Sunday Poster Session
Category: Liver
P1547 - High Fibrosis Risk in Lean Metabolic Dysfunction‐Associated Steatotic Liver Disease (MASLD): A NHANES 2017–2018 Analysis Challenging BMI-Based Screening
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall
Justin-James Chua, MD (he/him/his)
University of Pittsburgh Medical Center
Pittsburgh, PA
Presenting Author(s)
Justin-James Chua, MD1, Nikita Garg, MD2, Varun Jain, MD1, Tushar Abhinav, MD3, Shruthi Sethuraman, MD1, Paarth Kapadia, MD1, Nanditha Venkatesan, MD1, Lizeth Cifuentas, MD1
1University of Pittsburgh Medical Center, Pittsburgh, PA; 2Geisinger Wyoming Valley Medical Center, Wilkes-Barre, PA; 3The Wright Center for Graduate Medical Education, Scranton, PA
Introduction: Lean metabolic dysfunction-associated steatotic liver disease (MASLD) is an underrecognized subset of MASLD defined as patients with MASLD and a BMI < 23 kg/m2 for the Asian populace and < 25 kg/m2 for all other races. MASLD is estimated to have a global prevalence of ~30% with lean MASLD accounting for ~13% of MASLD cases, notably disproportionately more common in Asian or Hispanic populations. Importantly, lean MASLD patients experience overall mortality rates that are equal to or higher compared to non-lean MASLD patients, emphasizing the need to extend MASLD screening to normal BMI adults across diverse regions. We aimed to characterize the prevalence and fibrosis burden of MASLD among normal BMI adults in a nationally representative U.S. population.
Methods: We performed a cross-sectional analysis of U.S. adults (≥18 years) from NHANES 2017–2018 with valid transient elastography, excluding those with missing key covariates. Lean adults were defined as BMI < 25 kg/m2 and MASLD was defined as ALT ≥ 40 U/L with ≥ 2 metabolic risk factors (TG ≥ 150 mg/dL, glucose ≥ 100 mg/dL, or low sex-specific HDL). Notably, Non-Hispanic Asians were unable to be separated from “Other Race” since not enough were captured to account for event variation. Advanced fibrosis risk was classified into three stages based on the fibrosis-4 (FIB-4) score: low (≤ 1.3), intermediate (1.31–2.67), or high ( > 2.67). FIB-4 was then evaluated across sex, age, and race/ethnicity.
Results: Among 1,105 lean adults, 253 (23%) met criteria for MASLD (Table 1). Of these, 21.3% had intermediate or high fibrosis risk. High fibrosis risk was more prevalent in males (4.5%) than females (1.7%), and combined intermediate or high fibrosis risk increased with age (2.4% in < 40 years old versus 29.7% in ≥ 60 years old). Notably, 23.1% of Non-Hispanic Black and 21.7% of Mexican American lean MASLD individuals had intermediate or high fibrosis risk (Figure 1).
Discussion: In this nationally representative cohort, male sex, Non-Hispanic Black race, and Mexican American race emerged as robust predictors of advanced fibrosis risk on transient elastography, highlighting fibrosis risk beyond obesity. These findings support expanding noninvasive fibrosis screening to all MASLD patients irrespective of BMI with particular focus on lean individuals and high-risk demographics. Longitudinal studies should validate these predictors against elastography outcomes and assess the impact of early fibrosis detection on clinical endpoints.
