanie De Shadarevian indicated no relevant financial relationships.
Joy-Marie Hermes indicated no relevant financial relationships.
Matthew Skinner: Boston scientific – Consultant. Microtech – Consultant.
Melanie De Shadarevian, DO1, Joy-Marie Hermes, MD2, Matthew Skinner, MD3. P1466 - Endoscopic Mucosal Defect Closure for Management of High Risk Gastric Perforation, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Valley Hospital Medical Center, Las Vegas, NV; 2Scripps Green Hospital, San Diego, CA; 3Scripps Green Hospital, La Jolla, CA
Introduction: The management of gastrointestinal (GI) tract perforations typically includes surgical repair or observation and supportive care for small low-risk perforations. Endoscopic suturing is an advanced endoscopic technique which has been implemented for achieving tissue defect closure. It has been used in fistula repairs, anastomotic leaks, peroral endoscopic myotomy, and primary sleeve gastroplasty; its use in gastrointestinal perforations has thus far been limited.
Case Description/
Methods: A 44-year old female with a history of decompensated alcoholic cirrhosis complicated by portal hypertension, variceal hemorrhage, portal vein thrombosis and deep-vein thrombosis with inferior vena cava filter presented with hematemesis and melena of one day duration. She was initially hypotensive and tachycardic with a hemoglobin of 4.0. CT of the abdomen & pelvis revealed moderate pneumoperitoneum and multiple intra-abdominal fluid collections. She was intubated, admitted to the ICU and treated supportively including placement of multiple IR drains for abscess management. Esophagogastroduodenoscopy (EGD) revealed a large antral ulcer with full-thickness perforation. Attempts were made to clip the perforation without success. She was deemed a high-risk surgical candidate and recommended palliative care as she remained critically ill. She was transferred to our facility for advanced endoscopic evaluation. Repeat endoscopy demonstrated a 5cm x 3cm near circumferential antral ulcer with perforation and purulence suggestive of peritonitis. Complete defect closure was not achieved on initial endoscopy due to the fibrotic surrounding tissue. Using a combination of endoscopic suturing and fully covered esophageal stent placement across the antrum, the defect was successfully closed after serial endoscopic treatments. Ultimately, CT confirmed defect closure without any contrast extravasation. Oral diet was gradually advanced and the patient was discharged home in stable condition. Two month follow-up EGD demonstrated normal appearing gastric mucosa with no evidence of ongoing perforation nor fistulization at which time the stent was removed.
Discussion: Management of GI tract perforations has classically been supportive/non-operative or surgical. This case demonstrates the utility of minimally invasive endoscopic techniques for management of complex luminal perforations in an appropriate candidate.
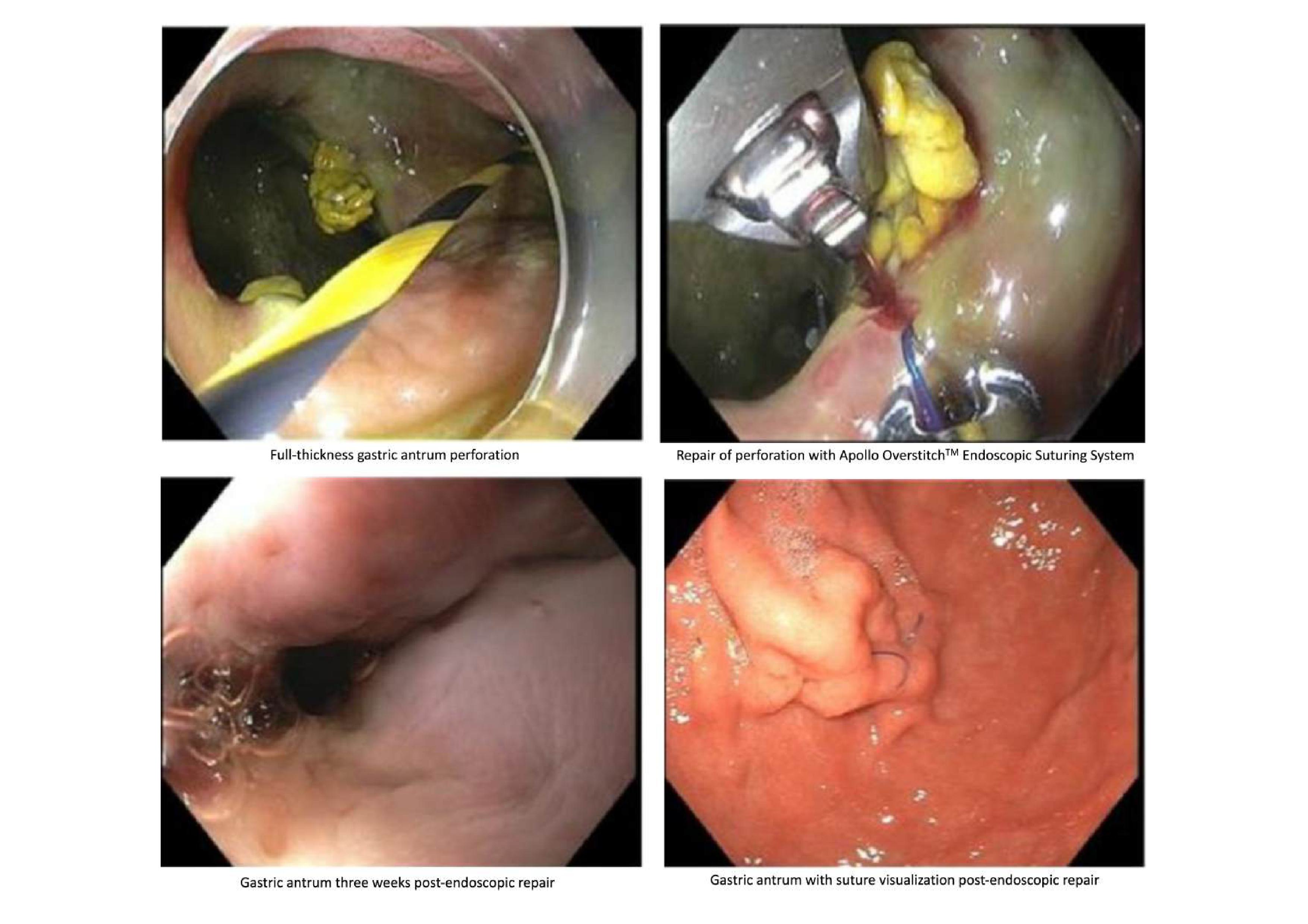
Figure: Figure 1. Esophagogastroduodenoscopy findings at time of initial endoscopic suture and post-endoscopic repair
Disclosures:
Melanie De Shadarevian indicated no relevant financial relationships.
Joy-Marie Hermes indicated no relevant financial relationships.
Matthew Skinner: Boston scientific – Consultant. Microtech – Consultant.
Melanie De Shadarevian, DO1, Joy-Marie Hermes, MD2, Matthew Skinner, MD3. P1466 - Endoscopic Mucosal Defect Closure for Management of High Risk Gastric Perforation, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
