Sunday Poster Session
Category: Liver
P1553 - Autoimmune Hepatic Involvement in Systemic Sclerosis: Systematic Review and Meta-Analysis
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall

Bipneet Singh, MD
Henry Ford Jackson Hospital
Lexington, KY
Presenting Author(s)
Bipneet Singh, MD1, Jahnavi Ethakota, MD1, Palak Grover, MD1, Aalam Sohal, MD2, Rahul Jain, MBBS3, Gurleen Kaur, MBBS4, Syed-Mohammed Jafri, MD5
1Henry Ford Jackson Hospital, Jackson, MI; 2Creighton University School of Medicine, Phoenix, AZ; 3Sri Manakula Vinayagar Medical College, Pondicherry, Puducherry, India; 4Government Medical College and Hospital, Khanna, Punjab, India; 5Henry Ford Health, Detroit, MI
Introduction: Systemic sclerosis (SSc) is a heterogeneous, multisystem autoimmune disease characterized by fibrosis in genetically predisposed individuals. It can involve multiple organ systems, but hepatic involvement is rare. In this study, we aim to find the correlation of liver disease, especially primary biliary cholangitis (PBC) and autoimmune hepatitis (AIH), in the population with SSc. Further, the correlation of anti-mitochondrial antibody (AMA) and other autoantibodies was done.
Methods: PubMed, Cochrane, Google Scholar, and Embase were searched for liver disease in SSc, and 11 studies were selected for analysis. Cochrane risk of bias tools and meta-analysis online were used. Controls were taken from the prevalence in the respective countries around the same time.
Results: Among 11 studies including 2,797 patients with systemic sclerosis (SSc), 190 (6.7%) had liver disease, with 157 (5.6%) attributed to autoimmune causes. Primary biliary cholangitis (PBC) was the most common (5%), followed by autoimmune hepatitis (AIH) at 1.2%. PSC was only seen in 1 patient across the studies. There was a significant association in prevalence compared to the general population (Figure 1). Antimitochondrial antibodies (AMA) were positive in 10.87%, and anti-sp100 in 3.1%.
Discussion: The increased prevalence of autoimmune hepatobiliary conditions, such as primary biliary cholangitis (PBC), in systemic sclerosis (SSc) patients is likely due to overlapping immunopathogenic features, including shared regulatory T cell abnormalities and common genetic variants (e.g., STAT4, IRF5, NF-κB, IRF8). PBC was observed in approximately 5.6% of SSc patients—significantly higher than the general population prevalence of 0.02% to 0.04%—highlighting a strong association. This link is further supported by the presence of antimitochondrial antibodies (AMA) in 10.87% of patients, suggesting a high rate of subclinical or evolving PBC in this population.
Autoimmune hepatitis (AIH) was identified in 1.2% of SSc patients. This rate exceeds general population estimates (0.02%–0.05%), suggesting that SSc may predispose patients to broader autoimmune liver involvement beyond PBC. Serological data revealed a substantial presence of liver-specific autoantibodies in SSc patients. In addition to AMA, anti-sp100 (3.1%) and anti-gp210 antibodies were frequently observed. These antibodies serve not only as diagnostic markers but may also offer prognostic value, reinforcing the link between SSc and autoimmune hepatobiliary pathology.
