Sunday Poster Session
Category: Liver
P1649 - Risk Stratification of Patients Admitted From the Emergency Department With Decompensated Cirrhosis
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall
- RK
Rohit Khullar, MD
Tufts Medical Center
Boston, MA
Presenting Author(s)
Rohit Khullar, MD1, Benjamin Rosen, MD1, Mohammad Almeqdadi, MD1, Raffi Karagozian, MD2
1Tufts Medical Center, Boston, MA; 2Tufts University School of Medicine, Boston, MA
Introduction: Patients with acute-on-chronic liver failure (ACLF) have 30d mortality between 25% to > 40%, highlighting the need for early identification and aggressive management of decompensated cirrhotic patients with high short-term mortality. The LIV-4 and CLIF-C ACLF scores have been previously validated to predict mortality of patients admitted to the ICU. To date, these models have not been validated on patients presenting to the emergency department (ED).
Methods: This single-center retrospective study of patients with decompensated cirrhosis admitted from the ED at Beth Israel Deaconess Medical Center between 2009 and 2022 utilized data available through the MIMIC-IV v3.1 database. Patients with decompensated cirrhosis were identified by ICD-9/10 diagnoses codes for ascites, esophageal variceal bleeding or hepatic encephalopathy. Patients were excluded with acute liver failure, no passage through the ED, or with insufficient lab or vital sign data to calculate LIV-4, CLIF-C ACLF or MELD 3.0 scores. Primary outcomes were 30d and 90d mortality. Categorical variables were analyzed with χ2 contingency tests. Performance of each risk score was measured by concordance (c)-index.
Results: Of 32,019 admissions for patients with cirrhosis, 13,714 were identified with decompensated cirrhosis. 4,697 patients passed through the ED and had sufficient data for risk score calculation. Overall, 30d mortality was 15.4% and 90d mortality was 27.6%. Among patients transferred to the ICU after 48h, mortality rates exceeded 38% after 30d and 55% after 90d, significantly higher than patients transferred within the first 48h of admission (8-29% after 30d and 20-41% after 90d, p < 0.001, χ2 contingency test, Fig 2C). The LIV-4, CLIF-C ACLF and MELD 3.0 models performed similarly in risk stratifying patients by mortality, with c-indices of 0.68, 0.75 and 0.66, respectively (Fig 2A). The top 25% of patients ranked by the LIV-4, CLIF-C ACLF and MELD 3.0 scores capture up to 59% of all deceased patients after 30 days (Fig 2B).
