Sunday Poster Session
Category: Interventional Endoscopy
P1455 - Endoscopic Reversal of Vertical Banded Gastroplasty
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall

Helena Steffens, BSc (she/her/hers)
Dartmouth Hitchcock Medical Center
Norwich, VT
Presenting Author(s)
Award: ACG Presidential Poster Award
Helena Steffens, BSc1, Jeffrey M. Adler, MD2
1Dartmouth Hitchcock Medical Center, Norwich, VT; 2Dartmouth Hitchcock Medical Center, Lebanon, NH
Introduction: Endoscopic interventions to reverse bariatric surgeries are promising because they offer the advantage of avoiding a surgical operation. Herein, we report the endoscopic reversal of a vertical banded gastroplasty (VBG) in a patient who suffered chronic reflux and recurrent emesis due to outlet obstruction from the surgical band and chronic retention within a dilated gastric pouch (Figure 1a). Following the endoscopic reversal of the VBG, the patient reported immediate resolution of his symptoms and a much better quality of life.
Case Description/
Methods: A 57-year-old man underwent an open vertical banded gastroplasty in 1989 for obesity, but was unsuccessful at sustaining a reduced body weight. In 2018 he was referred for consultation regarding bothersome reflux symptoms despite lifestyle interventions and acid suppression therapy. Following several attempts to resolve his symptoms by dilating the band to 15 mm, he was referred for an opinion regarding what endoscopic interventions could be performed to permanently reverse the VBG.
An endoscopic intervention was proposed to divide the gastroplasty staple line using endoscopic electrosurgical dissection. During the first of two proposed procedures, a total of three lumen apposing self-expanding metal stents (LAMS) were inserted under endosonographic guidance across the gastroplasty staple line (Figures 1b, 1c, 1d). This step was performed to delineate the correct plane for subsequent dissection, which was then performed two months later, and involved the removal of the stents and electrocautery assisted dissection between the sites where the stents had been placed (Figures 1e, 1f).
Discussion: This case demonstrates an endoscopic method for reversing a VBG. Both procedures were performed entirely on an outpatient basis. The patient recovered quickly and experienced a rapid improvement in symptoms. The development of this technique holds promise for an effective non-operative solution to reversing poorly tolerated VBGs.
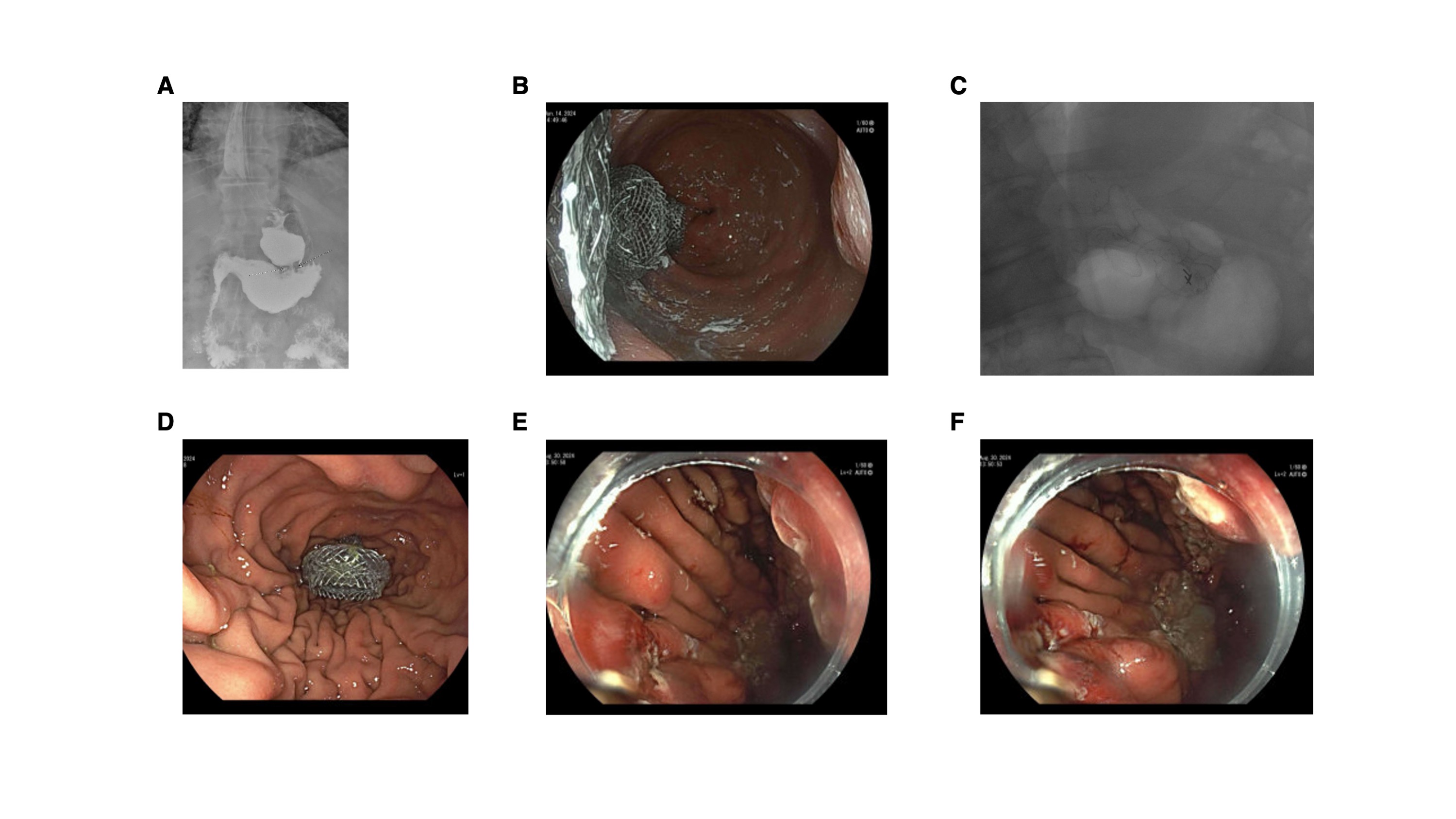