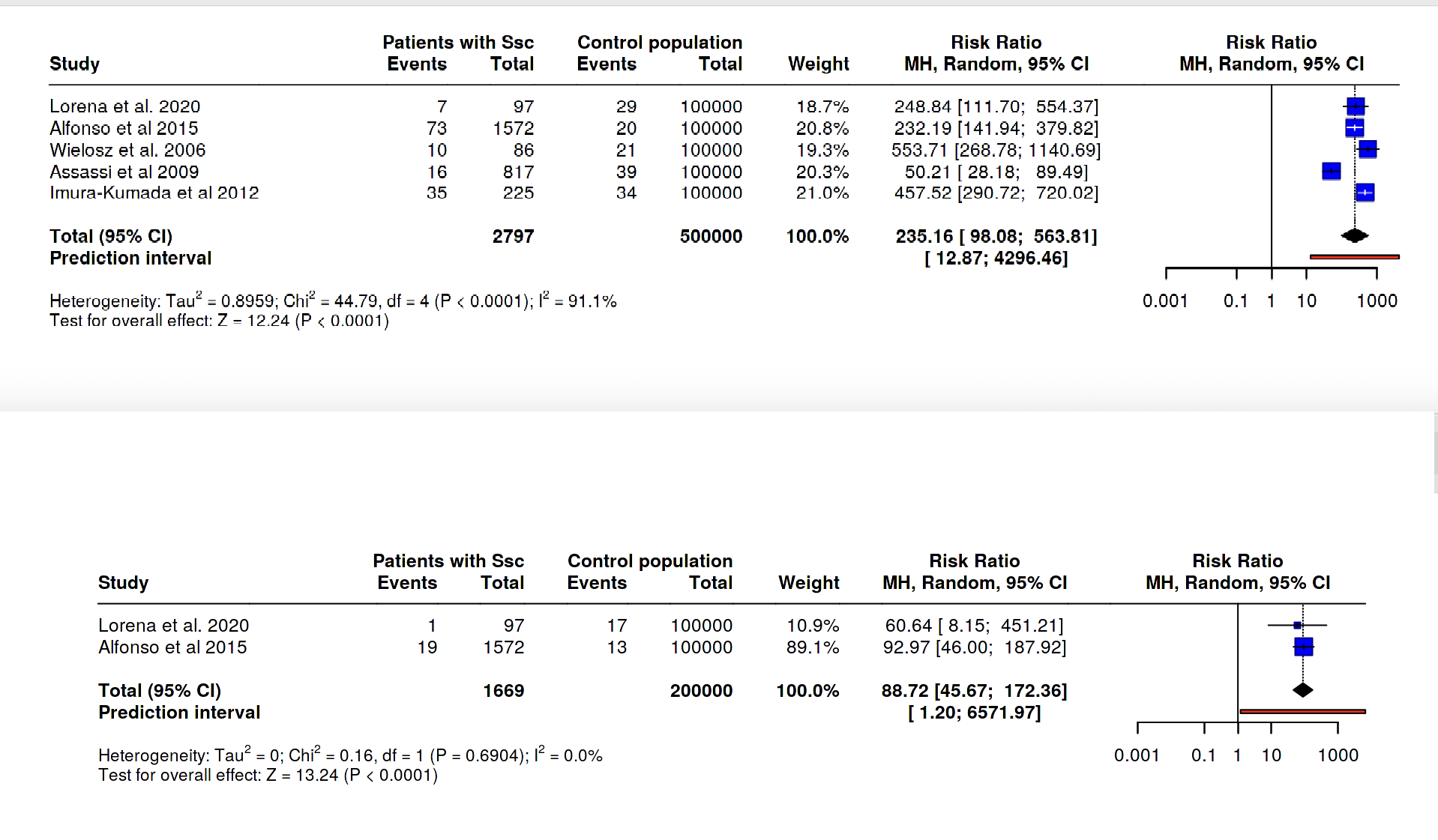
Figure: Forrest plot depicting a significant association between PBC and SSc and then AIH and SSc
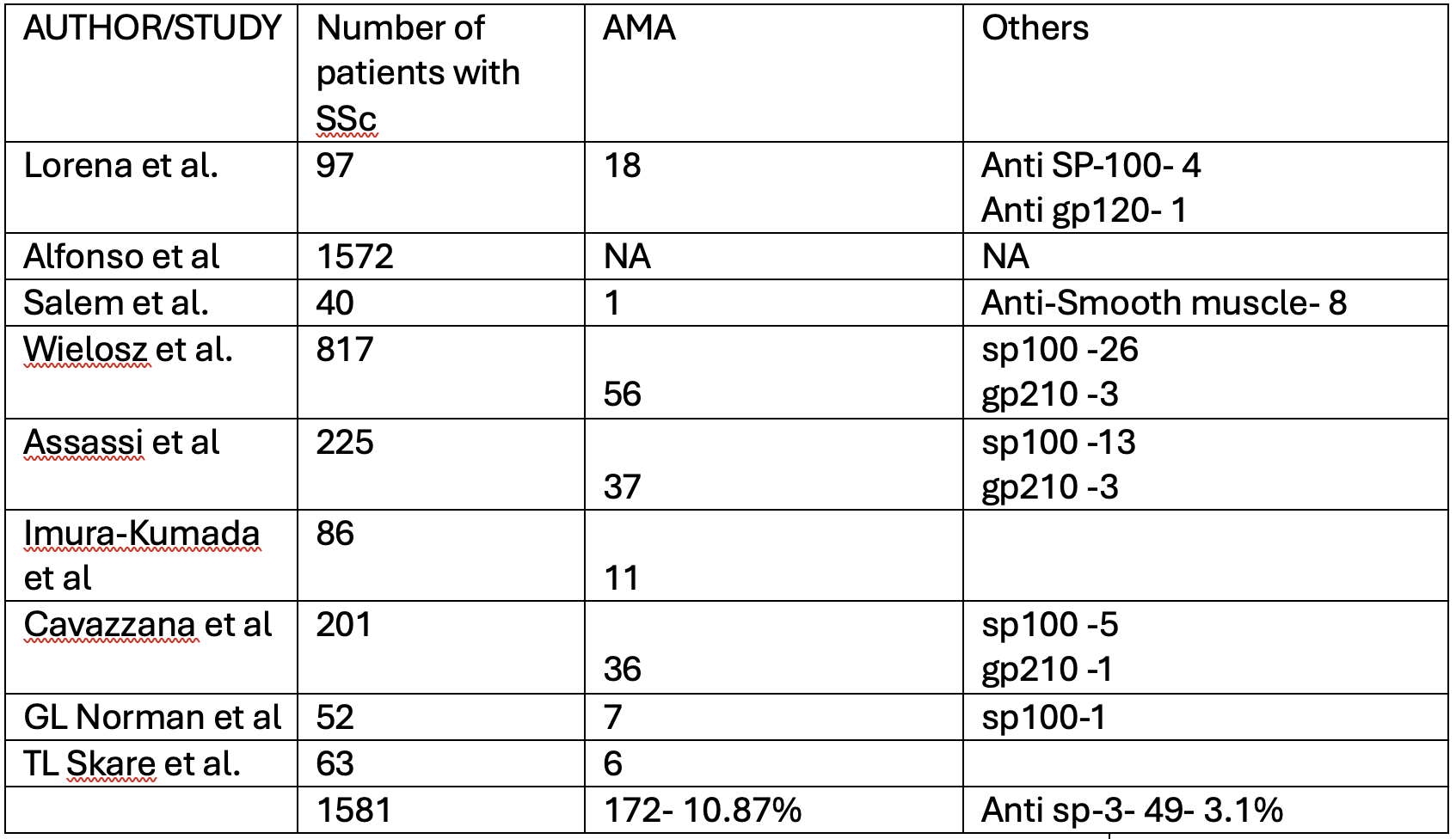
Figure: AMA and sp-100 positivity in the studies included in SR.
Disclosures:
Bipneet Singh indicated no relevant financial relationships.
Jahnavi Ethakota indicated no relevant financial relationships.
Palak Grover indicated no relevant financial relationships.
Aalam Sohal indicated no relevant financial relationships.
Rahul Jain indicated no relevant financial relationships.
Gurleen Kaur indicated no relevant financial relationships.
Syed-Mohammed Jafri: Abbvie – Speakers Bureau. Gilead – Speakers Bureau. Intercept – Speakers Bureau. Ironwood – Speakers Bureau. Takeda – Speakers Bureau.