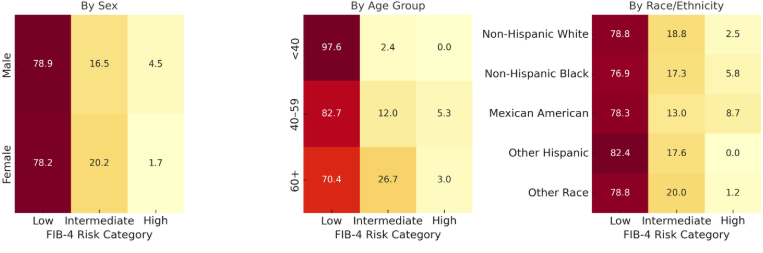
Figure: Table 1. FIB-4 fibrosis risk stratification in adults with lean MASLD
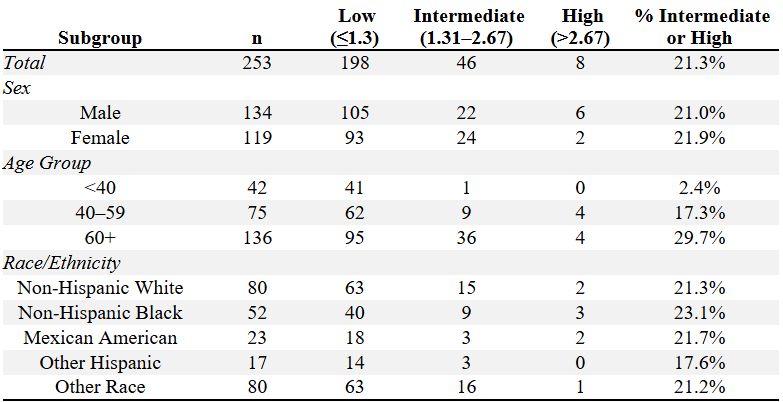
Figure: Figure 1. Heatmap summarizing FIB-4 fibrosis risk distribution among lean MASLD individuals by sex, age group, and race/ethnicity
Disclosures:
Justin-James Chua indicated no relevant financial relationships.
Nikita Garg indicated no relevant financial relationships.
Varun Jain indicated no relevant financial relationships.
Tushar Abhinav indicated no relevant financial relationships.
Shruthi Sethuraman indicated no relevant financial relationships.
Paarth Kapadia indicated no relevant financial relationships.
Nanditha Venkatesan indicated no relevant financial relationships.
Lizeth Cifuentas indicated no relevant financial relationships.
Justin-James Chua, MD1, Nikita Garg, MD2, Varun Jain, MD1, Tushar Abhinav, MD3, Shruthi Sethuraman, MD1, Paarth Kapadia, MD1, Nanditha Venkatesan, MD1, Lizeth Cifuentas, MD1. P1547 - High Fibrosis Risk in Lean Metabolic Dysfunction‐Associated Steatotic Liver Disease (MASLD): A NHANES 2017–2018 Analysis Challenging BMI-Based Screening, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1University of Pittsburgh Medical Center, Pittsburgh, PA; 2Geisinger Wyoming Valley Medical Center, Wilkes-Barre, PA; 3The Wright Center for Graduate Medical Education, Scranton, PA
Introduction: Lean metabolic dysfunction-associated steatotic liver disease (MASLD) is an underrecognized subset of MASLD defined as patients with MASLD and a BMI < 23 kg/m2 for the Asian populace and < 25 kg/m2 for all other races. MASLD is estimated to have a global prevalence of ~30% with lean MASLD accounting for ~13% of MASLD cases, notably disproportionately more common in Asian or Hispanic populations. Importantly, lean MASLD patients experience overall mortality rates that are equal to or higher compared to non-lean MASLD patients, emphasizing the need to extend MASLD screening to normal BMI adults across diverse regions. We aimed to characterize the prevalence and fibrosis burden of MASLD among normal BMI adults in a nationally representative U.S. population.
Methods: We performed a cross-sectional analysis of U.S. adults (≥18 years) from NHANES 2017–2018 with valid transient elastography, excluding those with missing key covariates. Lean adults were defined as BMI < 25 kg/m2 and MASLD was defined as ALT ≥ 40 U/L with ≥ 2 metabolic risk factors (TG ≥ 150 mg/dL, glucose ≥ 100 mg/dL, or low sex-specific HDL). Notably, Non-Hispanic Asians were unable to be separated from “Other Race” since not enough were captured to account for event variation. Advanced fibrosis risk was classified into three stages based on the fibrosis-4 (FIB-4) score: low (≤ 1.3), intermediate (1.31–2.67), or high ( > 2.67). FIB-4 was then evaluated across sex, age, and race/ethnicity.
