Sunday Poster Session
Category: Liver
P1559 - Racial Disparity in Weight Loss of MASLD/MASH Patients in a Predominantly African American Academic Medical Center Population
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall
- PN
Paul Naylor, PhD
Wayne State School of Medicine
Detroit, MI
Presenting Author(s)
Michael Mello, BS, Sriraj Atluri, BS, Reema Smadi, BS, Abigail Limary, BS, Cyra Kharas, BS, Izabel Thomas, BS, Astha Saini, DO, Paul Naylor, PhD, Milton Mutchnick, MD
Wayne State School of Medicine, Detroit, MI
Introduction: African American (AA) patients are less likely to develop Metabolic Dysfunction–Associated Steatotic Liver Disease (MASLD) compared to non-AA populations. Given the emphasis on weight loss as a cornerstone of MASLD management and the limited AA focus in studies, we evaluated the relationship between weight change and fibrosis progression in a predominantly AA patient Internal Medicine population.
Methods: We identified 317 patients with MASLD or MASH (Metabolic Dysfunction–Associated Steatohepatitis) between 2017 and 2023. Laboratory data at least two years apart was available for 121 patients. Fibrosis was assessed using the NAFLD Fibrosis Score (NFS), which incorporates age, BMI, AST, ALT, platelet count, and albumin. We also analyzed APRI and FIB-4 scores. Patients were stratified into three groups based on weight change: weight gain ( >4% pounds increase; n= 28%), weight stable (±4% pounds ; n= 38%), and weight loss ( >4% pounds decrease; n=34%). A few patients had weight loss surgery (10%) or received GLP-1 agonist therapy (16%). Paired t-tests were used to evaluate within-group changes in fibrosis scores.
Results: The mean age was 51 years; 66% were female, and 65% identified as AA. Weight gain was associated with a significant increase in fibrosis (p < 0.001), while weight loss was associated with a significant reduction in fibrosis (p < 0.0008), as measured by NFS (Figure 1). This was consistent across racial groups, although the magnitude of benefit from weight loss appeared more pronounced among AA patients. Interestingly, patients who gained weight had lower baseline fibrosis scores compared to those who maintained or lost weight. In subgroup analysis stratified by MASLD versus MASH (Figure 2), weight gain led to fibrosis progression, and weight loss was associated with fibrosis improvement regardless of initial fibrosis status. Changes in FIB-4 and APRI mirrored this trend for weight gain, but the impact of weight loss on these scores was less evident.
Discussion: Regardless of race or baseline fibrosis severity, weight loss is associated with improvement in fibrosis as assessed by NFS, while weight gain is associated with worsening fibrosis. The benefit of weight loss appeared greater among AA patients, although the underlying mechanisms require further investigation. Importantly, the positive impact of weight loss on fibrosis was observed even in patients with more advanced disease (MASH), suggesting a potential benefit across the MASLD spectrum.
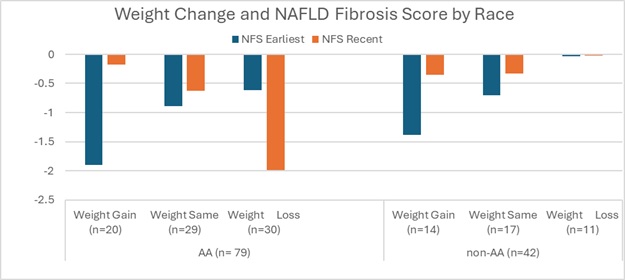
Figure: Figure 1. Weight Loss and Change in NFS by Race. A decrease in NFS reflects improvement in fibrosis; an increase reflects worsening. Weight gain results in an increase in fibrosis. Weight loss results in an improvement in fibrosis.
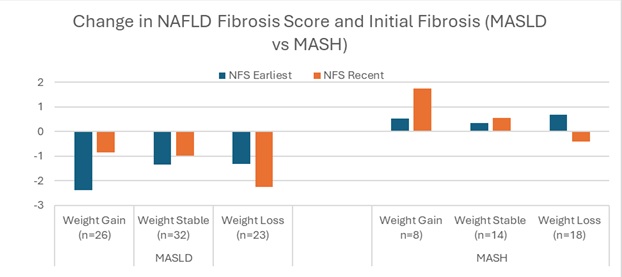
Figure: Figure 2 Change in NFS with Weight Change Stratified by MASLD vs. MASH. Weight gain led to increased fibrosis regardless of initial fibrosis status; weight loss led to improvement.
Disclosures:
Michael Mello indicated no relevant financial relationships.
Sriraj Atluri indicated no relevant financial relationships.
Reema Smadi indicated no relevant financial relationships.
Abigail Limary indicated no relevant financial relationships.
Cyra Kharas indicated no relevant financial relationships.
Izabel Thomas indicated no relevant financial relationships.
Astha Saini indicated no relevant financial relationships.
Paul Naylor: Janssen Biotech Inc – Grant/Research Support. Salix Pharmaceuticals – Grant/Research Support.
Milton Mutchnick: Janssen Biotech Inc – Grant/Research Support. Madrigal Pharmaceuticals – Speakers Bureau. Salix Pharmaceuticals – Grant/Research Support.
