Sunday Poster Session
Category: Liver
P1563 - Optimizing Early Detection of Hepatic Fibrosis in High-Risk Veterans Through Targeted Outreach and Transient Elastography Evaluation
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall

Pooja Pandita, MD
University of California San Diego
San Diego, CA
Presenting Author(s)
Pooja Pandita, MD1, Ann Deioma, BSN, RN2, Meghan Grant, RN2, Heather Patton, MD1
1University of California San Diego, San Diego, CA; 2VA San Diego Healthcare System, San Diego, CA
Introduction: Despite the availability of non-invasive tools such as the fibrosis-4 index (FIB-4) and Transient Elastography (TE), many high-risk patients remain unidentified and are not systematically referred for liver disease evaluation. This gap in care can delay diagnosis and treatment of hepatic fibrosis, potentially worsening patient outcomes. This project focused on identifying patients at risk for metabolic dysfunction and alcohol-associated steatotic liver disease (MetALD) given the potentially synergistic impact of these variables on liver disease progression.
Methods: We conducted a quality improvement project to identify veterans at high-risk for hepatic fibrosis using the VA MASLD dashboard. Inclusion criteria were: age ≤ 65, alcohol use disorder (AUDIT-C ≥ 4), BMI ≥ 30kg/m2, and FIB-4 score > 2.67. Patients were excluded if they had undergone TE or had a Hepatology clinic appointment within the past year. Eligible patients were contacted through a mailed letter and up to 2 phone calls to offer TE (FibroScan®) evaluation. Patients with a liver stiffness measurement (LSM) ≥ 8kPa were referred to Hepatology for further evaluation and care. The intervention’s effectiveness was based on TE completion, diagnostic yield for advanced fibrosis, and patient surveys to assess satisfaction.
Results: Of 24 VA San Diego Healthcare System patients identified for outreach, 10 (42%) patients scheduled TE within 3 months (Figure 1). Among them, 5/10 (50%) had a LSM ≥ 8kPa and were referred to Hepatology; 1 patient had a technically unsuccessful TE exam. 5/10 of the patients who completed a FibroScan® exam responded to the follow-up survey, of which 100% reported they were “very satisfied” or “satisfied” with the health screening process and 100% reported they would take action to improve their health following the screening. 4/6 patients who were referred to Hepatology attended their appointments, and all were recommended to undergo further imaging and a treatment plan including alcohol reduction and weight loss.
Discussion: Targeted outreach using a combination of clinical risk factors – alcohol use disorder, elevated BMI, and elevated FIB-4 score – was effective in identifying veterans at high risk for hepatic fibrosis. This proactive approach may serve as a scalable model to close existing gaps in liver disease screening and management.
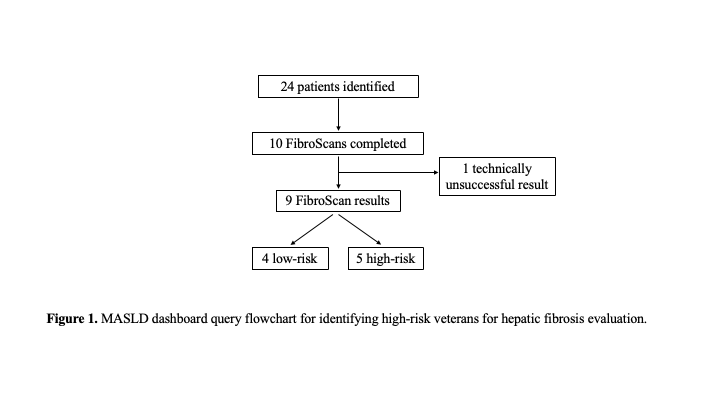
Figure: Figure 1. MASLD dashboard query flowchart for identifying high-risk veterans for hepatic fibrosis evaluation.
Disclosures:
Pooja Pandita indicated no relevant financial relationships.
Ann Deioma indicated no relevant financial relationships.
Meghan Grant indicated no relevant financial relationships.
Heather Patton indicated no relevant financial relationships.
