Sunday Poster Session
Category: Liver
P1645 - BMI Does Not Predict Advanced Fibrosis in Non-Obese Adults With Hepatic Steatosis
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall
- VP
Vinathi Polamraju, MD
Washington University School of Medicine in St. Louis / Barnes-Jewish Hospital
St. Louis, MO
Presenting Author(s)
Vinathi Polamraju, MD1, Kamilah Scales, MD2, Peter McDonnell, MD1, Scott McHenry, MD, MSc1, Cassandra D.L. Fritz, MD, MPHS3
1Washington University School of Medicine in St. Louis / Barnes-Jewish Hospital, St. Louis, MO; 2Washington University School of Medicine in St. Louis, St. Louis, MO; 3Washington University School of Medicine in St. Louis / Barnes-Jewish Hospital, Saint Louis, MO
Introduction: Cryptogenic steatotic liver disease (CSLD) and metabolic dysfunction-associated steatotic liver disease (MASLD) both involve fat accumulation in the liver but differ in etiology. CSLD is recognized as distinct from MASLD based on clinical and pathological features. The redefinition of MASLD emphasizes metabolic dysfunction, but the role of BMI in predicting disease severity in non-obese individuals (BMI < 30 kg/m²) is unclear.
Methods: This retrospective single-center study included 214 adult primary care patients with BMI < 30 kg/m² and hepatic steatosis on imaging, excluding those with significant alcohol use or secondary liver disease. MASLD was defined by hepatic steatosis plus ≥2 cardiometabolic risk factors (hypertension, hyperlipidemia, prediabetes) or type 2 diabetes alone. CSLD was defined by hepatic steatosis with 0–1 cardiometabolic risk factors. Fibrosis was assessed using the Fib-4 index (≥2.67 implying advanced fibrosis). BMI was evaluated as both a binary (< 25 vs. ≥25 kg/m²) and continuous variable. Multivariable logistic regression, with backward stepwise selection, identified significant independent predictors of advanced fibrosis. The model adjusted for BMI, race, sex, hypertension, glycemic status, and lipid status.
Results: The Mantel-Haenszel chi-squared test assessed whether BMI influenced the relationship between liver fibrosis and etiology (MASLD vs idiopathic steatosis). For those with BMI < 25 kg/m², there was no significant association between fibrosis and etiology (aOR 0.74[95% CI: 0.19–2.93],p = 0.763). Similarly, in those with BMI ≥25 kg/m², there was no significant association between fibrosis and etiology (aOR = 1.15[95% CI: 0.4–3.2],p = 0.814). For MASLD and CSLD patients, multivariable logistic regression analysis identified hyperlipidemia with hypertriglyceridemia as a significant factor for advanced fibrosis (OR = 1.291[95% CI: 1.079–2.838],p = 0.0358) (Fig 1). However, BMI was not a significant predictor of advanced fibrosis. While univariate analysis suggested African American race may be protective against advanced fibrosis (p = 0.045), this was not significant in the multivariable model (Fig 2).
Discussion: In non-obese individuals with hepatic steatosis, BMI is not an independent predictor of advanced fibrosis regardless of etiology. These findings support a shift away from BMI-centered evaluation and prioritizing metabolic risk factors—particularly dyslipidemia—in fatty liver disease management.
