Sunday Poster Session
Category: Liver
P1648 - A Comparative and Descriptive Analysis of Non-Viral Liver Cancer Trends in the US From 1999 – 2020
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall

Ibukunoluwa Oshobu, MD, MPH (she/her/hers)
University of Missouri Health Care
Columbia, MO
Presenting Author(s)
Ibukunoluwa Oshobu, MD, MPH1, Nourhan Saleh, MD1, Bright Nwatamole, MBBS2, Mary Iwuagwu, MD3, Adedeji Okikiade, MD, PhD, MBA4
1University of Missouri Health Care, Columbia, MO; 2Vassar Brothers Medical Center - Nuvance Health, Poughkeepsie, NY; 3All Saints University, School of Medicine, Chicago, IL; 4California Northstate University, Elk Grove, CA
Introduction: Non-viral liver cancer, particularly hepatocellular carcinoma (HCC), accounts for 90% of liver cancer cases and is the sixth most common cancer globally. With the advent of vaccines and therapeutic measures viral HCC has declined. However, non-viral etiologies such as nonalcoholic fatty liver disease (NAFLD) and alcohol-associated liver disease (ALD) are on the rise. At a population level, we aimed to evaluate temporal trends in non-viral HCC mortality across U.S. populations, focusing on demographic and regional disparities.
Methods: We conducted a retrospective analysis of the 1999-2020 CDC WONDER mortality data (n = 136,101,150). JoinPoint Regression assessed the temporal trends in liver cancer mortality in the age-adjusted mortality rates stratified by sex, race (White, Black, Asian/Pacific Islander), and Health and Human Services (HHS) regions. The Annual Percent Change (APC) and Average Annual Percent Change (AAPC) with 95% confidence intervals (CI) and p-values were calculated.
Results: White males aged 55-64 consistently exhibited the highest liver cancer mortality rates across all HHS regions, with female rates remaining approximately 1 per 100,000. HHS Region 9 had the highest overall liver cancer mortality rate at 23.3%, with a significant APC of 10.42% (95% CI: 8.34–13.10). Region 4 and Region 6 followed at 15.7% and 14.7%, respectively. In Region 9, male liver cancer mortality increased from 2007–2017 (7.5%; 95% CI: 3.6–31.2; p = 0.015). Region 6 males experienced a significant rise from 2000–2015 (12.6%; 95% CI: 10.1–17.9; p < 0.001), followed by a decline from 2015–2020 (APC -6.7%; 95% CI: -30.3 to 4.4; p = 0.20). Black males in Regions 3 and 6 showed rising trends with APCs of 5.83% (95% CI: 0.53–11.27) and 6.77% (95% CI: 3.85–9.84), respectively. In contrast, Asian/Pacific Islander males in Region 9 demonstrated a non-significant decrease (APC -4.21%; 95% CI: -9.51 to 1.46).
Discussion: Non-viral liver cancer mortality has been rising disproportionately among older white and Black males in several U.S. regions, notably HHS Regions 6 and 9 over the last two decades. This correlates with the trend of nonalcoholic fatty liver disease (NAFLD) and alcohol-associated liver disease (ALD). Factors contributing are multifactorial, gender disparities, socioeconomic disparities. Recommended intervention are aspirin, statins, lifestyle modifications, and increased surveillance. There is an increased need for public health intervention in at-risk groups mainly the male population.
