Sunday Poster Session
Category: Liver
P1860 - Unexpected Detection of Primary Hepatic Angiosarcoma in a Car Mechanic With Ulcerative Colitis
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall
- BK
Bhupinder Kaur, MD
University of Arizona College of Medicine, Phoenix VA Medical Center
Phoenix, AZ
Presenting Author(s)
Award: ACG Presidential Poster Award
Bhupinder Kaur, MD1, Adnan Malik, MD2, Mohamed Mostafa, MD3, Karn Wijarnpreecha, MD, MPH1
1University of Arizona College of Medicine, Phoenix VA Medical Center, Phoenix, AZ; 2HonorHealth, Mesa, AZ; 3Banner University Medical Center, Phoenix, AZ
Introduction: Angiosarcomas are rare soft-tissue sarcomas of endothelial cell origin that have a poor prognosis. Primary hepatic angiosarcoma (HA) accounts for approximately 2% of all liver tumors, yet it is considered the third most common primary hepatic malignancy, following hepatocellular carcinoma and cholangiocarcinoma. This case highlights an unexpected diagnosis of primary HA in a patient with ulcerative colitis and potential vinyl chloride exposure through occupational work as a car mechanic.
Case Description/
Methods: A 60-year-old male with ulcerative colitis (UC) presented with two months of right upper quadrant (RUQ) abdominal pain and jaundice. Physical exam was notable for jaundice, abdominal distension with RUQ tenderness, and prominent hepatomegaly. Lab results showed hemoglobin 7.8 g/dL, platelets 201 K/u, total bilirubin 10.3 mg/dL and direct bilirubin 7.9 mg/dL. Magnetic resonance imaging with and without contrast showed an enlarged liver mass with diffusely infiltrative process with countless lesions ranging from 1 cm to 10 cm (Image 1). Ultimately, liver biopsy revealed HA (Image 2). Given patient’s aggressive tumor burden, hospice care was recommended.
Discussion: HA has a nonspecific presentation including abdominal pain, weight loss, and fatigue with a rapid progression of disease. It is linked to toxins like vinyl chloride and steroids, but most cases lack clear causes. Indirect exposure (e.g., PVC in automechanics) may pose risks. Although UC is associated to some liver cancers, no clear connection to HA has been identified. The most common laboratory abnormalities include anemia and thrombocytopenia, which are thought to result from the consumption of clotting factors. Abdominal imaging in HA typically shows multiple heterogeneous masses with hemorrhage, necrosis, or cavitation, often invading liver parenchyma, vessels, and nearby structures. Diagnosis relies on histopathology and immunohistochemistry, with biopsy showing epithelioid to spindled neoplasms and varied vascular patterns. Given its rarity and poor prognosis (median survival 6–12 months), HA lacks standardized management guidelines. Surgical resection may be possible if localized and liver function is preserved, though it is often limited by vascular invasion. Chemotherapy responses are typically limited and non-curative. Early diagnosis is crucial, and further research is needed to establish standardized diagnostic and management guidelines.