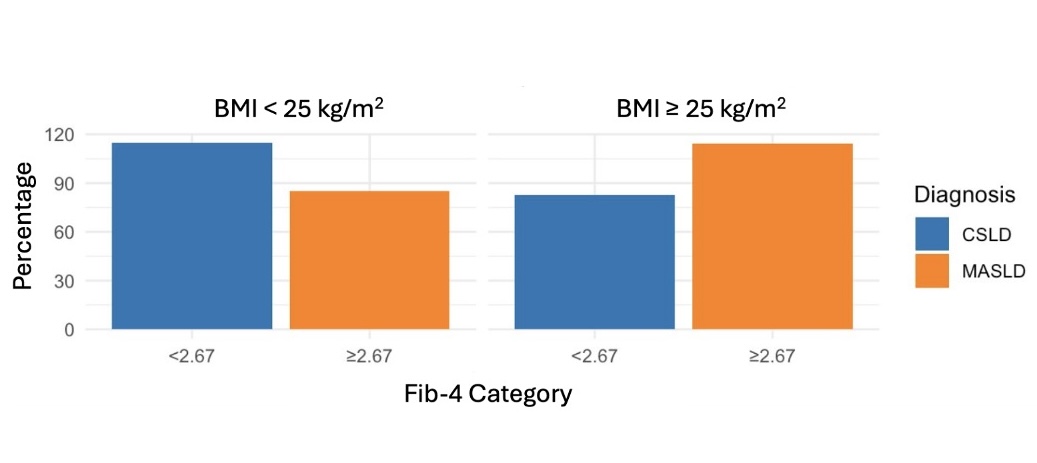
Figure: BMI Does Not Significantly Modify the Association Between Fibrosis Severity and Etiology of Steatotic Liver Disease
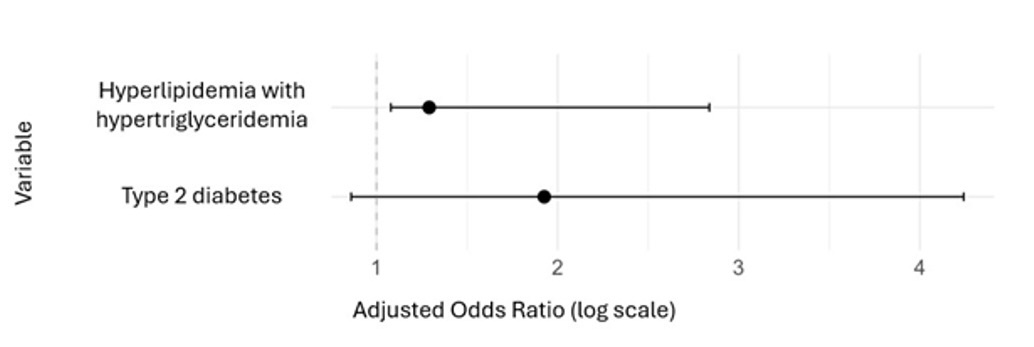
Figure: Independent Predictors of Advanced Fibrosis Among Non-Obese Patients with MASLD and CSLD
*Multivariable logistic regression analysis adjusted for body mass index (BMI), race (White,
African American, Asian), sex, hypertension, glycemic control (normoglycemia, pre-diabetes,
type 2 diabetes), and lipid control (normal, hyperlipidemia with or without hypertriglyceridemia).
Disclosures:
Vinathi Polamraju indicated no relevant financial relationships.
Kamilah Scales indicated no relevant financial relationships.
Peter McDonnell indicated no relevant financial relationships.
Scott McHenry indicated no relevant financial relationships.
Cassandra Fritz indicated no relevant financial relationships.
Vinathi Polamraju, MD1, Kamilah Scales, MD2, Peter McDonnell, MD1, Scott McHenry, MD, MSc1, Cassandra D.L. Fritz, MD, MPHS3. P1645 - BMI Does Not Predict Advanced Fibrosis in Non-Obese Adults With Hepatic Steatosis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Washington University School of Medicine in St. Louis / Barnes-Jewish Hospital, St. Louis, MO; 2Washington University School of Medicine in St. Louis, St. Louis, MO; 3Washington University School of Medicine in St. Louis / Barnes-Jewish Hospital, Saint Louis, MO
Introduction: Cryptogenic steatotic liver disease (CSLD) and metabolic dysfunction-associated steatotic liver disease (MASLD) both involve fat accumulation in the liver but differ in etiology. CSLD is recognized as distinct from MASLD based on clinical and pathological features. The redefinition of MASLD emphasizes metabolic dysfunction, but the role of BMI in predicting disease severity in non-obese individuals (BMI < 30 kg/m²) is unclear.
Methods: This retrospective single-center study included 214 adult primary care patients with BMI < 30 kg/m² and hepatic steatosis on imaging, excluding those with significant alcohol use or secondary liver disease. MASLD was defined by hepatic steatosis plus ≥2 cardiometabolic risk factors (hypertension, hyperlipidemia, prediabetes) or type 2 diabetes alone. CSLD was defined by hepatic steatosis with 0–1 cardiometabolic risk factors. Fibrosis was assessed using the Fib-4 index (≥2.67 implying advanced fibrosis). BMI was evaluated as both a binary (< 25 vs. ≥25 kg/m²) and continuous variable. Multivariable logistic regression, with backward stepwise selection, identified significant independent predictors of advanced fibrosis. The model adjusted for BMI, race, sex, hypertension, glycemic status, and lipid status.
Results: The Mantel-Haenszel chi-squared test assessed whether BMI influenced the relationship between liver fibrosis and etiology (MASLD vs idiopathic steatosis). For those with BMI < 25 kg/m², there was no significant association between fibrosis and etiology (aOR 0.74[95% CI: 0.19–2.93],p = 0.763). Similarly, in those with BMI ≥25 kg/m², there was no significant association between fibrosis and etiology (aOR = 1.15[95% CI: 0.4–3.2],p = 0.814). For MASLD and CSLD patients, multivariable logistic regression analysis identified hyperlipidemia with hypertriglyceridemia as a significant factor for advanced fibrosis (OR = 1.291[95% CI: 1.079–2.838],p = 0.0358) (Fig 1). However, BMI was not a significant predictor of advanced fibrosis. While univariate analysis suggested African American race may be protective against advanced fibrosis (p = 0.045), this was not significant in the multivariable model (Fig 2).