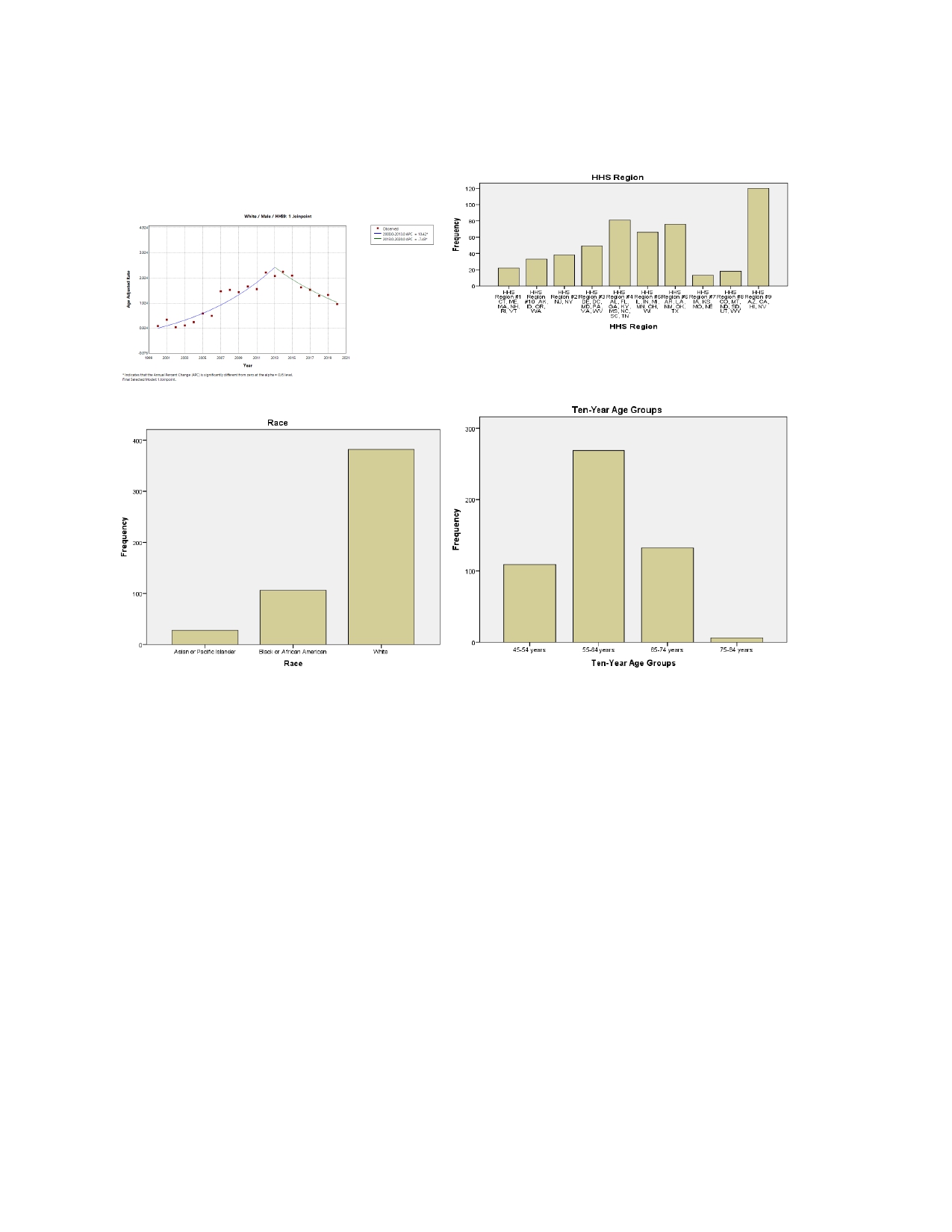
Figure: Figure 1: Illustrates the graphical representation of disparities
Disclosures:
Ibukunoluwa Oshobu indicated no relevant financial relationships.
Nourhan Saleh indicated no relevant financial relationships.
Bright Nwatamole indicated no relevant financial relationships.
Mary Iwuagwu indicated no relevant financial relationships.
Adedeji Okikiade indicated no relevant financial relationships.
Ibukunoluwa Oshobu, MD, MPH1, Nourhan Saleh, MD1, Bright Nwatamole, MBBS2, Mary Iwuagwu, MD3, Adedeji Okikiade, MD, PhD, MBA4. P1648 - A Comparative and Descriptive Analysis of Non-Viral Liver Cancer Trends in the US From 1999 – 2020, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1University of Missouri Health Care, Columbia, MO; 2Vassar Brothers Medical Center - Nuvance Health, Poughkeepsie, NY; 3All Saints University, School of Medicine, Chicago, IL; 4California Northstate University, Elk Grove, CA
Introduction: Non-viral liver cancer, particularly hepatocellular carcinoma (HCC), accounts for 90% of liver cancer cases and is the sixth most common cancer globally. With the advent of vaccines and therapeutic measures viral HCC has declined. However, non-viral etiologies such as nonalcoholic fatty liver disease (NAFLD) and alcohol-associated liver disease (ALD) are on the rise. At a population level, we aimed to evaluate temporal trends in non-viral HCC mortality across U.S. populations, focusing on demographic and regional disparities.
Methods: We conducted a retrospective analysis of the 1999-2020 CDC WONDER mortality data (n = 136,101,150). JoinPoint Regression assessed the temporal trends in liver cancer mortality in the age-adjusted mortality rates stratified by sex, race (White, Black, Asian/Pacific Islander), and Health and Human Services (HHS) regions. The Annual Percent Change (APC) and Average Annual Percent Change (AAPC) with 95% confidence intervals (CI) and p-values were calculated.
Results: White males aged 55-64 consistently exhibited the highest liver cancer mortality rates across all HHS regions, with female rates remaining approximately 1 per 100,000. HHS Region 9 had the highest overall liver cancer mortality rate at 23.3%, with a significant APC of 10.42% (95% CI: 8.34–13.10). Region 4 and Region 6 followed at 15.7% and 14.7%, respectively. In Region 9, male liver cancer mortality increased from 2007–2017 (7.5%; 95% CI: 3.6–31.2; p = 0.015). Region 6 males experienced a significant rise from 2000–2015 (12.6%; 95% CI: 10.1–17.9; p < 0.001), followed by a decline from 2015–2020 (APC -6.7%; 95% CI: -30.3 to 4.4; p = 0.20). Black males in Regions 3 and 6 showed rising trends with APCs of 5.83% (95% CI: 0.53–11.27) and 6.77% (95% CI: 3.85–9.84), respectively. In contrast, Asian/Pacific Islander males in Region 9 demonstrated a non-significant decrease (APC -4.21%; 95% CI: -9.51 to 1.46).