Bipneet Singh, MD1, Jahnavi Ethakota, MD1, Palak Grover, MD1, Aalam Sohal, MD2, Rahul Jain, MBBS3, Gurleen Kaur, MBBS4, Syed-Mohammed Jafri, MD5. P1553 - Autoimmune Hepatic Involvement in Systemic Sclerosis: Systematic Review and Meta-Analysis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Henry Ford Jackson Hospital, Jackson, MI; 2Creighton University School of Medicine, Phoenix, AZ; 3Sri Manakula Vinayagar Medical College, Pondicherry, Puducherry, India; 4Government Medical College and Hospital, Khanna, Punjab, India; 5Henry Ford Health, Detroit, MI
Introduction: Systemic sclerosis (SSc) is a heterogeneous, multisystem autoimmune disease characterized by fibrosis in genetically predisposed individuals. It can involve multiple organ systems, but hepatic involvement is rare. In this study, we aim to find the correlation of liver disease, especially primary biliary cholangitis (PBC) and autoimmune hepatitis (AIH), in the population with SSc. Further, the correlation of anti-mitochondrial antibody (AMA) and other autoantibodies was done.
Methods: PubMed, Cochrane, Google Scholar, and Embase were searched for liver disease in SSc, and 11 studies were selected for analysis. Cochrane risk of bias tools and meta-analysis online were used. Controls were taken from the prevalence in the respective countries around the same time.
Results: Among 11 studies including 2,797 patients with systemic sclerosis (SSc), 190 (6.7%) had liver disease, with 157 (5.6%) attributed to autoimmune causes. Primary biliary cholangitis (PBC) was the most common (5%), followed by autoimmune hepatitis (AIH) at 1.2%. PSC was only seen in 1 patient across the studies. There was a significant association in prevalence compared to the general population (Figure 1). Antimitochondrial antibodies (AMA) were positive in 10.87%, and anti-sp100 in 3.1%.
Discussion: The increased prevalence of autoimmune hepatobiliary conditions, such as primary biliary cholangitis (PBC), in systemic sclerosis (SSc) patients is likely due to overlapping immunopathogenic features, including shared regulatory T cell abnormalities and common genetic variants (e.g., STAT4, IRF5, NF-κB, IRF8). PBC was observed in approximately 5.6% of SSc patients—significantly higher than the general population prevalence of 0.02% to 0.04%—highlighting a strong association. This link is further supported by the presence of antimitochondrial antibodies (AMA) in 10.87% of patients, suggesting a high rate of subclinical or evolving PBC in this population.
Autoimmune hepatitis (AIH) was identified in 1.2% of SSc patients. This rate exceeds general population estimates (0.02%–0.05%), suggesting that SSc may predispose patients to broader autoimmune liver involvement beyond PBC. Serological data revealed a substantial presence of liver-specific autoantibodies in SSc patients. In addition to AMA, anti-sp100 (3.1%) and anti-gp210 antibodies were frequently observed. These antibodies serve not only as diagnostic markers but may also offer prognostic value, reinforcing the link between SSc and autoimmune hepatobiliary pathology.