Michael Mello, BS, Sriraj Atluri, BS, Reema Smadi, BS, Abigail Limary, BS, Cyra Kharas, BS, Izabel Thomas, BS, Astha Saini, DO, Paul Naylor, PhD, Milton Mutchnick, MD. P1559 - Racial Disparity in Weight Loss of MASLD/MASH Patients in a Predominantly African American Academic Medical Center Population, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
Wayne State School of Medicine, Detroit, MI
Introduction: African American (AA) patients are less likely to develop Metabolic Dysfunction–Associated Steatotic Liver Disease (MASLD) compared to non-AA populations. Given the emphasis on weight loss as a cornerstone of MASLD management and the limited AA focus in studies, we evaluated the relationship between weight change and fibrosis progression in a predominantly AA patient Internal Medicine population.
Methods: We identified 317 patients with MASLD or MASH (Metabolic Dysfunction–Associated Steatohepatitis) between 2017 and 2023. Laboratory data at least two years apart was available for 121 patients. Fibrosis was assessed using the NAFLD Fibrosis Score (NFS), which incorporates age, BMI, AST, ALT, platelet count, and albumin. We also analyzed APRI and FIB-4 scores. Patients were stratified into three groups based on weight change: weight gain ( >4% pounds increase; n= 28%), weight stable (±4% pounds ; n= 38%), and weight loss ( >4% pounds decrease; n=34%). A few patients had weight loss surgery (10%) or received GLP-1 agonist therapy (16%). Paired t-tests were used to evaluate within-group changes in fibrosis scores.
Results: The mean age was 51 years; 66% were female, and 65% identified as AA. Weight gain was associated with a significant increase in fibrosis (p < 0.001), while weight loss was associated with a significant reduction in fibrosis (p < 0.0008), as measured by NFS (Figure 1). This was consistent across racial groups, although the magnitude of benefit from weight loss appeared more pronounced among AA patients. Interestingly, patients who gained weight had lower baseline fibrosis scores compared to those who maintained or lost weight. In subgroup analysis stratified by MASLD versus MASH (Figure 2), weight gain led to fibrosis progression, and weight loss was associated with fibrosis improvement regardless of initial fibrosis status. Changes in FIB-4 and APRI mirrored this trend for weight gain, but the impact of weight loss on these scores was less evident.
Discussion: Regardless of race or baseline fibrosis severity, weight loss is associated with improvement in fibrosis as assessed by NFS, while weight gain is associated with worsening fibrosis. The benefit of weight loss appeared greater among AA patients, although the underlying mechanisms require further investigation. Importantly, the positive impact of weight loss on fibrosis was observed even in patients with more advanced disease (MASH), suggesting a potential benefit across the MASLD spectrum.
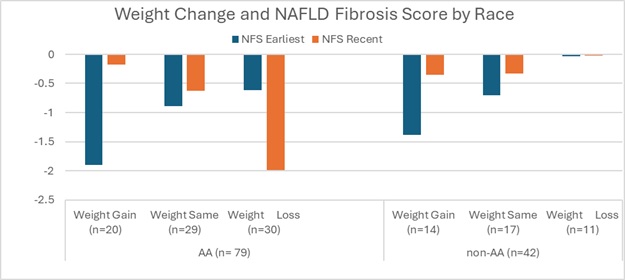
Figure: Figure 1. Weight Loss and Change in NFS by Race. A decrease in NFS reflects improvement in fibrosis; an increase reflects worsening. Weight gain results in an increase in fibrosis. Weight loss results in an improvement in fibrosis.
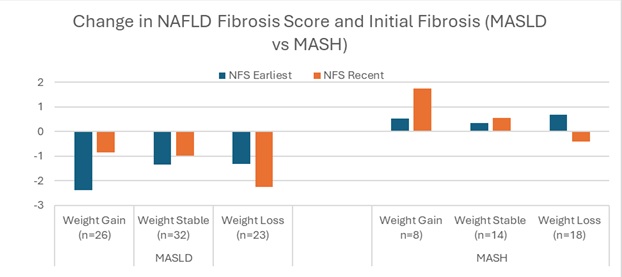
Figure: Figure 2 Change in NFS with Weight Change Stratified by MASLD vs. MASH. Weight gain led to increased fibrosis regardless of initial fibrosis status; weight loss led to improvement.
Disclosures:
Michael Mello indicated no relevant financial relationships.
Sriraj Atluri indicated no relevant financial relationships.
Reema Smadi indicated no relevant financial relationships.
Abigail Limary indicated no relevant financial relationships.
Cyra Kharas indicated no relevant financial relationships.
Izabel Thomas indicated no relevant financial relationships.
Astha Saini indicated no relevant financial relationships.
Paul Naylor: Janssen Biotech Inc – Grant/Research Support. Salix Pharmaceuticals – Grant/Research Support.
Milton Mutchnick: Janssen Biotech Inc – Grant/Research Support. Madrigal Pharmaceuticals – Speakers Bureau. Salix Pharmaceuticals – Grant/Research Support.
Michael Mello, BS, Sriraj Atluri, BS, Reema Smadi, BS, Abigail Limary, BS, Cyra Kharas, BS, Izabel Thomas, BS, Astha Saini, DO, Paul Naylor, PhD, Milton Mutchnick, MD. P1559 - Racial Disparity in Weight Loss of MASLD/MASH Patients in a Predominantly African American Academic Medical Center Population, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.

