Sunday Poster Session
Category: Small Intestine
P1953 - The Hidden Burden: Incidentally Uncovered Extensive Duodenal Polyposis Presenting as Postoperative Biliary Complication in Familial Adenomatous Polyposis (FAP)
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall

Garvita Singhal, MD (she/her/hers)
Tucson Medical Center (TMC)
Tucson, AZ
Presenting Author(s)
Garvita Singhal, MD, Craig Gross, MD, Karen Drenner, NP
Tucson Medical Center (TMC), Tucson, AZ
Introduction: Familial adenomatous polyposis (FAP) is an autosomal dominant colorectal cancer syndrome marked by early-onset colorectal polyps and near-certain cancer risk without prophylactic colectomy. As patients live longer post-colectomy, extracolonic manifestations—particularly duodenal and periampullary adenomas—have emerged as major sources of morbidity and mortality. Up to 90% of FAP patients develop duodenal polyps, with potential progression to adenocarcinoma. We present a case of extensive duodenal polyposis discovered incidentally after a postoperative complication, highlighting missed surveillance and questioning current screening paradigms.
Case Description/
Methods: A 70-year-old woman with FAP and prior near-total colectomy for colorectal cancer presented with fever, nausea, and right upper quadrant pain. Imaging showed acute cholecystitis. She underwent laparoscopic cholecystectomy, converted to open due to adhesions. Postoperatively, she developed bilious output in closed suction surgical drain and small bowel obstruction. ERCP was attempted for presumed bile leak but was aborted upon encountering extensive, carpet-like duodenal polyposis involving the bulb, second/third portions and likely further. The ampulla of Vater could not be visualized due to