Figure: (A) Prior to VBG reversal. Marked narrowing at the level of the banding with delayed emptying of the intact proximal gastric pouch and back up into the dilated esophagus. (B) The internal flanges of three lumen apposing self-expanding metal stents (LAMS) stents seen from within the gastric pouch. (C) Fluoroscopic image of the three LAMS placed through the gastroplasty. (D) Retroflexed view of LAMS entering the gastric body from the gastric pouch. (E, F) Continuity between gastric pouch and excluded stomach restored after electrosurgical dissection of gastroplasty.
Disclosures:
Helena Steffens indicated no relevant financial relationships.
Jeffrey Adler indicated no relevant financial relationships.
Helena Steffens, BSc1, Jeffrey M. Adler, MD2. P1455 - Endoscopic Reversal of Vertical Banded Gastroplasty, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
Helena Steffens, BSc1, Jeffrey M. Adler, MD2
1Dartmouth Hitchcock Medical Center, Norwich, VT; 2Dartmouth Hitchcock Medical Center, Lebanon, NH
Introduction: Endoscopic interventions to reverse bariatric surgeries are promising because they offer the advantage of avoiding a surgical operation. Herein, we report the endoscopic reversal of a vertical banded gastroplasty (VBG) in a patient who suffered chronic reflux and recurrent emesis due to outlet obstruction from the surgical band and chronic retention within a dilated gastric pouch (Figure 1a). Following the endoscopic reversal of the VBG, the patient reported immediate resolution of his symptoms and a much better quality of life.
Case Description/
Methods: A 57-year-old man underwent an open vertical banded gastroplasty in 1989 for obesity, but was unsuccessful at sustaining a reduced body weight. In 2018 he was referred for consultation regarding bothersome reflux symptoms despite lifestyle interventions and acid suppression therapy. Following several attempts to resolve his symptoms by dilating the band to 15 mm, he was referred for an opinion regarding what endoscopic interventions could be performed to permanently reverse the VBG.
An endoscopic intervention was proposed to divide the gastroplasty staple line using endoscopic electrosurgical dissection. During the first of two proposed procedures, a total of three lumen apposing self-expanding metal stents (LAMS) were inserted under endosonographic guidance across the gastroplasty staple line (Figures 1b, 1c, 1d). This step was performed to delineate the correct plane for subsequent dissection, which was then performed two months later, and involved the removal of the stents and electrocautery assisted dissection between the sites where the stents had been placed (Figures 1e, 1f).
Discussion: This case demonstrates an endoscopic method for reversing a VBG. Both procedures were performed entirely on an outpatient basis. The patient recovered quickly and experienced a rapid improvement in symptoms. The development of this technique holds promise for an effective non-operative solution to reversing poorly tolerated VBGs.