Results: Among 1,105 lean adults, 253 (23%) met criteria for MASLD (Table 1). Of these, 21.3% had intermediate or high fibrosis risk. High fibrosis risk was more prevalent in males (4.5%) than females (1.7%), and combined intermediate or high fibrosis risk increased with age (2.4% in < 40 years old versus 29.7% in ≥ 60 years old). Notably, 23.1% of Non-Hispanic Black and 21.7% of Mexican American lean MASLD individuals had intermediate or high fibrosis risk (Figure 1).
Discussion: In this nationally representative cohort, male sex, Non-Hispanic Black race, and Mexican American race emerged as robust predictors of advanced fibrosis risk on transient elastography, highlighting fibrosis risk beyond obesity. These findings support expanding noninvasive fibrosis screening to all MASLD patients irrespective of BMI with particular focus on lean individuals and high-risk demographics. Longitudinal studies should validate these predictors against elastography outcomes and assess the impact of early fibrosis detection on clinical endpoints.
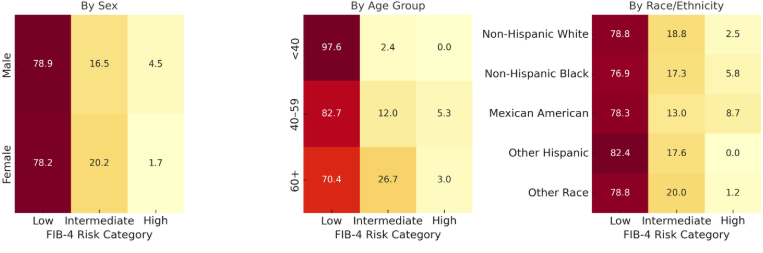
Figure: Table 1. FIB-4 fibrosis risk stratification in adults with lean MASLD
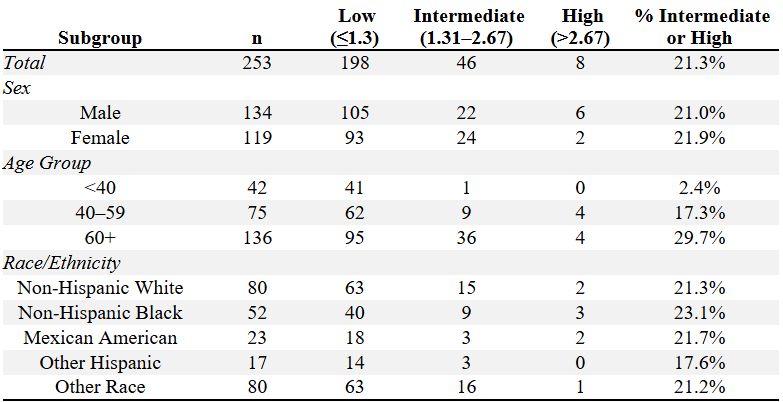
Figure: Figure 1. Heatmap summarizing FIB-4 fibrosis risk distribution among lean MASLD individuals by sex, age group, and race/ethnicity
Disclosures:
Justin-James Chua indicated no relevant financial relationships.
Nikita Garg indicated no relevant financial relationships.
Varun Jain indicated no relevant financial relationships.
Tushar Abhinav indicated no relevant financial relationships.
Shruthi Sethuraman indicated no relevant financial relationships.
Paarth Kapadia indicated no relevant financial relationships.
Nanditha Venkatesan indicated no relevant financial relationships.
Lizeth Cifuentas indicated no relevant financial relationships.
Justin-James Chua, MD1, Nikita Garg, MD2, Varun Jain, MD1, Tushar Abhinav, MD3, Shruthi Sethuraman, MD1, Paarth Kapadia, MD1, Nanditha Venkatesan, MD1, Lizeth Cifuentas, MD1. P1547 - High Fibrosis Risk in Lean Metabolic Dysfunction‐Associated Steatotic Liver Disease (MASLD): A NHANES 2017–2018 Analysis Challenging BMI-Based Screening, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