adenomatous overgrowth. Biopsies revealed tubular adenomas. No EUS was available. The patient had not undergone upper GI surveillance since her colectomy. She was referred to a tertiary center for EUS and hepatobiliary evaluation. Pancreaticoduodenectomy is under consideration given the extent and malignant potential of polyposis.
Discussion: This case underscores a silent yet serious complication of FAP—advanced duodenal polyposis discovered only due to a surgical complication. While duodenal adenomas are common in FAP, carpet-like polyposis is rare and typically indicates advanced disease with high malignant risk. Though Spigelman staging remains the primary risk stratification tool, emerging data suggest limited sensitivity, particularly for ampullary or deeply infiltrative lesions. This case exemplifies the need for lifelong, structured surveillance in FAP patients, especially as they age. Alarmingly, the patient never underwent germline APC testing; her mother and maternal grandmother, both with FAP, were also untested. This underscores gaps in genetic counseling and cascade testing. Clinicians must prioritize sustained follow-up, patient education, and family-based screening to prevent delayed diagnosis of serious extracolonic disease.
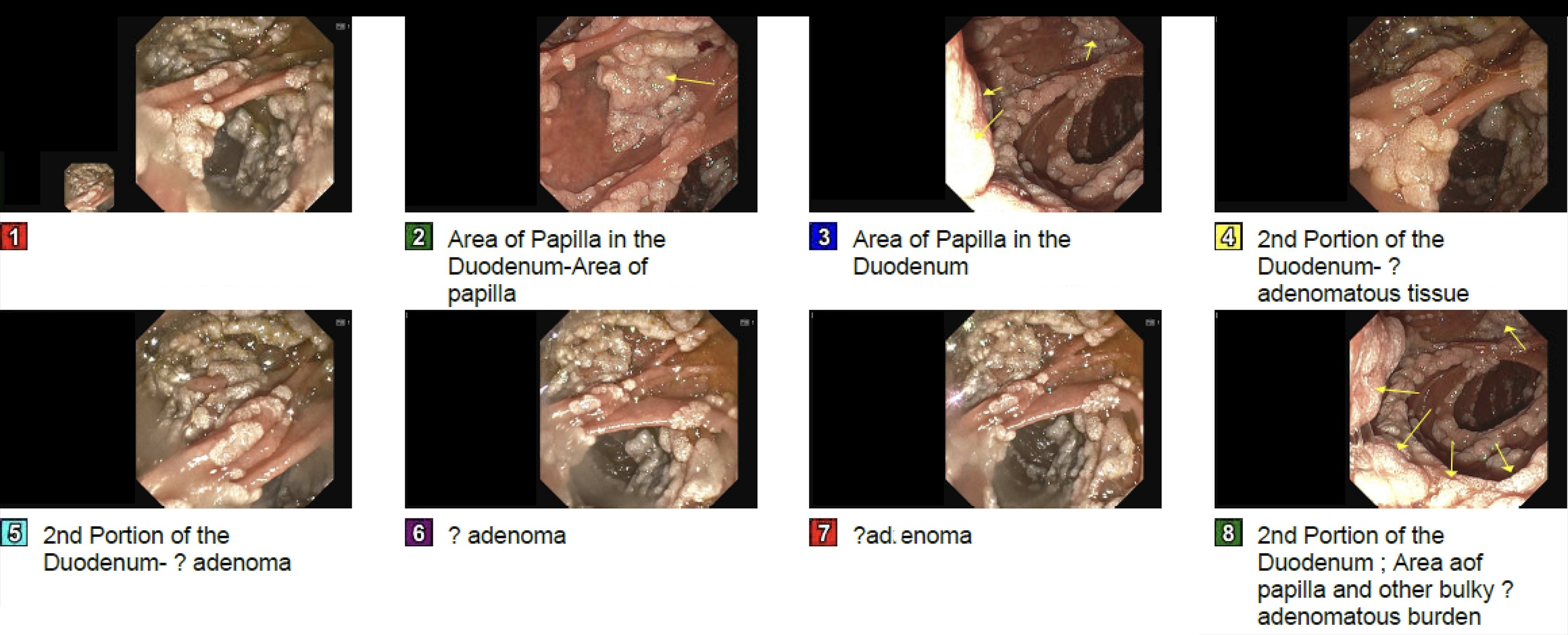
Figure: Endoscopic views of the duodenum demonstrating multiple adenomatous polyps in a patient with Familial Adenomatous Polyposis (FAP)
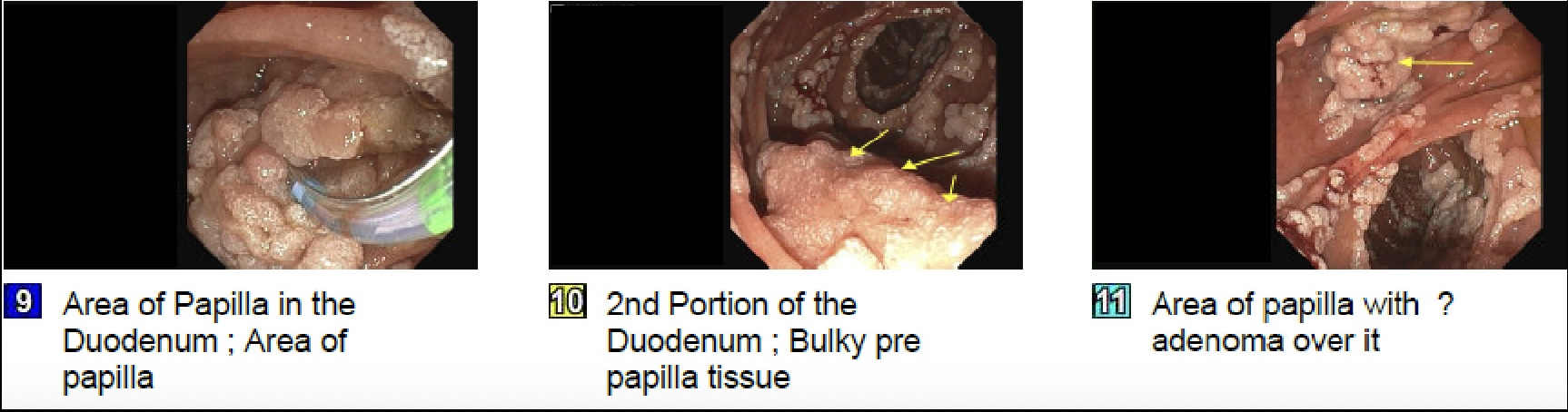
Figure: Additional endoscopic views demonstrating extensive adenomatous involvement
Disclosures:
Garvita Singhal indicated no relevant financial relationships.
Craig Gross indicated no relevant financial relationships.
Karen Drenner indicated no relevant financial relationships.