Discussion: Non-viral liver cancer mortality has been rising disproportionately among older white and Black males in several U.S. regions, notably HHS Regions 6 and 9 over the last two decades. This correlates with the trend of nonalcoholic fatty liver disease (NAFLD) and alcohol-associated liver disease (ALD). Factors contributing are multifactorial, gender disparities, socioeconomic disparities. Recommended intervention are aspirin, statins, lifestyle modifications, and increased surveillance. There is an increased need for public health intervention in at-risk groups mainly the male population.
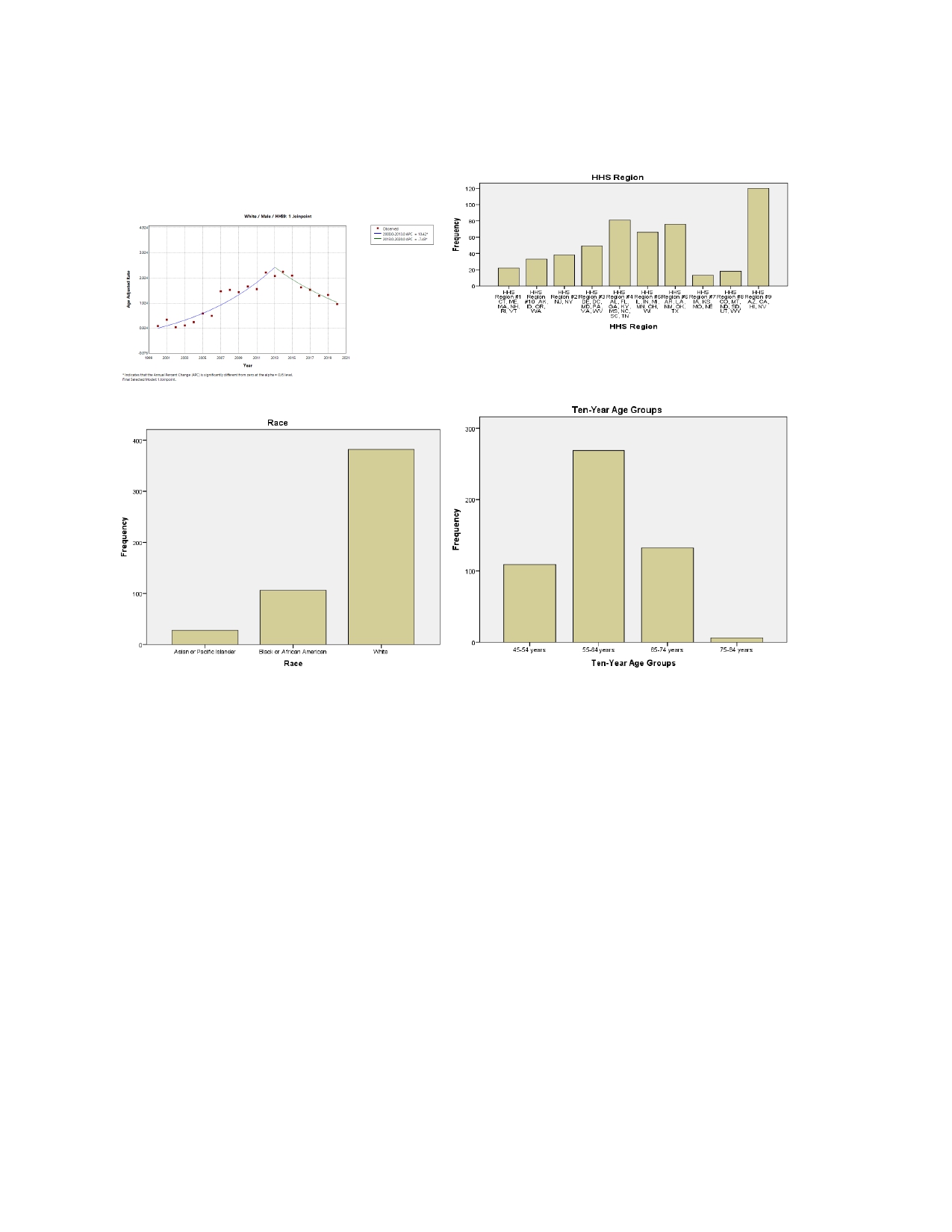
Figure: Figure 1: Illustrates the graphical representation of disparities
Disclosures:
Ibukunoluwa Oshobu indicated no relevant financial relationships.
Nourhan Saleh indicated no relevant financial relationships.
Bright Nwatamole indicated no relevant financial relationships.
Mary Iwuagwu indicated no relevant financial relationships.
Adedeji Okikiade indicated no relevant financial relationships.
Ibukunoluwa Oshobu, MD, MPH1, Nourhan Saleh, MD1, Bright Nwatamole, MBBS2, Mary Iwuagwu, MD3, Adedeji Okikiade, MD, PhD, MBA4. P1648 - A Comparative and Descriptive Analysis of Non-Viral Liver Cancer Trends in the US From 1999 – 2020, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