Discussion: In non-obese individuals with hepatic steatosis, BMI is not an independent predictor of advanced fibrosis regardless of etiology. These findings support a shift away from BMI-centered evaluation and prioritizing metabolic risk factors—particularly dyslipidemia—in fatty liver disease management.
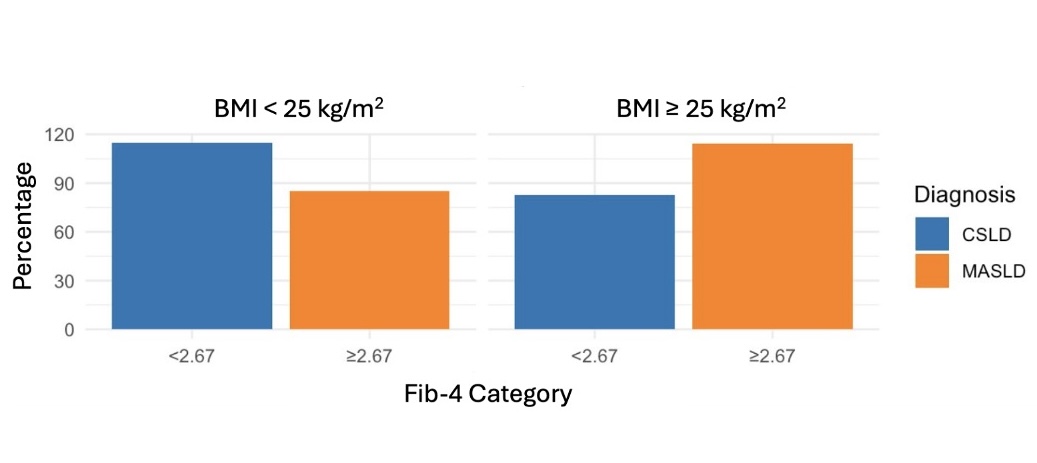
Figure: BMI Does Not Significantly Modify the Association Between Fibrosis Severity and Etiology of Steatotic Liver Disease
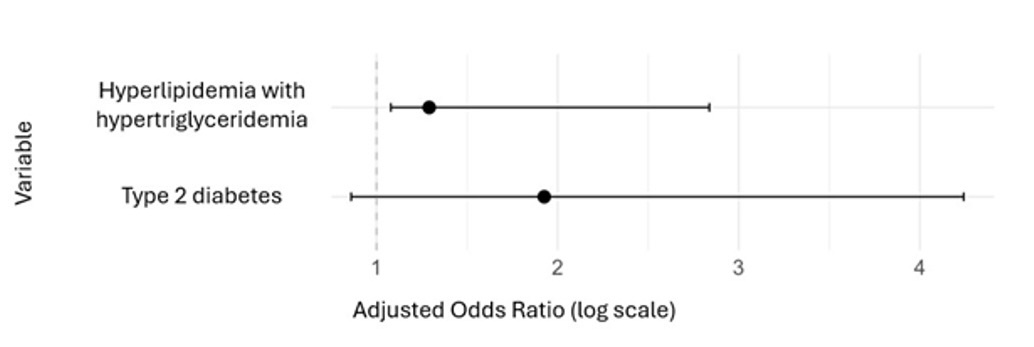
Figure: Independent Predictors of Advanced Fibrosis Among Non-Obese Patients with MASLD and CSLD
*Multivariable logistic regression analysis adjusted for body mass index (BMI), race (White,
African American, Asian), sex, hypertension, glycemic control (normoglycemia, pre-diabetes,
type 2 diabetes), and lipid control (normal, hyperlipidemia with or without hypertriglyceridemia).
Disclosures:
Vinathi Polamraju indicated no relevant financial relationships.
Kamilah Scales indicated no relevant financial relationships.
Peter McDonnell indicated no relevant financial relationships.
Scott McHenry indicated no relevant financial relationships.
Cassandra Fritz indicated no relevant financial relationships.
Vinathi Polamraju, MD1, Kamilah Scales, MD2, Peter McDonnell, MD1, Scott McHenry, MD, MSc1, Cassandra D.L. Fritz, MD, MPHS3. P1645 - BMI Does Not Predict Advanced Fibrosis in Non-Obese Adults With Hepatic Steatosis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