Garvita Singhal, MD, Craig Gross, MD, Karen Drenner, NP. P1953 - The Hidden Burden: Incidentally Uncovered Extensive Duodenal Polyposis Presenting as Postoperative Biliary Complication in Familial Adenomatous Polyposis (FAP), ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
Tucson Medical Center (TMC), Tucson, AZ
Introduction: Familial adenomatous polyposis (FAP) is an autosomal dominant colorectal cancer syndrome marked by early-onset colorectal polyps and near-certain cancer risk without prophylactic colectomy. As patients live longer post-colectomy, extracolonic manifestations—particularly duodenal and periampullary adenomas—have emerged as major sources of morbidity and mortality. Up to 90% of FAP patients develop duodenal polyps, with potential progression to adenocarcinoma. We present a case of extensive duodenal polyposis discovered incidentally after a postoperative complication, highlighting missed surveillance and questioning current screening paradigms.
Case Description/
Methods: A 70-year-old woman with FAP and prior near-total colectomy for colorectal cancer presented with fever, nausea, and right upper quadrant pain. Imaging showed acute cholecystitis. She underwent laparoscopic cholecystectomy, converted to open due to adhesions. Postoperatively, she developed bilious output in closed suction surgical drain and small bowel obstruction. ERCP was attempted for presumed bile leak but was aborted upon encountering extensive, carpet-like duodenal polyposis involving the bulb, second/third portions and likely further. The ampulla of Vater could not be visualized due to adenomatous overgrowth. Biopsies revealed tubular adenomas. No EUS was available. The patient had not undergone upper GI surveillance since her colectomy. She was referred to a tertiary center for EUS and hepatobiliary evaluation. Pancreaticoduodenectomy is under consideration given the extent and malignant potential of polyposis.