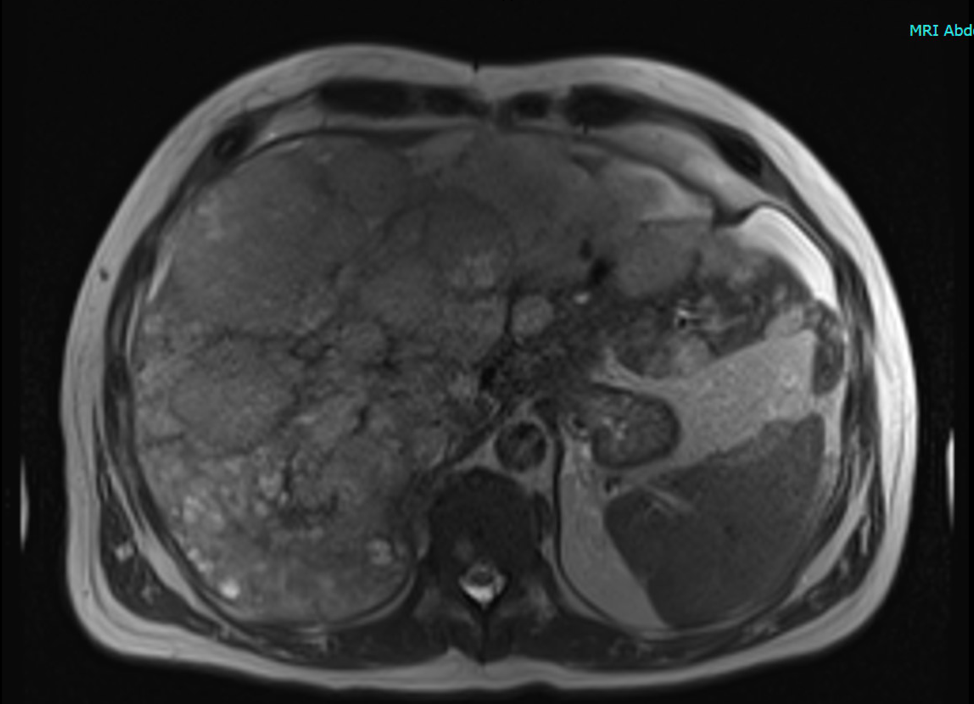
Figure: Image 1. Magnetic resonance imaging with and without contrast showing extensive liver lesions with heterogenous pattern, hypointensity, and capsular retraction.

Figure: Image 2. Ultrasound guided biopsy of the liver. A. 5x tumor and adjacent liver with dilated sinusoids. B. Erythroblast transformation-specific-related gene (ERG) positive stain. C. 20X Spindle Cells. D. CD31 biomarker positive staining in brown.
Disclosures:
Bhupinder Kaur indicated no relevant financial relationships.
Adnan Malik indicated no relevant financial relationships.
Mohamed Mostafa indicated no relevant financial relationships.
Karn Wijarnpreecha indicated no relevant financial relationships.
Bhupinder Kaur, MD1, Adnan Malik, MD2, Mohamed Mostafa, MD3, Karn Wijarnpreecha, MD, MPH1. P1860 - Unexpected Detection of Primary Hepatic Angiosarcoma in a Car Mechanic With Ulcerative Colitis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
Bhupinder Kaur, MD1, Adnan Malik, MD2, Mohamed Mostafa, MD3, Karn Wijarnpreecha, MD, MPH1
1University of Arizona College of Medicine, Phoenix VA Medical Center, Phoenix, AZ; 2HonorHealth, Mesa, AZ; 3Banner University Medical Center, Phoenix, AZ
Introduction: Angiosarcomas are rare soft-tissue sarcomas of endothelial cell origin that have a poor prognosis. Primary hepatic angiosarcoma (HA) accounts for approximately 2% of all liver tumors, yet it is considered the third most common primary hepatic malignancy, following hepatocellular carcinoma and cholangiocarcinoma. This case highlights an unexpected diagnosis of primary HA in a patient with ulcerative colitis and potential vinyl chloride exposure through occupational work as a car mechanic.
Case Description/
Methods: A 60-year-old male with ulcerative colitis (UC) presented with two months of right upper quadrant (RUQ) abdominal pain and jaundice. Physical exam was notable for jaundice, abdominal distension with RUQ tenderness, and prominent hepatomegaly. Lab results showed hemoglobin 7.8 g/dL, platelets 201 K/u, total bilirubin 10.3 mg/dL and direct bilirubin 7.9 mg/dL. Magnetic resonance imaging with and without contrast showed an enlarged liver mass with diffusely infiltrative process with countless lesions ranging from 1 cm to 10 cm (Image 1). Ultimately, liver biopsy revealed HA (Image 2). Given patient’s aggressive tumor burden, hospice care was recommended.