Discussion: All risk scores here were designed for the ICU setting but demonstrated efficacy in risk-stratifying patients with decompensated cirrhosis presenting to the ED. The CLIF-C ACLF model performed modestly better than MELD 3.0 and LIV-4 by c-index. Utilization of these risk scores would enable concentration of resources on patients with likely short-term mortality. Next steps include a prospective study to triage newly admitted cirrhotic patients for early ICU consultation.
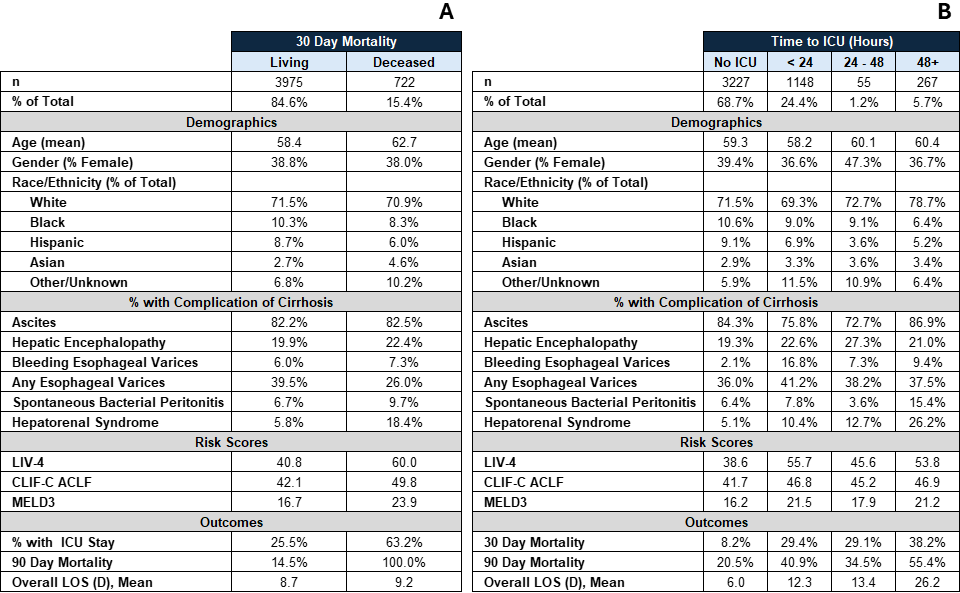
Figure: Figure 1 stratifies patient demographics, rates of various complications of cirrhosis, risk scores, mortality rates, admission length-of-stay (LOS) and rate with ICU admission by (A) 30 day mortality and (B) time from hospital admission to ICU upgrade. Ascites, hepatic encephalopathy, bleeding esophageal varices, any esophageal varices, spontaneous bacterial peritonitis and hepatorenal syndrome were identified by ICD diagnosis code
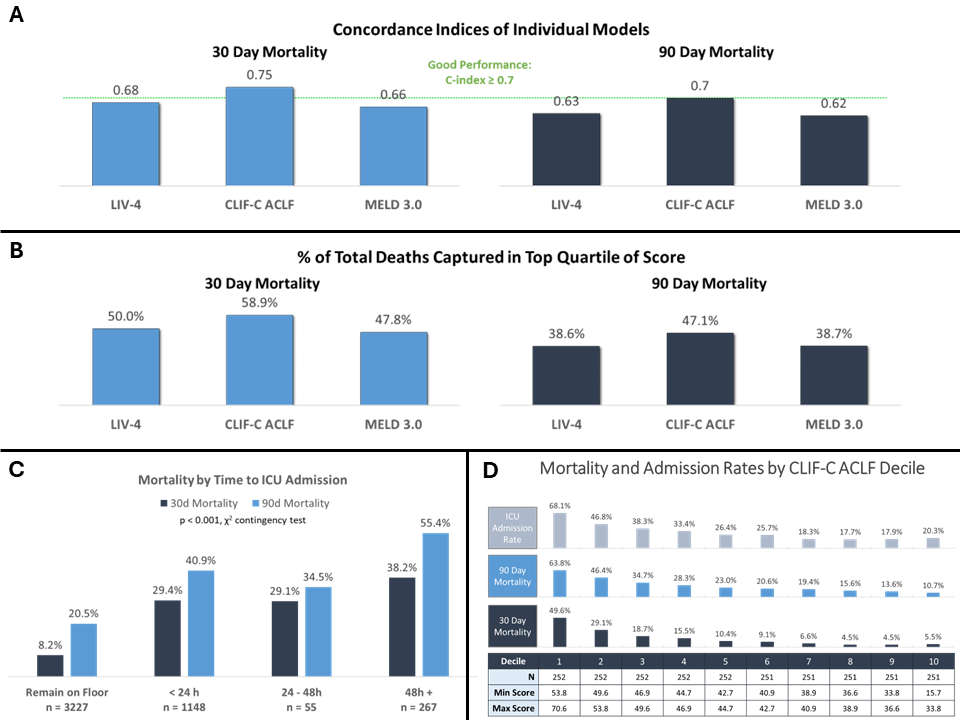
Figure: Figure 2A: Represents concordance indices for LIV-4, CLIF-C ACLF and MELD 3.0 models in discriminating 30 day and 90 day mortality rates. Figure 2B: Represents share of total deceased represented by targeting the top 25% of all patients ordered by the LIV-4, CLIF-C ACLF and MELD 3.0 scores, respectively after 30 days and 90 days. Figure 2C: Shows that patients admitted to ICU within 48 hours have lower mortality rates after 30 and 90 days than patients admitted to ICU > 48h from hospital admission. Figure 2D: Patients in deciles 1 and 2 have the highest CLIF-C ACLF scores and higher mortality rates than patients in lower deciles. Focusing resources on these groups may improve patient outcomes
Disclosures:
Rohit Khullar indicated no relevant financial relationships.
Benjamin Rosen indicated no relevant financial relationships.
Mohammad Almeqdadi indicated no relevant financial relationships.
Raffi Karagozian indicated no relevant financial relationships.