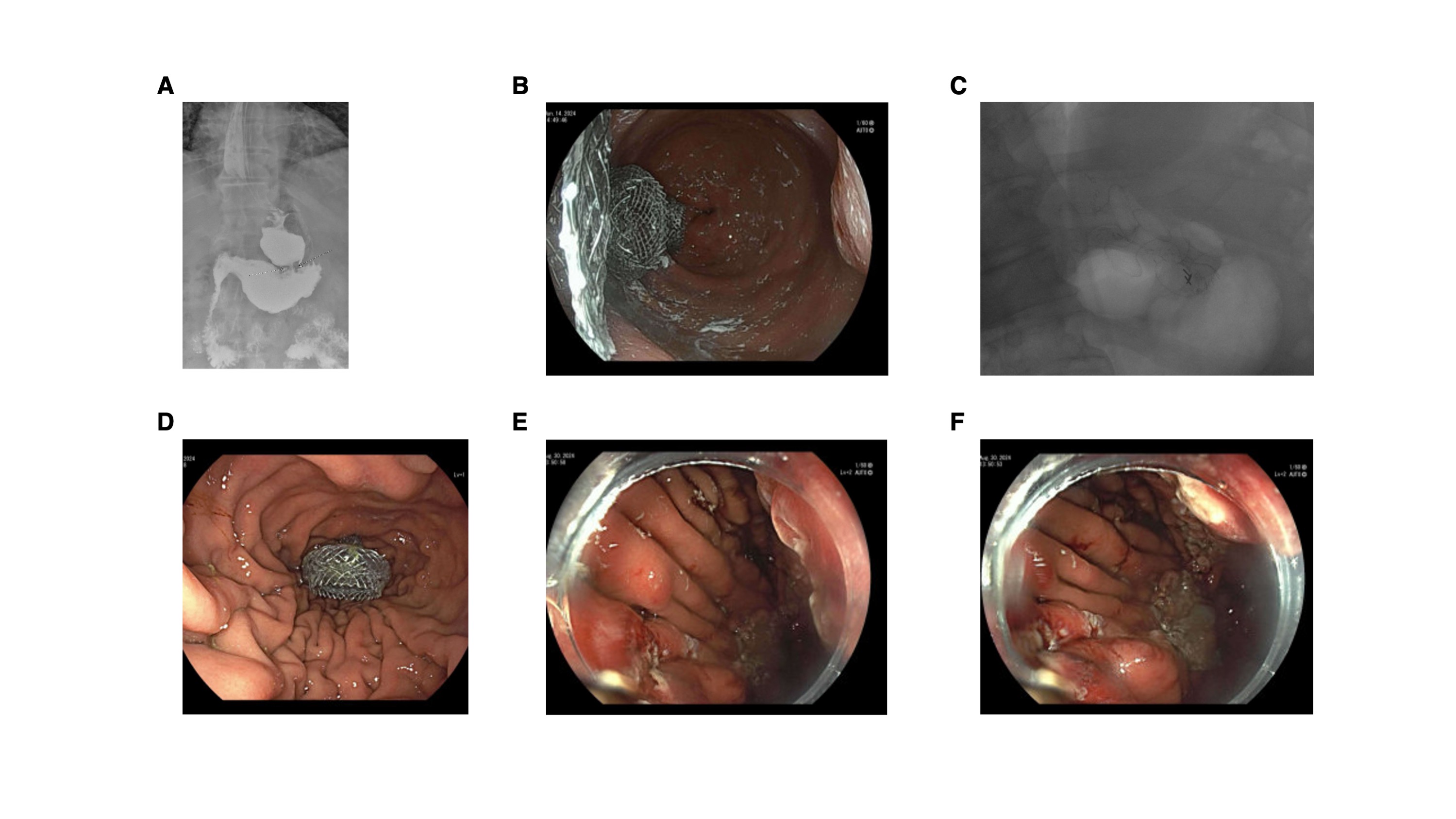
Figure: (A) Prior to VBG reversal. Marked narrowing at the level of the banding with delayed emptying of the intact proximal gastric pouch and back up into the dilated esophagus. (B) The internal flanges of three lumen apposing self-expanding metal stents (LAMS) stents seen from within the gastric pouch. (C) Fluoroscopic image of the three LAMS placed through the gastroplasty. (D) Retroflexed view of LAMS entering the gastric body from the gastric pouch. (E, F) Continuity between gastric pouch and excluded stomach restored after electrosurgical dissection of gastroplasty.
Disclosures:
Helena Steffens indicated no relevant financial relationships.
Jeffrey Adler indicated no relevant financial relationships.
Helena Steffens, BSc1, Jeffrey M. Adler, MD2. P1455 - Endoscopic Reversal of Vertical Banded Gastroplasty, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.