Discussion: This case underscores a silent yet serious complication of FAP—advanced duodenal polyposis discovered only due to a surgical complication. While duodenal adenomas are common in FAP, carpet-like polyposis is rare and typically indicates advanced disease with high malignant risk. Though Spigelman staging remains the primary risk stratification tool, emerging data suggest limited sensitivity, particularly for ampullary or deeply infiltrative lesions. This case exemplifies the need for lifelong, structured surveillance in FAP patients, especially as they age. Alarmingly, the patient never underwent germline APC testing; her mother and maternal grandmother, both with FAP, were also untested. This underscores gaps in genetic counseling and cascade testing. Clinicians must prioritize sustained follow-up, patient education, and family-based screening to prevent delayed diagnosis of serious extracolonic disease.
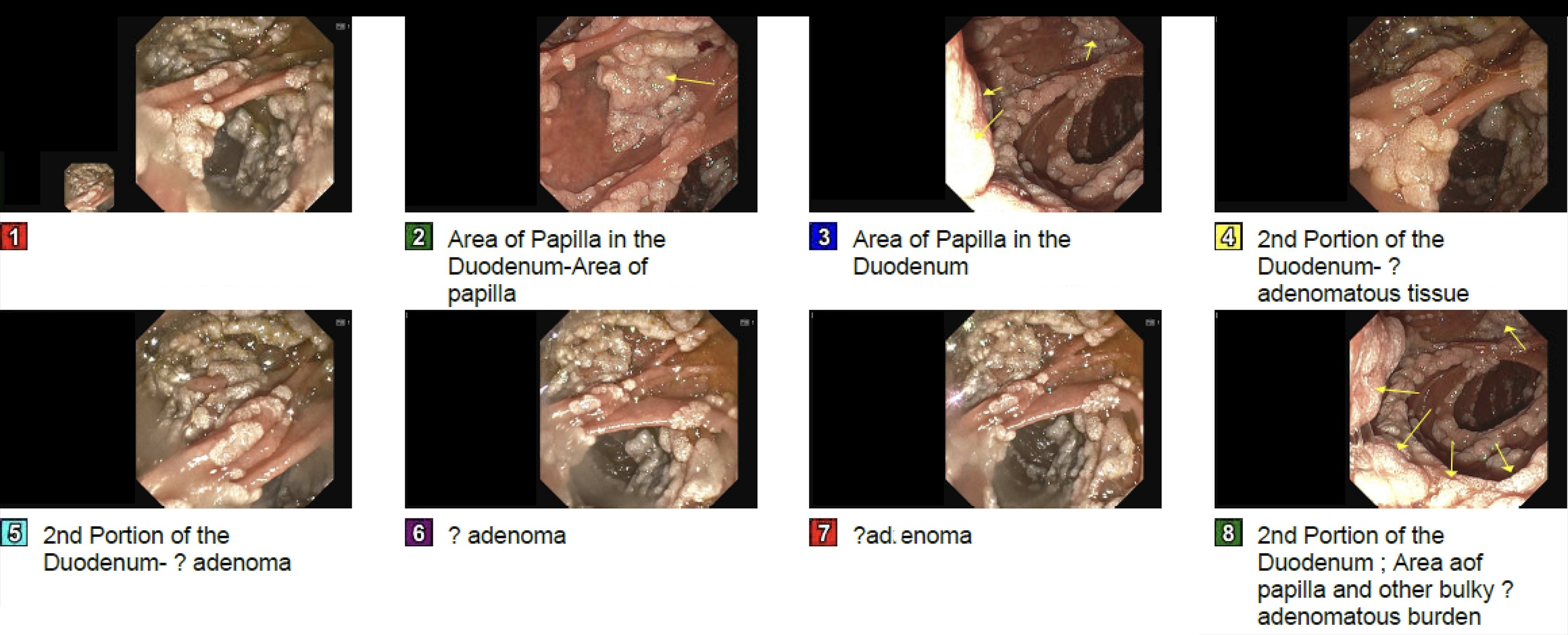
Figure: Endoscopic views of the duodenum demonstrating multiple adenomatous polyps in a patient with Familial Adenomatous Polyposis (FAP)
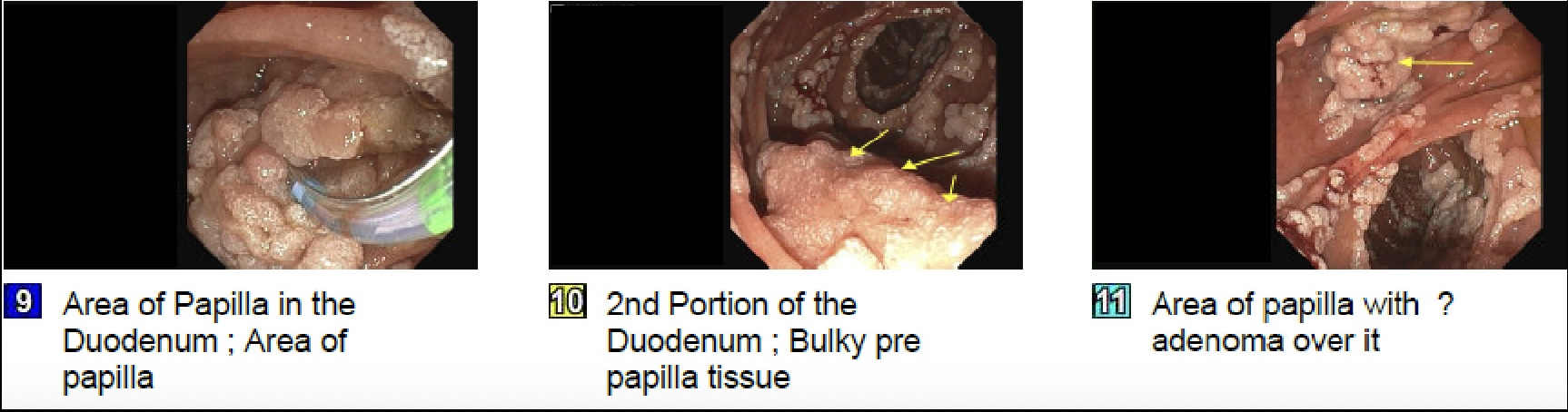
Figure: Additional endoscopic views demonstrating extensive adenomatous involvement
Disclosures:
Garvita Singhal indicated no relevant financial relationships.
Craig Gross indicated no relevant financial relationships.
Karen Drenner indicated no relevant financial relationships.
Garvita Singhal, MD, Craig Gross, MD, Karen Drenner, NP. P1953 - The Hidden Burden: Incidentally Uncovered Extensive Duodenal Polyposis Presenting as Postoperative Biliary Complication in Familial Adenomatous Polyposis (FAP), ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