Rohit Khullar, MD1, Benjamin Rosen, MD1, Mohammad Almeqdadi, MD1, Raffi Karagozian, MD2. P1649 - Risk Stratification of Patients Admitted From the Emergency Department With Decompensated Cirrhosis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Tufts Medical Center, Boston, MA; 2Tufts University School of Medicine, Boston, MA
Introduction: Patients with acute-on-chronic liver failure (ACLF) have 30d mortality between 25% to > 40%, highlighting the need for early identification and aggressive management of decompensated cirrhotic patients with high short-term mortality. The LIV-4 and CLIF-C ACLF scores have been previously validated to predict mortality of patients admitted to the ICU. To date, these models have not been validated on patients presenting to the emergency department (ED).
Methods: This single-center retrospective study of patients with decompensated cirrhosis admitted from the ED at Beth Israel Deaconess Medical Center between 2009 and 2022 utilized data available through the MIMIC-IV v3.1 database. Patients with decompensated cirrhosis were identified by ICD-9/10 diagnoses codes for ascites, esophageal variceal bleeding or hepatic encephalopathy. Patients were excluded with acute liver failure, no passage through the ED, or with insufficient lab or vital sign data to calculate LIV-4, CLIF-C ACLF or MELD 3.0 scores. Primary outcomes were 30d and 90d mortality. Categorical variables were analyzed with χ2 contingency tests. Performance of each risk score was measured by concordance (c)-index.
Results: Of 32,019 admissions for patients with cirrhosis, 13,714 were identified with decompensated cirrhosis. 4,697 patients passed through the ED and had sufficient data for risk score calculation. Overall, 30d mortality was 15.4% and 90d mortality was 27.6%. Among patients transferred to the ICU after 48h, mortality rates exceeded 38% after 30d and 55% after 90d, significantly higher than patients transferred within the first 48h of admission (8-29% after 30d and 20-41% after 90d, p < 0.001, χ2 contingency test, Fig 2C). The LIV-4, CLIF-C ACLF and MELD 3.0 models performed similarly in risk stratifying patients by mortality, with c-indices of 0.68, 0.75 and 0.66, respectively (Fig 2A). The top 25% of patients ranked by the LIV-4, CLIF-C ACLF and MELD 3.0 scores capture up to 59% of all deceased patients after 30 days (Fig 2B).