Discussion: HA has a nonspecific presentation including abdominal pain, weight loss, and fatigue with a rapid progression of disease. It is linked to toxins like vinyl chloride and steroids, but most cases lack clear causes. Indirect exposure (e.g., PVC in automechanics) may pose risks. Although UC is associated to some liver cancers, no clear connection to HA has been identified. The most common laboratory abnormalities include anemia and thrombocytopenia, which are thought to result from the consumption of clotting factors. Abdominal imaging in HA typically shows multiple heterogeneous masses with hemorrhage, necrosis, or cavitation, often invading liver parenchyma, vessels, and nearby structures. Diagnosis relies on histopathology and immunohistochemistry, with biopsy showing epithelioid to spindled neoplasms and varied vascular patterns. Given its rarity and poor prognosis (median survival 6–12 months), HA lacks standardized management guidelines. Surgical resection may be possible if localized and liver function is preserved, though it is often limited by vascular invasion. Chemotherapy responses are typically limited and non-curative. Early diagnosis is crucial, and further research is needed to establish standardized diagnostic and management guidelines.
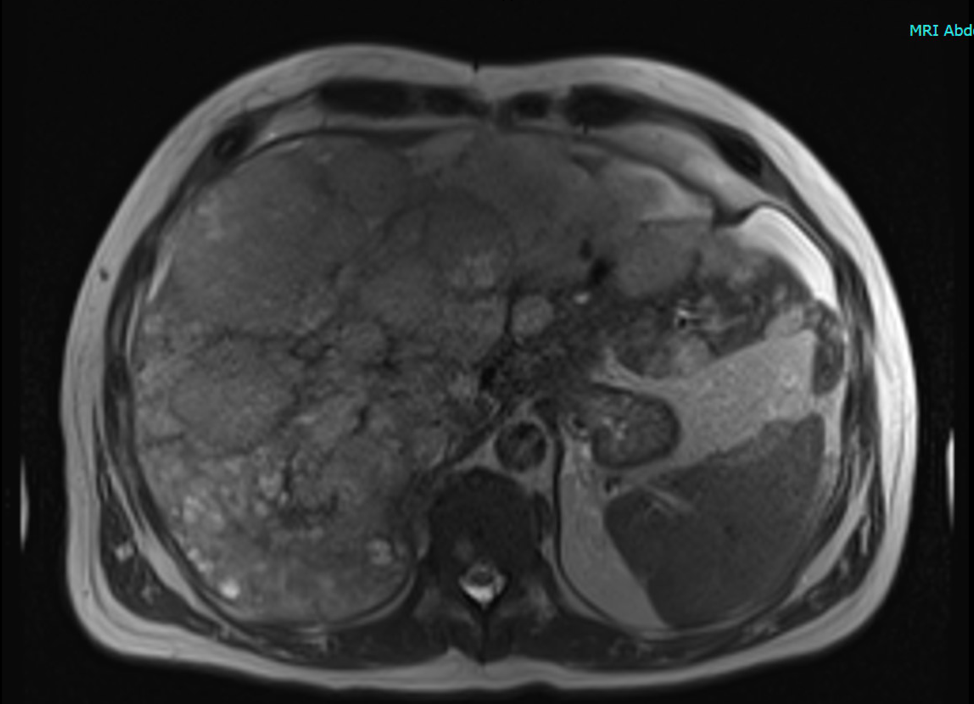
Figure: Image 1. Magnetic resonance imaging with and without contrast showing extensive liver lesions with heterogenous pattern, hypointensity, and capsular retraction.

Figure: Image 2. Ultrasound guided biopsy of the liver. A. 5x tumor and adjacent liver with dilated sinusoids. B. Erythroblast transformation-specific-related gene (ERG) positive stain. C. 20X Spindle Cells. D. CD31 biomarker positive staining in brown.
Disclosures:
Bhupinder Kaur indicated no relevant financial relationships.
Adnan Malik indicated no relevant financial relationships.
Mohamed Mostafa indicated no relevant financial relationships.
Karn Wijarnpreecha indicated no relevant financial relationships.
Bhupinder Kaur, MD1, Adnan Malik, MD2, Mohamed Mostafa, MD3, Karn Wijarnpreecha, MD, MPH1. P1860 - Unexpected Detection of Primary Hepatic Angiosarcoma in a Car Mechanic With Ulcerative Colitis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.