Pooja Pandita, MD1, Ann Deioma, BSN, RN2, Meghan Grant, RN2, Heather Patton, MD1. P1563 - Optimizing Early Detection of Hepatic Fibrosis in High-Risk Veterans Through Targeted Outreach and Transient Elastography Evaluation, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1University of California San Diego, San Diego, CA; 2VA San Diego Healthcare System, San Diego, CA
Introduction: Despite the availability of non-invasive tools such as the fibrosis-4 index (FIB-4) and Transient Elastography (TE), many high-risk patients remain unidentified and are not systematically referred for liver disease evaluation. This gap in care can delay diagnosis and treatment of hepatic fibrosis, potentially worsening patient outcomes. This project focused on identifying patients at risk for metabolic dysfunction and alcohol-associated steatotic liver disease (MetALD) given the potentially synergistic impact of these variables on liver disease progression.
Methods: We conducted a quality improvement project to identify veterans at high-risk for hepatic fibrosis using the VA MASLD dashboard. Inclusion criteria were: age ≤ 65, alcohol use disorder (AUDIT-C ≥ 4), BMI ≥ 30kg/m2, and FIB-4 score > 2.67. Patients were excluded if they had undergone TE or had a Hepatology clinic appointment within the past year. Eligible patients were contacted through a mailed letter and up to 2 phone calls to offer TE (FibroScan®) evaluation. Patients with a liver stiffness measurement (LSM) ≥ 8kPa were referred to Hepatology for further evaluation and care. The intervention’s effectiveness was based on TE completion, diagnostic yield for advanced fibrosis, and patient surveys to assess satisfaction.
Results: Of 24 VA San Diego Healthcare System patients identified for outreach, 10 (42%) patients scheduled TE within 3 months (Figure 1). Among them, 5/10 (50%) had a LSM ≥ 8kPa and were referred to Hepatology; 1 patient had a technically unsuccessful TE exam. 5/10 of the patients who completed a FibroScan® exam responded to the follow-up survey, of which 100% reported they were “very satisfied” or “satisfied” with the health screening process and 100% reported they would take action to improve their health following the screening. 4/6 patients who were referred to Hepatology attended their appointments, and all were recommended to undergo further imaging and a treatment plan including alcohol reduction and weight loss.
Discussion: Targeted outreach using a combination of clinical risk factors – alcohol use disorder, elevated BMI, and elevated FIB-4 score – was effective in identifying veterans at high risk for hepatic fibrosis. This proactive approach may serve as a scalable model to close existing gaps in liver disease screening and management.
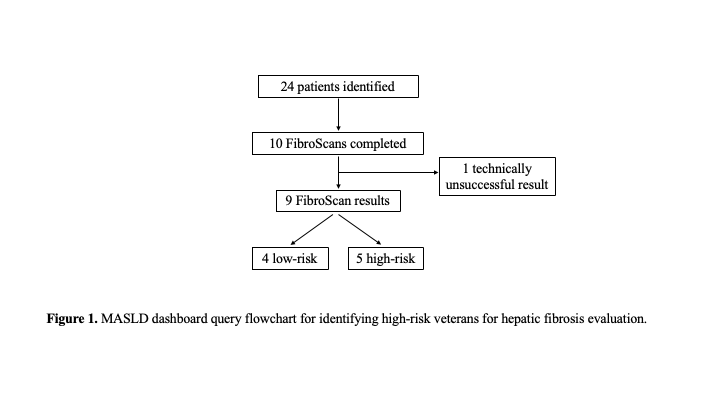
Figure: Figure 1. MASLD dashboard query flowchart for identifying high-risk veterans for hepatic fibrosis evaluation.
Disclosures:
Pooja Pandita indicated no relevant financial relationships.
Ann Deioma indicated no relevant financial relationships.
Meghan Grant indicated no relevant financial relationships.
Heather Patton indicated no relevant financial relationships.
Pooja Pandita, MD1, Ann Deioma, BSN, RN2, Meghan Grant, RN2, Heather Patton, MD1. P1563 - Optimizing Early Detection of Hepatic Fibrosis in High-Risk Veterans Through Targeted Outreach and Transient Elastography Evaluation, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