Discussion: All risk scores here were designed for the ICU setting but demonstrated efficacy in risk-stratifying patients with decompensated cirrhosis presenting to the ED. The CLIF-C ACLF model performed modestly better than MELD 3.0 and LIV-4 by c-index. Utilization of these risk scores would enable concentration of resources on patients with likely short-term mortality. Next steps include a prospective study to triage newly admitted cirrhotic patients for early ICU consultation.
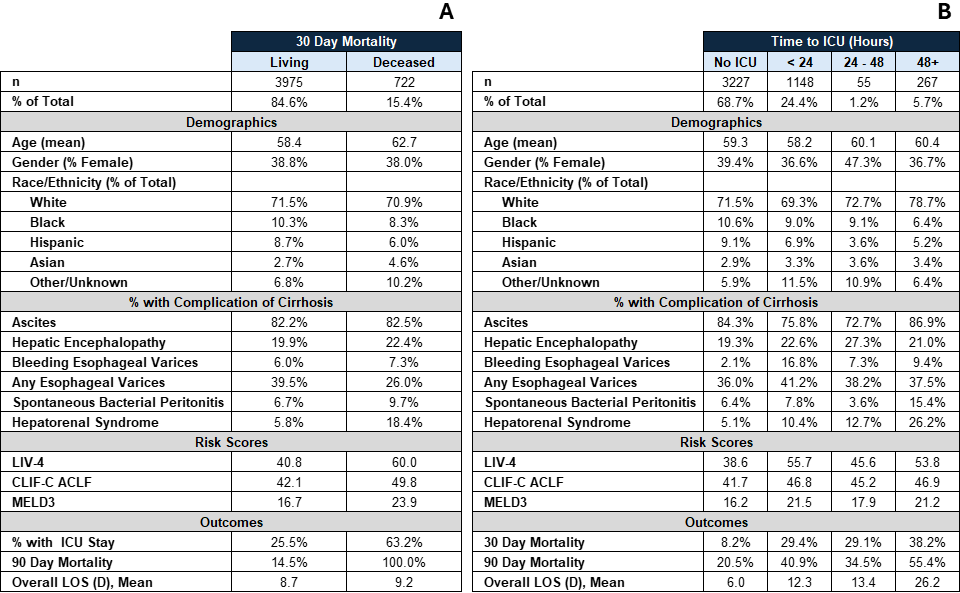
Figure: Figure 1 stratifies patient demographics, rates of various complications of cirrhosis, risk scores, mortality rates, admission length-of-stay (LOS) and rate with ICU admission by (A) 30 day mortality and (B) time from hospital admission to ICU upgrade. Ascites, hepatic encephalopathy, bleeding esophageal varices, any esophageal varices, spontaneous bacterial peritonitis and hepatorenal syndrome were identified by ICD diagnosis code
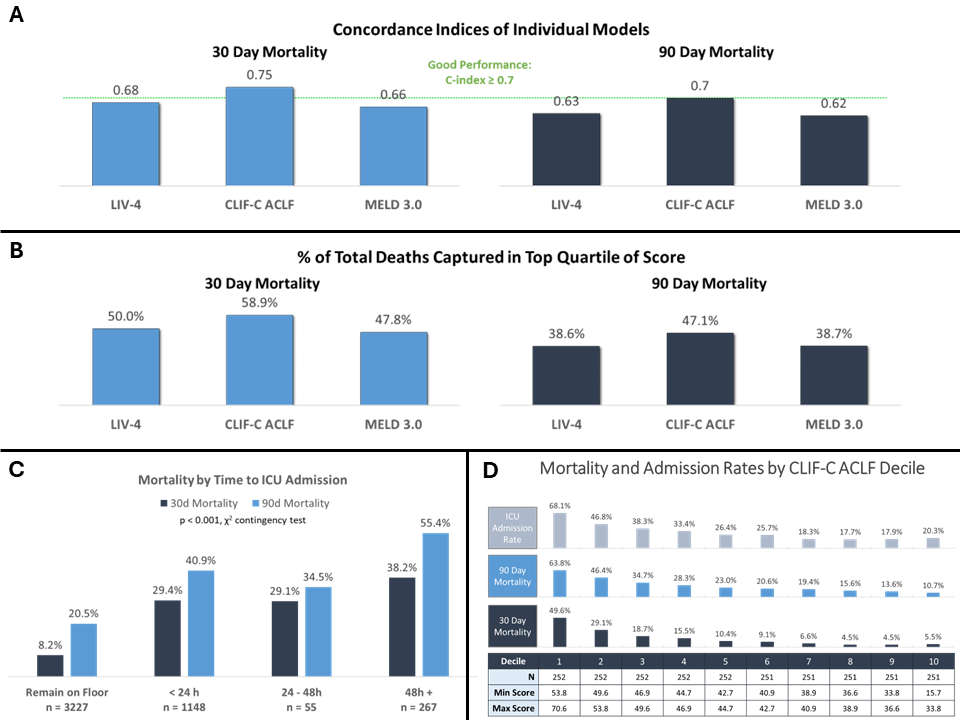
Figure: Figure 2A: Represents concordance indices for LIV-4, CLIF-C ACLF and MELD 3.0 models in discriminating 30 day and 90 day mortality rates. Figure 2B: Represents share of total deceased represented by targeting the top 25% of all patients ordered by the LIV-4, CLIF-C ACLF and MELD 3.0 scores, respectively after 30 days and 90 days. Figure 2C: Shows that patients admitted to ICU within 48 hours have lower mortality rates after 30 and 90 days than patients admitted to ICU > 48h from hospital admission. Figure 2D: Patients in deciles 1 and 2 have the highest CLIF-C ACLF scores and higher mortality rates than patients in lower deciles. Focusing resources on these groups may improve patient outcomes
Disclosures:
Rohit Khullar indicated no relevant financial relationships.
Benjamin Rosen indicated no relevant financial relationships.
Mohammad Almeqdadi indicated no relevant financial relationships.
Raffi Karagozian indicated no relevant financial relationships.
Rohit Khullar, MD1, Benjamin Rosen, MD1, Mohammad Almeqdadi, MD1, Raffi Karagozian, MD2. P1649 - Risk Stratification of Patients Admitted From the Emergency Department With Decompensated Cirrhosis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