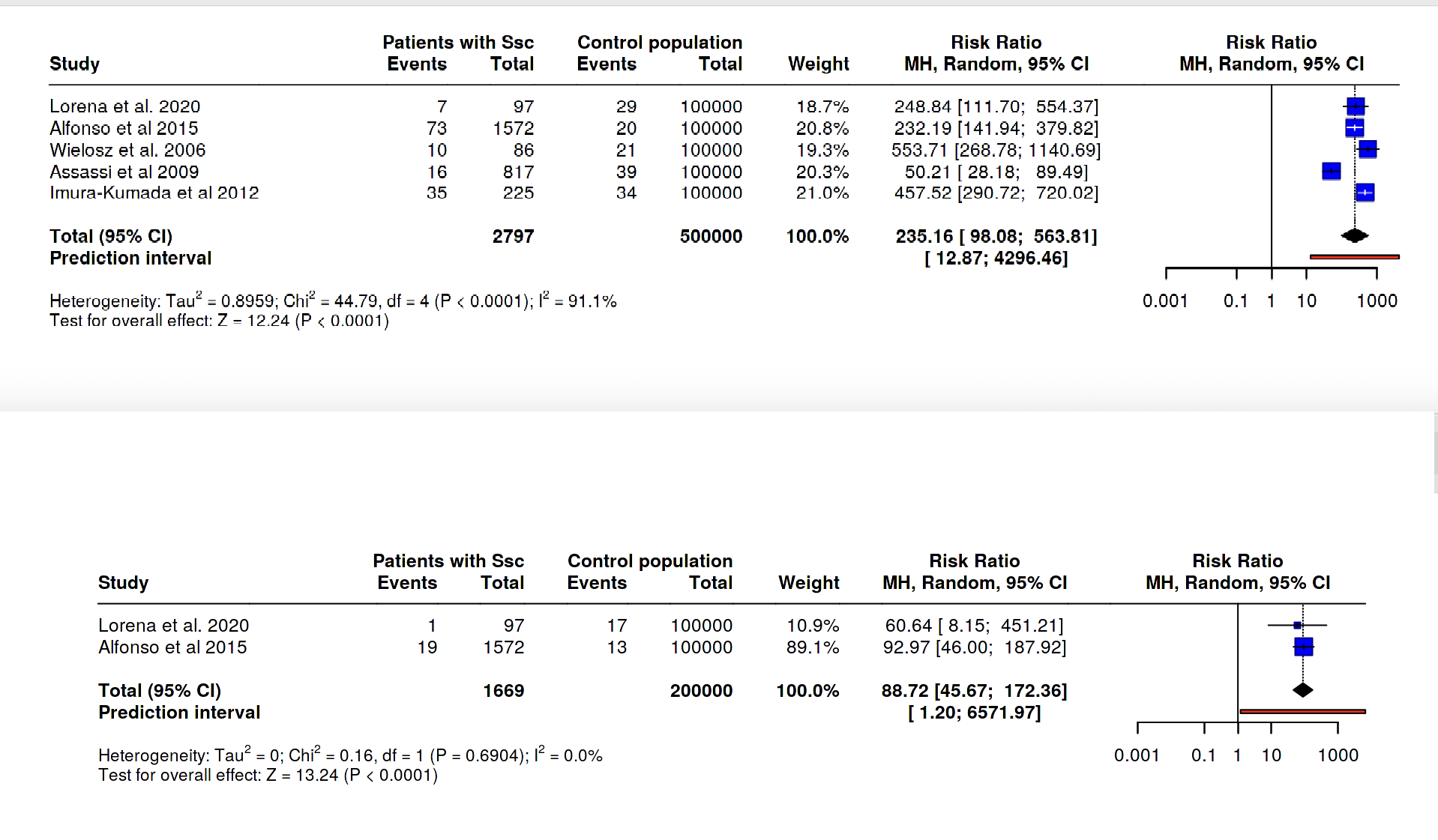
Figure: Forrest plot depicting a significant association between PBC and SSc and then AIH and SSc
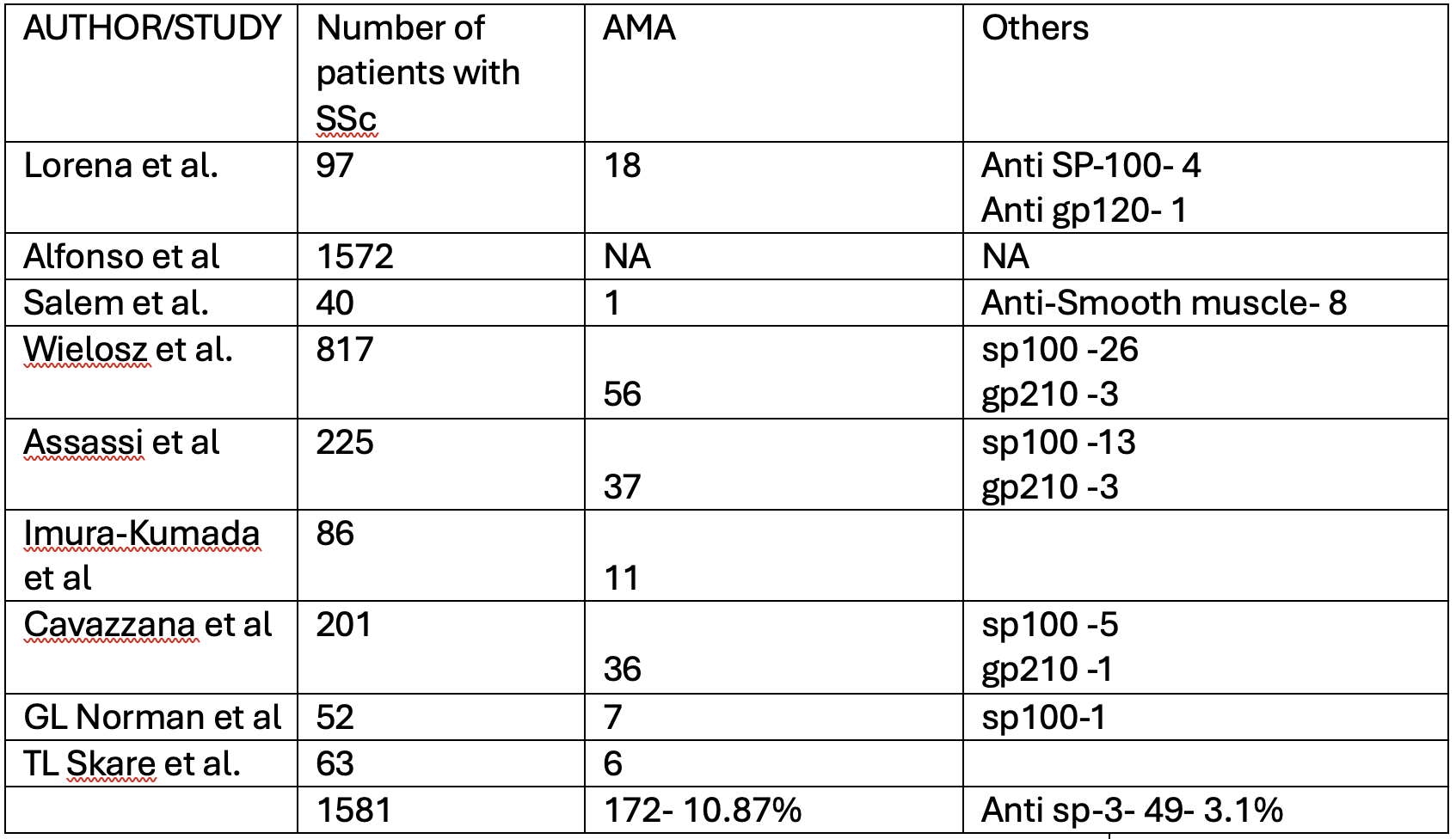
Figure: AMA and sp-100 positivity in the studies included in SR.
Disclosures:
Bipneet Singh indicated no relevant financial relationships.
Jahnavi Ethakota indicated no relevant financial relationships.
Palak Grover indicated no relevant financial relationships.
Aalam Sohal indicated no relevant financial relationships.
Rahul Jain indicated no relevant financial relationships.
Gurleen Kaur indicated no relevant financial relationships.
Syed-Mohammed Jafri: Abbvie – Speakers Bureau. Gilead – Speakers Bureau. Intercept – Speakers Bureau. Ironwood – Speakers Bureau. Takeda – Speakers Bureau.
Bipneet Singh, MD1, Jahnavi Ethakota, MD1, Palak Grover, MD1, Aalam Sohal, MD2, Rahul Jain, MBBS3, Gurleen Kaur, MBBS4, Syed-Mohammed Jafri, MD5. P1553 - Autoimmune Hepatic Involvement in Systemic Sclerosis: Systematic Review and Meta-Analysis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.

